中国全科医学 ›› 2023, Vol. 26 ›› Issue (13): 1605-1612.DOI: 10.12114/j.issn.1007-9572.2022.0781
所属专题: 社区卫生服务最新研究合辑; 老年人群健康最新文章合辑; 用药最新文章合辑; 老年人合理用药专题研究; 老年问题最新文章合辑
收稿日期:2022-10-28
修回日期:2023-02-18
出版日期:2023-05-05
发布日期:2023-02-23
通讯作者:
孔令娜
基金资助:
LUO Yachan1, KONG Lingna2,*( ), LYU Qiong3, YAO Haiyan4
), LYU Qiong3, YAO Haiyan4
Received:2022-10-28
Revised:2023-02-18
Published:2023-05-05
Online:2023-02-23
Contact:
KONG Lingna
摘要: 背景 随着人口老龄化程度日益加深,老年人多病共存和多重用药现象明显增加,易发生潜在不适当用药。潜在不适当用药与不良健康结局相关。 目的 系统评价中国社区老年人潜在不适当用药发生率及相关因素,旨在为制定干预策略提供依据。 方法 于2022年6月,检索中国知网、维普中文科技期刊全文数据库、万方数据知识服务平台、中国生物医学文献数据库、PubMed、EmBase和Web of Science,获取有关中国社区老年人潜在不适当用药发生率及相关因素的文献,检索时限均为建库至2022年6月。由2名研究者独立筛选文献、提取数据后,采用美国卫生保健质量和研究机构推荐的横断面研究质量评价工具评价文献质量。采用Stata 12.0软件进行Meta分析。 结果 共纳入24篇文献,其中2篇文献质量为高,22篇文献质量中等。Meta分析结果显示,中国社区老年人潜在不适当用药发生率为34.8%〔95%CI(31.3%,38.3%)〕,其发生潜在不适当用药的相关因素有年龄≥75岁〔OR(95%CI)=1.261(1.074,1.481)〕、合并多病(≥5种)〔OR(95%CI)=3.287(1.405,7.691)〕、用药数量≥5种〔OR(95%CI)=1.800(1.305,2.481)〕和用药数量≥10种〔OR(95%CI)=4.380(2.612,7.347)〕。 结论 中国社区老年人潜在不适当用药发生率较高,高龄、合并多病、用药数量多是社区老年人发生潜在不适当用药的危险因素,应重视对具有上述特征的社区老年人群潜在不适当用药的预防和干预管理。
| 步骤 | 策略 |
|---|---|
| #1 | ("inappropriate prescribing"[MeSH Terms]OR "medication error*"[MeSH Terms])OR("inappropriate prescribing"[Title/Abstract]OR "inappropriate prescription*"[Title/Abstract]OR "inappropriate medication*"[Title/Abstract]OR "inappropriate medicine*"[Title/Abstract]OR "inappropriate drug*"[Title/Abstract]OR "irrational prescribing*"[Title/Abstract]OR "irrational prescription*"[Title/Abstract]OR "high risk prescription*"[Title/Abstract]OR "high risk medication*"[Title/Abstract]OR "unsafe prescribing"[Title/Abstract]OR "unsafe medication*"[Title/Abstract]OR "harmful medication*"[Title/Abstract]OR "harmful drug*"[Title/Abstract]OR "suboptimal prescribing"[Title/Abstract]OR "suboptimal medication*"[Title/Abstract]OR "overprescribing"[Title/Abstract]OR "over-prescribing"[Title/Abstract]OR "over-prescription"[Title/Abstract]OR "prescription drug misuse"[Title/Abstract]OR "deprescrib*"[Title/Abstract]OR "prescribing patterns"[Title/Abstract]) |
| #2 | ("primary health care"[MeSH Terms]OR "general practice"[MeSH Terms]OR "general practitioners"[MeSH Terms] OR "family practice"[MeSH Terms]OR "community health centers"[MeSH Terms]OR "community health services"[MeSH Terms]OR "physicians,family"[MeSH Terms] OR "hospitals,community"[MeSH Terms])OR("family physicians"[Title/Abstract]OR "family practice*"[Title/Abstract]OR "general practice*"[Title/Abstract]OR "general practitioner*"[Title/Abstract]OR "primary care"[Title/Abstract]OR "primary health care"[Title/Abstract]OR "primary medical care"[Title/Abstract]OR "community*"[Title/Abstract]OR "home*"[Title/Abstract]OR "general population"[Title/Abstract]OR "health station"[Title/Abstract]) |
| #3 | ("aged"[MeSH Terms])OR("elder*"[Title/Abstract] OR "older*"[Title/Abstract]OR "senior*"[Title/Abstract] OR "aging"[Title/Abstract]OR "ageing"[Title/Abstract]OR "aged"[Title/Abstract]OR "geriatric"[Title/Abstract]) |
| #4 | "China"[All Fields]OR"Chinese"[All Fields]OR"China"[MeSH Terms] |
| #5 | #1 AND #2 AND #3 AND #4 |
表1 PubMed检索策略
Table 1 Strategy for searching in PubMed
| 步骤 | 策略 |
|---|---|
| #1 | ("inappropriate prescribing"[MeSH Terms]OR "medication error*"[MeSH Terms])OR("inappropriate prescribing"[Title/Abstract]OR "inappropriate prescription*"[Title/Abstract]OR "inappropriate medication*"[Title/Abstract]OR "inappropriate medicine*"[Title/Abstract]OR "inappropriate drug*"[Title/Abstract]OR "irrational prescribing*"[Title/Abstract]OR "irrational prescription*"[Title/Abstract]OR "high risk prescription*"[Title/Abstract]OR "high risk medication*"[Title/Abstract]OR "unsafe prescribing"[Title/Abstract]OR "unsafe medication*"[Title/Abstract]OR "harmful medication*"[Title/Abstract]OR "harmful drug*"[Title/Abstract]OR "suboptimal prescribing"[Title/Abstract]OR "suboptimal medication*"[Title/Abstract]OR "overprescribing"[Title/Abstract]OR "over-prescribing"[Title/Abstract]OR "over-prescription"[Title/Abstract]OR "prescription drug misuse"[Title/Abstract]OR "deprescrib*"[Title/Abstract]OR "prescribing patterns"[Title/Abstract]) |
| #2 | ("primary health care"[MeSH Terms]OR "general practice"[MeSH Terms]OR "general practitioners"[MeSH Terms] OR "family practice"[MeSH Terms]OR "community health centers"[MeSH Terms]OR "community health services"[MeSH Terms]OR "physicians,family"[MeSH Terms] OR "hospitals,community"[MeSH Terms])OR("family physicians"[Title/Abstract]OR "family practice*"[Title/Abstract]OR "general practice*"[Title/Abstract]OR "general practitioner*"[Title/Abstract]OR "primary care"[Title/Abstract]OR "primary health care"[Title/Abstract]OR "primary medical care"[Title/Abstract]OR "community*"[Title/Abstract]OR "home*"[Title/Abstract]OR "general population"[Title/Abstract]OR "health station"[Title/Abstract]) |
| #3 | ("aged"[MeSH Terms])OR("elder*"[Title/Abstract] OR "older*"[Title/Abstract]OR "senior*"[Title/Abstract] OR "aging"[Title/Abstract]OR "ageing"[Title/Abstract]OR "aged"[Title/Abstract]OR "geriatric"[Title/Abstract]) |
| #4 | "China"[All Fields]OR"Chinese"[All Fields]OR"China"[MeSH Terms] |
| #5 | #1 AND #2 AND #3 AND #4 |
| 作者 | 发表年份(年) | 研究类型 | 地区 | 样本量 | 年龄(岁) | 样本中男性占比(%) | PIM评估工具 | PIM发生率(%) | PIM相关因素 |
|---|---|---|---|---|---|---|---|---|---|
| 赵欢等[ | 2012 | 横断面研究 | 河北省 | 416 | ≥60 | 50.2 | Beers标准(2003版) | 14.7 | — |
| 李旭琴等[ | 2015 | 横断面研究 | 上海市 | 398 | 60~75 | 44.2 | Beers标准(2012版) | 37.7 | — |
| 杨楠等[ | 2016 | 横断面研究 | 上海市 | 6 002 | 60~97 | 40.1 | Beers标准(2012版) | 16.0 | ⑦ |
| 杨晓欧等[ | 2017 | 横断面研究 | 北京市 | 216 | 65~89 | 41.2 | Beers标准(2015版) STOPP标准(2014版) | 26.4 33.8 | — |
| 陈张勇等[ | 2018 | 横断面研究 | 北京市 | 795 | 65~103 | 49.2 | Beers标准(2015版) STOPP标准(2014版) 中国PIM标准(2015版) | 25.4 18.5 28.9 | — |
| 栗芳等[ | 2018 | 横断面研究 | 北京市 | 332 | 65~80 | 56.6 | Beers标准(2015版) | 17.5 | — |
| 唐志华[ | 2018 | 横断面研究 | 浙江省 | 300 | ≥60 | 32.7 | Beers标准(2015版) | 36.3 | — |
| 刘葳等[ | 2020 | 横断面研究 | 上海市 | 360 | 65~96 | 50.3 | Beers标准(2015版) STOPP标准(2014版) | 15.8 22.2 | ①、②、③、④、⑤、⑥、⑦ |
| 刘晓瑞等[ | 2020 | 横断面研究 | 北京市 | 215 | 60~90 | 31.2 | Beers标准(2019版) 中国PIM标准(2017版) | 30.7 24.7 | — |
| 黄琦岚[ | 2020 | 横断面研究 | 山西省 | 476 | ≥60 | 43.5 | Beers标准(2015版) | 67.2 | ①、②、③、④、⑤、⑥、⑦ |
| 李雪冰等[ | 2020 | 横断面研究 | 北京市 | 264 | 62~95 | 58.3 | Beers标准(2019版) 中国PIM标准(2017版) | 39.0 28.4 | ①、②、④、⑤、⑥ |
| 章陈怡等[ | 2020 | 横断面研究 | 上海市 | 968 | ≥65 | 51.3 | Beers标准(2015版) | 32.7 | ①、②、⑥、⑦ |
| 单青等[ | 2021 | 横断面研究 | 北京市 | 562 | 65~97 | 33.3 | 中国PIM标准(2017版) | 69.6 | ①、②、③、④、⑦ |
| 顾乐乐等[ | 2021 | 横断面研究 | 上海市 | 300 | 61~88 | 52.3 | 中国PIM标准(2017版) | 19.3 | ①、②、⑥、⑦ |
| 杜琳娜[ | 2021 | 横断面研究 | 陕西省 | 319 | ≥60 | 40.4 | 中国PIM标准(2017版) | 58.0 | ①、②、③、④、⑤ |
| 周茜等[ | 2021 | 横断面研究 | 青海省 | 530 | ≥65 | 53.8 | STOPP标准(2014版) | 32.6 | ①、②、④、⑤、⑥、⑦ |
| 栗芳等[ | 2022 | 横断面研究 | 北京市 | 943 | 60~79 | 48.5 | 中国PIM标准(2017版) | 31.3 | — |
| 耿佳音等[ | 2022 | 横断面研究 | 北京市 | 815 | ≥60 | 37.4 | Beers标准(2019版) 中国PIM标准(2017版) | 32.6 22.3 | ①、②、⑥、⑦ |
| 田艳等[ | 2022 | 横断面研究 | 北京市 | 312 | 65~93 | 42.8 | STOPP标准(2014版) 中国PIM标准(2017版) | 35.9 29.7 | ①、②、④、⑥、⑦ |
| 王思蒙[ | 2022 | 横断面研究 | 安徽省 | 422 | 62~101 | 46.2 | 中国PIM标准(2017版) | 64.0 | — |
| HUANG等[ | 2020 | 横断面研究 | 湖南省 | 1 874 | 65~102 | 80.0 | Beers标准(2019版) 中国PIM标准(2017版) | 35.0 50.6 | ①、②、⑥、⑦ |
| LI等[ | 2021 | 横断面研究 | 江苏省 | 8 235 | 65~103 | 51.9 | Beers标准(2019版) 中国PIM标准(2017版) | 32.2 37.1 | ①、②、⑥、⑦ |
| SU等[ | 2022 | 横断面研究 | 北京市 | 506 214 | 65~105 | 49.9 | Beers标准(2015版) | 38.1 | ①、② |
| ZENG等[ | 2022 | 横断面研究 | 北京市 | 508 | ≥65 | 46.7 | Beers标准(2015版) Beers标准(2019版) STOPP标准(2014版) | 34.7 42.5 73.2 | ①、②、③、④、⑤、⑥、⑦ |
表2 纳入文献基本特征
Table 2 Basic characteristics of included studies
| 作者 | 发表年份(年) | 研究类型 | 地区 | 样本量 | 年龄(岁) | 样本中男性占比(%) | PIM评估工具 | PIM发生率(%) | PIM相关因素 |
|---|---|---|---|---|---|---|---|---|---|
| 赵欢等[ | 2012 | 横断面研究 | 河北省 | 416 | ≥60 | 50.2 | Beers标准(2003版) | 14.7 | — |
| 李旭琴等[ | 2015 | 横断面研究 | 上海市 | 398 | 60~75 | 44.2 | Beers标准(2012版) | 37.7 | — |
| 杨楠等[ | 2016 | 横断面研究 | 上海市 | 6 002 | 60~97 | 40.1 | Beers标准(2012版) | 16.0 | ⑦ |
| 杨晓欧等[ | 2017 | 横断面研究 | 北京市 | 216 | 65~89 | 41.2 | Beers标准(2015版) STOPP标准(2014版) | 26.4 33.8 | — |
| 陈张勇等[ | 2018 | 横断面研究 | 北京市 | 795 | 65~103 | 49.2 | Beers标准(2015版) STOPP标准(2014版) 中国PIM标准(2015版) | 25.4 18.5 28.9 | — |
| 栗芳等[ | 2018 | 横断面研究 | 北京市 | 332 | 65~80 | 56.6 | Beers标准(2015版) | 17.5 | — |
| 唐志华[ | 2018 | 横断面研究 | 浙江省 | 300 | ≥60 | 32.7 | Beers标准(2015版) | 36.3 | — |
| 刘葳等[ | 2020 | 横断面研究 | 上海市 | 360 | 65~96 | 50.3 | Beers标准(2015版) STOPP标准(2014版) | 15.8 22.2 | ①、②、③、④、⑤、⑥、⑦ |
| 刘晓瑞等[ | 2020 | 横断面研究 | 北京市 | 215 | 60~90 | 31.2 | Beers标准(2019版) 中国PIM标准(2017版) | 30.7 24.7 | — |
| 黄琦岚[ | 2020 | 横断面研究 | 山西省 | 476 | ≥60 | 43.5 | Beers标准(2015版) | 67.2 | ①、②、③、④、⑤、⑥、⑦ |
| 李雪冰等[ | 2020 | 横断面研究 | 北京市 | 264 | 62~95 | 58.3 | Beers标准(2019版) 中国PIM标准(2017版) | 39.0 28.4 | ①、②、④、⑤、⑥ |
| 章陈怡等[ | 2020 | 横断面研究 | 上海市 | 968 | ≥65 | 51.3 | Beers标准(2015版) | 32.7 | ①、②、⑥、⑦ |
| 单青等[ | 2021 | 横断面研究 | 北京市 | 562 | 65~97 | 33.3 | 中国PIM标准(2017版) | 69.6 | ①、②、③、④、⑦ |
| 顾乐乐等[ | 2021 | 横断面研究 | 上海市 | 300 | 61~88 | 52.3 | 中国PIM标准(2017版) | 19.3 | ①、②、⑥、⑦ |
| 杜琳娜[ | 2021 | 横断面研究 | 陕西省 | 319 | ≥60 | 40.4 | 中国PIM标准(2017版) | 58.0 | ①、②、③、④、⑤ |
| 周茜等[ | 2021 | 横断面研究 | 青海省 | 530 | ≥65 | 53.8 | STOPP标准(2014版) | 32.6 | ①、②、④、⑤、⑥、⑦ |
| 栗芳等[ | 2022 | 横断面研究 | 北京市 | 943 | 60~79 | 48.5 | 中国PIM标准(2017版) | 31.3 | — |
| 耿佳音等[ | 2022 | 横断面研究 | 北京市 | 815 | ≥60 | 37.4 | Beers标准(2019版) 中国PIM标准(2017版) | 32.6 22.3 | ①、②、⑥、⑦ |
| 田艳等[ | 2022 | 横断面研究 | 北京市 | 312 | 65~93 | 42.8 | STOPP标准(2014版) 中国PIM标准(2017版) | 35.9 29.7 | ①、②、④、⑥、⑦ |
| 王思蒙[ | 2022 | 横断面研究 | 安徽省 | 422 | 62~101 | 46.2 | 中国PIM标准(2017版) | 64.0 | — |
| HUANG等[ | 2020 | 横断面研究 | 湖南省 | 1 874 | 65~102 | 80.0 | Beers标准(2019版) 中国PIM标准(2017版) | 35.0 50.6 | ①、②、⑥、⑦ |
| LI等[ | 2021 | 横断面研究 | 江苏省 | 8 235 | 65~103 | 51.9 | Beers标准(2019版) 中国PIM标准(2017版) | 32.2 37.1 | ①、②、⑥、⑦ |
| SU等[ | 2022 | 横断面研究 | 北京市 | 506 214 | 65~105 | 49.9 | Beers标准(2015版) | 38.1 | ①、② |
| ZENG等[ | 2022 | 横断面研究 | 北京市 | 508 | ≥65 | 46.7 | Beers标准(2015版) Beers标准(2019版) STOPP标准(2014版) | 34.7 42.5 73.2 | ①、②、③、④、⑤、⑥、⑦ |
| 作者 | ① | ② | ③ | ④ | ⑤ | ⑥ | ⑦ | ⑧ | ⑨ | ⑩ | ⑪ | 总分(分) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 赵欢等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 李旭琴等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 杨楠等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 杨晓欧等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 陈张勇等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 栗芳等[ | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 5 |
| 唐志华[ | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 7 |
| 刘葳等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 刘晓瑞等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 黄琦岚[ | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 7 |
| 李雪冰等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 章陈怡等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 单青等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 顾乐乐等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 杜琳娜[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 周茜等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 栗芳等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 耿佳音等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 田艳等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 王思蒙[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| HUANG等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| LI等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| SU等[ | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 8 |
| ZENG等[ | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 8 |
表3 纳入研究质量评价结果
Table 3 Risk of bias assessment of included studies
| 作者 | ① | ② | ③ | ④ | ⑤ | ⑥ | ⑦ | ⑧ | ⑨ | ⑩ | ⑪ | 总分(分) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 赵欢等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 李旭琴等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 杨楠等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 杨晓欧等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 陈张勇等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 栗芳等[ | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 5 |
| 唐志华[ | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 7 |
| 刘葳等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 刘晓瑞等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 黄琦岚[ | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 7 |
| 李雪冰等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 章陈怡等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 单青等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 顾乐乐等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 杜琳娜[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 周茜等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 栗芳等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 耿佳音等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 田艳等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 王思蒙[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| HUANG等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| LI等[ | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| SU等[ | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 8 |
| ZENG等[ | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 8 |
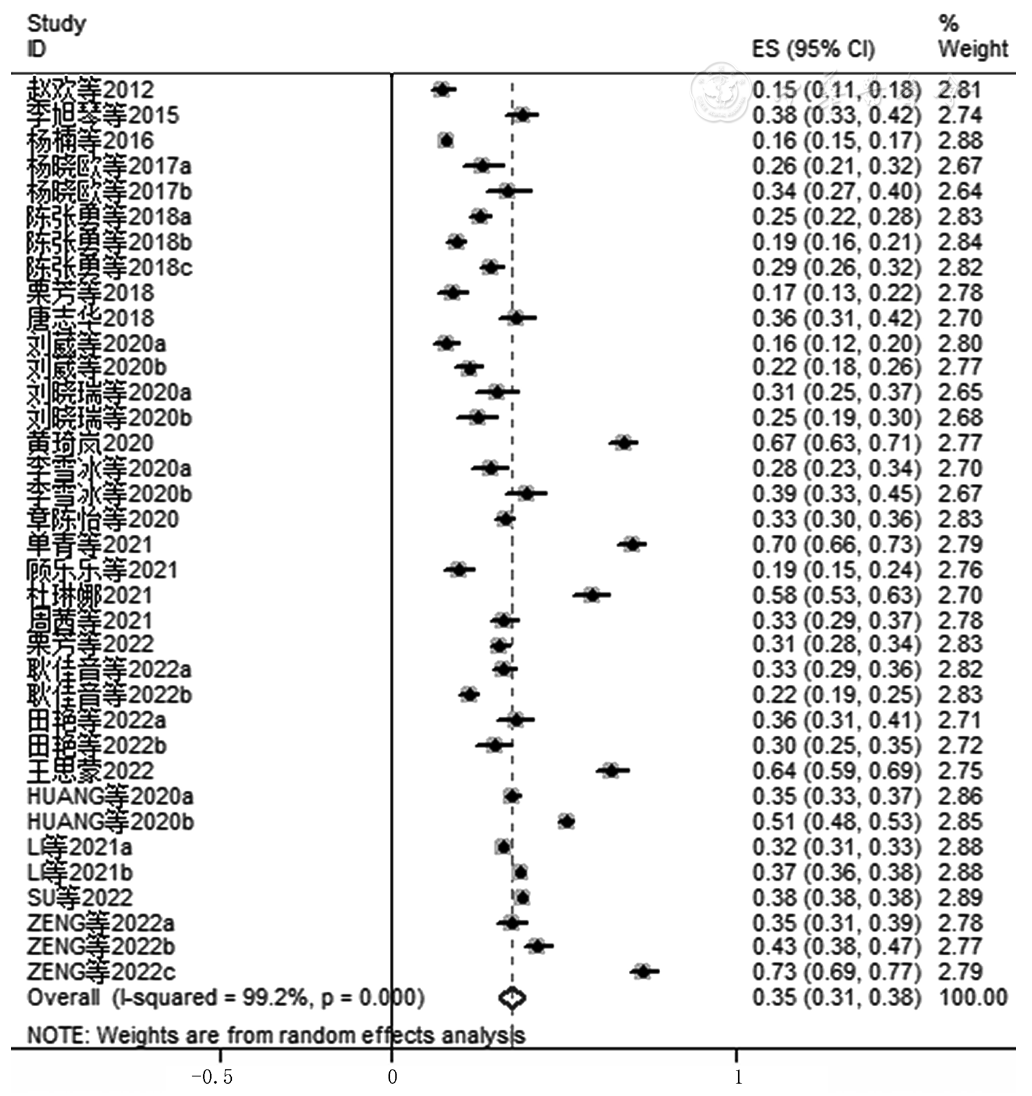
图2 中国社区老年人潜在不适当用药率Meta分析森林图注:a表示从同一研究中提取的第1组社区老年人PIM发生率数据,b表示从同一研究中提取的第2组社区老年人PIM发生率数据,c表示从同一研究中提取的第3组社区老年人PIM发生率数据
Figure 2 Forest plot of the pooled prevalence of potentially inappropriate medication in community-dwelling Chinese older adults
| 亚组 | 纳入研究数(项) | 异质性检验 | 效应模型 | PIM发生率(95%CI)(%) | |
|---|---|---|---|---|---|
| P值 | I2(%) | ||||
| 评估工具 | |||||
| Beers标准 | 17[ | <0.001 | 99.4 | 随机 | 31.9(26.7,37.1) |
| 中国PIM标准 | 12[ | <0.001 | 98.7 | 随机 | 38.7(31.1,46.3) |
| STOPP标准 | 6[ | <0.001 | 99.1 | 随机 | 36.0(18.4,53.7) |
| 样本中男性占比(%) | |||||
| <50 | 15[ | <0.001 | 99.4 | 随机 | 38.1(32.4,43.9) |
| ≥50 | 9[ | <0.001 | 98.0 | 随机 | 29.1(24.4,33.8) |
| 地理区域 | |||||
| 北方 | 15[ | <0.001 | 98.6 | 随机 | 35.6(30.8,40.5) |
| 南方 | 9[ | <0.001 | 99.4 | 随机 | 33.2(26.3,40.1) |
| 文献发表时间(年) | |||||
| 2012—2019 | 7[ | <0.001 | 96.0 | 随机 | 25.2(20.4,30.1) |
| 2020—2022 | 17[ | <0.001 | 98.5 | 随机 | 38.4(35.3,41.6) |
表4 中国社区老年人PIM发生率的亚组分析
Table 4 Subgroup analysis of the prevalence of potentially inappropriate medication in community-dwelling Chinese older adults
| 亚组 | 纳入研究数(项) | 异质性检验 | 效应模型 | PIM发生率(95%CI)(%) | |
|---|---|---|---|---|---|
| P值 | I2(%) | ||||
| 评估工具 | |||||
| Beers标准 | 17[ | <0.001 | 99.4 | 随机 | 31.9(26.7,37.1) |
| 中国PIM标准 | 12[ | <0.001 | 98.7 | 随机 | 38.7(31.1,46.3) |
| STOPP标准 | 6[ | <0.001 | 99.1 | 随机 | 36.0(18.4,53.7) |
| 样本中男性占比(%) | |||||
| <50 | 15[ | <0.001 | 99.4 | 随机 | 38.1(32.4,43.9) |
| ≥50 | 9[ | <0.001 | 98.0 | 随机 | 29.1(24.4,33.8) |
| 地理区域 | |||||
| 北方 | 15[ | <0.001 | 98.6 | 随机 | 35.6(30.8,40.5) |
| 南方 | 9[ | <0.001 | 99.4 | 随机 | 33.2(26.3,40.1) |
| 文献发表时间(年) | |||||
| 2012—2019 | 7[ | <0.001 | 96.0 | 随机 | 25.2(20.4,30.1) |
| 2020—2022 | 17[ | <0.001 | 98.5 | 随机 | 38.4(35.3,41.6) |
| 项目 | 纳入研究数(项) | 异质性检验 | 效应模型 | OR (95%CI) | Z值 | P值 | |
|---|---|---|---|---|---|---|---|
| P值 | I2(%) | ||||||
| 性别男 | 11[ | 0.301 | 13.9 | 固定 | 0.986(0.936,1.039) | 0.53 | 0.599 |
| 年龄≥75岁 | 6[ | <0.001 | 78.6 | 随机 | 1.261(1.074,1.481) | 2.84 | 0.005 |
| 有配偶 | 4[ | 0.524 | 0 | 固定 | 0.921(0.788,1.076) | 1.04 | 0.297 |
| 文化程度为初中及以下 | 6[ | 0.287 | 18.8 | 固定 | 1.060(0.926,1.214) | 0.84 | 0.399 |
| 独居 | 5[ | 0.932 | 0 | 固定 | 1.114(0.862,1.441) | 0.83 | 0.408 |
| 合并多病(≥5种) | 3[ | <0.001 | 92.6 | 随机 | 3.287(1.405,7.691) | 2.74 | 0.006 |
| 用药数量≥5种 | 7[ | <0.001 | 95.7 | 随机 | 1.800(1.305,2.481) | 3.59 | <0.001 |
| 用药数量≥10种 | 4[ | 0.006 | 76.1 | 随机 | 4.380(2.612,7.347) | 5.60 | <0.001 |
表5 中国社区老年人潜在不适当用药发生相关因素的Meta分析
Table 5 Meta-analysis of associated factors of potentially inappropriate medication in community-dwelling Chinese older adults
| 项目 | 纳入研究数(项) | 异质性检验 | 效应模型 | OR (95%CI) | Z值 | P值 | |
|---|---|---|---|---|---|---|---|
| P值 | I2(%) | ||||||
| 性别男 | 11[ | 0.301 | 13.9 | 固定 | 0.986(0.936,1.039) | 0.53 | 0.599 |
| 年龄≥75岁 | 6[ | <0.001 | 78.6 | 随机 | 1.261(1.074,1.481) | 2.84 | 0.005 |
| 有配偶 | 4[ | 0.524 | 0 | 固定 | 0.921(0.788,1.076) | 1.04 | 0.297 |
| 文化程度为初中及以下 | 6[ | 0.287 | 18.8 | 固定 | 1.060(0.926,1.214) | 0.84 | 0.399 |
| 独居 | 5[ | 0.932 | 0 | 固定 | 1.114(0.862,1.441) | 0.83 | 0.408 |
| 合并多病(≥5种) | 3[ | <0.001 | 92.6 | 随机 | 3.287(1.405,7.691) | 2.74 | 0.006 |
| 用药数量≥5种 | 7[ | <0.001 | 95.7 | 随机 | 1.800(1.305,2.481) | 3.59 | <0.001 |
| 用药数量≥10种 | 4[ | 0.006 | 76.1 | 随机 | 4.380(2.612,7.347) | 5.60 | <0.001 |
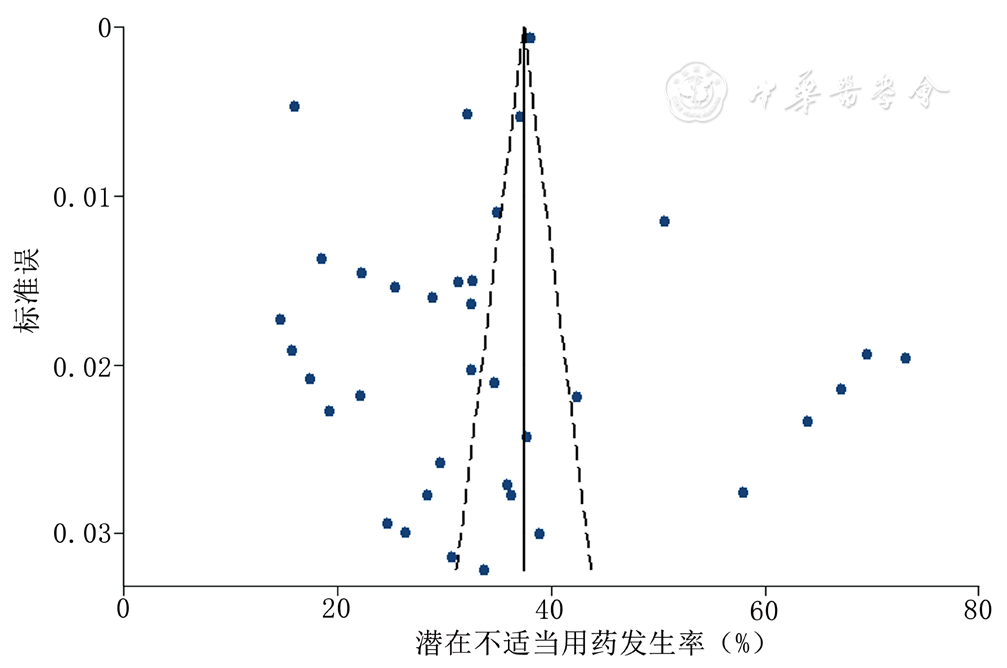
图3 中国社区老年人潜在不适当用药发生率的漏斗图
Figure 3 Funnel plot of studies on prevalence of potentially inappropriate medication in community-dwelling Chinese older adults
| [1] |
|
| [2] |
王思蒙,张晨,孙雪,等. 社区老年人潜在不适当用药及其应对模式的研究进展[J]. 中国全科医学,2022,25(13):1551-1556. DOI:10.12114/j.issn.1007-9572.2022.0077.
|
| [3] |
迟俊婷,牛晓丹,阮海慧,等. 潜在不适当用药对老年人不良健康结局影响的系统评价[J]. 中华护理教育,2020,17(3):268-274. DOI:10.3761/j.issn.1672-9234.2020.03.017.
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
曾宪涛,刘慧,陈曦,等. Meta分析系列之四:观察性研究的质量评价工具[J]. 中国循证心血管医学杂志,2012,4(4):297-299. DOI:10.3969/j.1674-4055.2012.04.004.
|
| [8] |
朱洁云,高敏,宋秋韵,等. 中国老年人骨质疏松症患病率的Meta分析[J]. 中国全科医学,2022,25(3):346-353. DOI:10.12114/j.issn.1007-9572.2021.02.083.
|
| [9] |
赵欢,薛鹏,刘建秋,等. 基于Beers准则的社区老年慢性病患者潜在性不适当用药调查分析[J]. 中国农村卫生事业管理,2012,32(3):241-243.
|
| [10] |
李旭琴,杨惠赟,毛凤飞,等. 新版Beers标准评价社区多病种慢性病老年患者潜在性不适当用药的探索[J]. 世界临床药物,2015,36(9):618-622. DOI:10.13683/j.wph.2015.09.010.
|
| [11] |
杨楠,管璐艳,郑晓栋,等. 真如社区老年高血压合并糖尿病患者多重用药现状调查[J]. 药物流行病学杂志,2016,25(5):306-308.
|
| [12] |
杨晓欧,庄宁,张琳,等. Beers标准和STOPP标准在社区老年患者潜在不适当用药中的评估作用[J]. 临床合理用药杂志,2017,10(21):95-97.
|
| [13] |
陈张勇,刘利刚,吐达洪,等. 基于3种标准的社区老年患者潜在不适当用药评估[J]. 中国新药与临床杂志,2018,37(12):700-706. DOI:10.14109/j.cnki.xyylc.2018.12.009.
|
| [14] |
栗芳,王思铮,石志华,等. 基于2015版Beers标准的社区老年患者用药问题分析[J]. 中国新药与临床杂志,2018,37(3):173-176. DOI:10.14109/j.cnki.xyylc.2018.03.012.
|
| [15] |
唐志华. 社区独居与非独居老人不合理用药现状及影响因素比较研究[D]. 杭州:浙江大学,2018.
|
| [16] |
刘葳,于德华,金花,等. 社区老年多病共存患者多重用药情况评价研究[J]. 中国全科医学,2020,23(13):1592-1598. DOI:10.12114/j.issn.1007-9572.2020.00.026.
|
| [17] |
刘晓瑞,郭桂芳. 北京市社区老年人潜在不适当用药的调查分析[J]. 解放军护理杂志,2020,37(5):30-34. DOI:10.3969/j.issn.1008-9993.2020.05.008.
|
| [18] |
黄琦岚. 太原市社区老年慢性病患者用药情况及生命质量评价研究[D]. 晋中:山西中医药大学,2020.
|
| [19] |
李雪冰,王鹏. 斋堂社区老年人潜在不适当用药及其相关因素[J]. 中华老年多器官疾病杂志,2020,19(5):340-344. DOI:10.11915/j.issn.1671-5403.2020.05.080.
|
| [20] |
章陈怡,潘志刚,陈实,等. 上海社区老年慢性病患者潜在不适当用药情况及影响因素[J]. 中华全科医师杂志,2020,19(4):324-328. DOI:10.3760/cma.j.cn114798-20190718-00547.
|
| [21] |
单青,胡波,陈孟莉. 社区老年人潜在不适当用药与衰弱的相关性[J]. 中华老年多器官疾病杂志,2021,20(8):581-585. DOI:10.11915/j.issn.1671-5403.2021.08.121.
|
| [22] |
顾乐乐,杨郗. 社区临床药师视角下老年高血压合并糖尿病患者合理用药现况研究[J]. 山西医药杂志,2021,50(5):706-709. DOI:10.3969/j.issn.0253-9926.2021.05.002.
|
| [23] |
杜林娜. 老年糖尿病患者潜在不恰当用药与衰弱的关系研究[D]. 西安:西安医学院,2021.
|
| [24] |
周茜,汪晓洲,白洁. 青海地区65岁以上老年群体高血压多病共存患者治疗现状调查[J]. 公共卫生与预防医学,2021,32(5):153-156. DOI:10.3969/j.issn.1006-2483.2021.05.036.
|
| [25] |
栗芳,陈张勇,吐达洪,等. 基于我国标准社区老年患者潜在不适当用药分析[J]. 临床药物治疗杂志,2022,20(6):58-62. DOI:10.3969/j.issn.1672-3384.2022.06.011.
|
| [26] |
耿佳音,黄亚芳,刘艳丽. 老年患者社区门诊潜在不适当处方影响因素分析[J]. 中国全科医学,2022,25(16):1969-1977. DOI:10.12114/j.issn.1007-9572.2022.0164.
|
| [27] |
田艳,周涛,丁林,等. 北京市东城区社区老年患者潜在不适当用药和处方遗漏问题调查分析[J]. 医药导报,2022,41(8):1207-1212. DOI:3870/j.issn.1004-0781.2022.08.022.
|
| [28] |
王思蒙. 社区老年轻度认知障碍者衰弱与其亚型分布现状及影响因素分析[D]. 湖州:湖州师范学院,2022.
|
| [29] |
|
| [30] |
|
| [31] |
|
| [32] |
|
| [33] |
|
| [34] |
|
| [35] |
侯凯旋,邢晓璇,闫素英. 中国老年门诊患者潜在不适当用药现状系统评价[J]. 临床药物治疗杂志,2017,15(11):26-30. DOI:10.3969/j.issn.1672-3384.2017.11.006.
|
| [36] |
中国老年保健医学研究会老年合理用药分会,中华医学会老年医学分会,中国药学会老年药学专业委员会,等. 中国老年人潜在不适当用药判断标准(2017年版)[J]. 药物不良反应杂志,2018,20(1):2-8. DOI:10.3760/cma.j.issn.1008-5734.2018.01.002.
|
| [37] |
舒冰,刘玉龙,姜玲. 老年人潜在不适当用药评估标准研究进展[J]. 中国医院药学杂志,2019,39(18):1905-1910. DOI:10.13286/j.cnki.chinhosppharmacyj.2019.18.20.
|
| [38] |
廖雅慧,郎驿天,林燕,等. 常用老年人潜在不适当用药判断标准比较[J]. 中国药房,2022,33(9):1131-1135. DOI:10.6039/j.issn.1001-0408.2022.09.18.
|
| [39] |
|
| [40] |
李荔,李莎,卫芸,等. 社区老年人多重用药率及其相关因素的系统综述[J]. 中国全科医学,2021,24(25):3161-3170. DOI:10.12114/j.issn.1007-9572.2021.00.204.
|
| [41] |
|
| [42] |
|
| [43] |
|
| [1] | 李玲, 李雅萍, 钱时兴, 聂婧, 陆春华, 李霞. 社区中老年人认知功能影响因素及风险预测研究[J]. 中国全科医学, 2025, 28(30): 3773-3778. |
| [2] | 许佳兰, 阎红, 文君, 周紫彤, 王思宇. 老年癌症患者潜在不适当用药发生率的Meta分析[J]. 中国全科医学, 2025, 28(30): 3815-3822. |
| [3] | 张天宇, 于海搏, 陈飞, 李新, 张佳佳, 詹晓凯, 申曼, 汤然, 范斯斌, 赵凤仪, 黄仲夏. POEMS综合征全身系统性治疗疗效和安全性的Meta分析[J]. 中国全科医学, 2025, 28(27): 3447-3455. |
| [4] | 全家霖, 朱琳, 苏煜, 陈泽恺, 陈梓淇, 张卓凡. 运动方式对超重或肥胖儿童青少年执行功能改善效果的网状Meta分析[J]. 中国全科医学, 2025, 28(27): 3422-3431. |
| [5] | 崔宇阳, 程桂荣, 曾燕, 黄招兰, 谭伟. 社区老年人婚姻状况和社会支持及生活习惯与认知障碍的关联:基于湖北老年记忆队列基线调查[J]. 中国全科医学, 2025, 28(26): 3240-3247. |
| [6] | 纪冰, 姜嘟嘟, 陈晨, 郑艳玲, 石建伟, 方力争, 杜雪平. 分级诊疗背景下带状疱疹社区全科诊疗路径构建[J]. 中国全科医学, 2025, 28(25): 3110-3118. |
| [7] | 燕芳红, 彭国恬, 张国莉, 孙瑞仪, 马玉霞, 韩琳. 医联体内老年慢性病管理内容的匹配分析:基于"指南-实践-需求"视角[J]. 中国全科医学, 2025, 28(25): 3119-3126. |
| [8] | 蒋世华, 朱政, 任盈盈, 朱垚磊, 王越, 高希彬. 中国儿童青少年近视患病率及影响因素的Meta分析[J]. 中国全科医学, 2025, 28(24): 3043-3052. |
| [9] | 李嘉欣, 刘钟桧, 谢硕, 付志方, 孙丹, 焦红梅. 分解代谢及炎症状态的生物标志物变化趋势对老年患者慢性危重症的早期预测价值研究[J]. 中国全科医学, 2025, 28(24): 2993-2999. |
| [10] | 于文华, 李建国, 段文燕, 高旭妍, 李夏夏, 张子龙, 张丽, 马丽娜. 老年人功能受损评估量表在社区老年人中的信效度检验[J]. 中国全科医学, 2025, 28(24): 3000-3004. |
| [11] | 杨晨, 陈瞳, 张利方, 张洪旭, 李鹏飞, 张雪娟. 达格列净对老年乳腺癌幸存者射血分数保留的心力衰竭合并2型糖尿病患者的预后影响研究[J]. 中国全科医学, 2025, 28(24): 3053-3058. |
| [12] | 李浩, 李江涛, 刘丹, 王建军. 贝利尤单抗和阿尼鲁单抗及泰它西普治疗系统性红斑狼疮疗效和安全性的网状Meta分析[J]. 中国全科医学, 2025, 28(23): 2924-2933. |
| [13] | 王笑林, 李秋月, 周彦君, 张金辉, 梁涛. 转移性结直肠癌患者呋喹替尼治疗相关心血管毒性发生率和风险的Meta分析[J]. 中国全科医学, 2025, 28(23): 2934-2940. |
| [14] | 陈友兰, 蓝彦琦, 吴阿华, 张海霞, 黄健康, 郭志南. "三师共管"家庭医生签约服务对老年高血压患者的健康管理效果研究[J]. 中国全科医学, 2025, 28(22): 2769-2775. |
| [15] | 赵晓晴, 郭桐桐, 张欣怡, 李林虹, 张亚, 嵇丽红, 董志伟, 高倩倩, 蔡伟芹, 郑文贵, 井淇. 社区老年人认知障碍风险预测模型的构建与验证研究[J]. 中国全科医学, 2025, 28(22): 2776-2783. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





