中国全科医学 ›› 2023, Vol. 26 ›› Issue (17): 2078-2088.DOI: 10.12114/j.issn.1007-9572.2022.0827
沈傲梅1,2, 路潜1,*( ), 符鑫1, 韦小夏1, 卞静如2, 张丽媛2, 强万敏2, 庞冬1
), 符鑫1, 韦小夏1, 卞静如2, 张丽媛2, 强万敏2, 庞冬1
收稿日期:2022-08-08
修回日期:2022-12-10
出版日期:2023-06-15
发布日期:2023-01-18
通讯作者:
路潜
基金资助:
SHEN Aomei1,2, LU Qian1,*( ), FU Xin1, WEI Xiaoxia1, BIAN Jingru2, ZHANG Liyuan2, QIANG Wanmin2, PANG Dong1
), FU Xin1, WEI Xiaoxia1, BIAN Jingru2, ZHANG Liyuan2, QIANG Wanmin2, PANG Dong1
Received:2022-08-08
Revised:2022-12-10
Published:2023-06-15
Online:2023-01-18
Contact:
LU Qian
摘要: 背景 乳腺癌相关淋巴水肿(BCRL)是困扰乳腺癌患者术后常见的慢性并发症,早期评估和预测BCRL风险尤为重要,但目前仍缺乏权威公认、适宜推广的风险预测模型。目的 本研究拟基于Meta分析构建并验证乳腺癌患者BCRL风险预测模型。方法 计算机检索PubMed、Embase、CINAHL、Scopus、Web of Science、Cochrane Library、中国知网、中国生物医学数据库、万方数据知识服务平台自建库至2021年11月发表的有关BCRL危险因素的前瞻性队列研究。由2名经过系统培训的研究者分别独立筛选文献、提取资料,并采用纽卡斯尔-渥太华量表(NOS)进行质量评价。采用Stata 17.0软件进行Meta分析。根据Meta分析结果提取合并效应量具有显著性的风险因素及合并风险值,构建Logistic回归预测模型。基于回归系数及合并风险值构建Logistic和Additive评分模型。选取2017年4月至2018年12月在北京大学人民医院乳腺中心招募的486例乳腺癌术后患者为模型验证集,采用受试者工作特征(ROC)曲线下面积(AUC)、Hosmer-Lemeshow检验评价评分模型的预测性能,采用决策曲线分析评价预测模型的临床实用性。结果 共纳入49项前瞻性队列研究、32 543例乳腺癌患者。Meta分析结果显示,乳腺癌患者BCRL发生率为20.6%〔95%CI(17.9%,23.3%)〕。49项研究中报告次数>5次且Meta分析合并效应量结果具有显著性的危险因素共5个,分别为:体质指数(BMI)〔RR=1.777,95%CI(1.515,2.085)〕、乳腺手术类型〔RR=1.320,95%CI(1.125,1.549)〕、腋窝手术类型〔RR=3.058,95%CI(2.325,4.020)〕、放疗〔RR=1.620,95%CI(1.214,2.160)〕、术后并发症〔RR=2.373,95%CI(1.278,4.405)〕。Logistic及Additive评分模型总分分别为0~34分、5~11分。Logistic及Additive评分模型的AUC分别为0.748〔95%CI(0.701,0.794)〕、0.737〔95%CI(0.691,0.784)〕,Hosmer-Lemeshow检验P值分别为0.185、0.763。Logistic评分模型最佳截断值为18分,灵敏度为81.7%,特异度为43.1%;Additive评分模型最佳截断值为8.5分,灵敏度为80.9%,特异度为42.8%。当阈值概率在20%~30%时,预测模型具有较高的临床净获益。结论 基于Meta分析构建的BCRL风险预测模型具有较好的预测性能,可作为BCRL风险评估工具,指导BCRL的分层管理,但其预测性能和临床实用性仍有待进一步验证和优化。
| 步骤 | 检索式 | 命中数量(篇) |
|---|---|---|
| #1 | "Breast Neoplasms" [Mesh] | 315 036 |
| #2 | "breast cancer" [Title/Abstract] OR "breast neoplasm*" [Title/Abstract] OR "breast tumor*" [Title/Abstract] OR "breast tumour*" [Title/Abstract] OR "Breast Carcinoma" [Title/Abstract] | 328 162 |
| #3 | #1 OR #2 | 409 101 |
| #4 | "lymphedema" [MeSH Terms] OR "Breast Cancer Lymphedema" [MeSH Terms] | 13 039 |
| #5 | "lymphoedema*" [Title/Abstract] OR "lymphedema*" [Title/Abstract] OR "lymphatic oedema*" [Title/Abstract] OR "lymphatic edema*" [Title/Abstract] OR "oedema*" [Title/Abstract] OR "edema*" [Title/Abstract] OR "arm oedema" [Title/Abstract] OR "arm edema" [Title/Abstract] OR "upper extremity oedema" [Title/Abstract] OR "upper limb oedema" [Title/Abstract] OR "upper extremity edema" [Title/Abstract] OR "upper limb edema" [Title/Abstract] OR "breast cancer lymphedema" [Title/Abstract] OR "breast cancer related lymphedema" [Title/Abstract] OR "breast cancer treatment related lymphedema" [Title/Abstract] OR "breast cancer lymphoedema" [Title/Abstract] OR "breast cancer related lymphoedema" [Title/Abstract] OR "breast cancer treatment related lymphoedema" [Title/Abstract] OR "breast cancer related arm lymphedema" [Title/Abstract] OR "lymphedemic" [Title/Abstract] OR "lymphedemic" [Title/Abstract] OR "swelling" [Title/Abstract] | 252 930 |
| #6 | #4 OR #5 | 257 765 |
| #7 | "Risk Factors" [MeSH Terms] OR "epidemiologic factors" [MeSH Terms] | 1 656 289 |
| #8 | "risk factor*" [Title/Abstract] OR "risk variable*" [Title/Abstract] OR "predictor*" [Title/Abstract] OR "prediction" [Title/Abstract] OR "predict factor*" [Title/Abstract] OR "prognostic factor*" [Title/Abstract] OR "prognostic variable*" [Title/Abstract] OR "epidemiologic factor*" [Title/Abstract] OR "epidemiologic variable*" [Title/Abstract] OR "relevant factor*" [Title/Abstract] OR "relevant variable*" [Title/Abstract] OR "related factor*" [Title/Abstract] OR "related variable*" [Title/Abstract] OR "contributing factor*" [Title/Abstract] | 1 445 977 |
| #9 | #7 OR #8 | 2 646 906 |
| #10 | #3 AND #7 AND #11 | 768 |
| #11 | #10 AND ((humans [Filter]) AND (Chinese [Filter] OR English [Filter])) | 626 |
表1 PubMed检索策略
Table 1 Strategies for searching studies about breast cancer-related lymphedema in databases of PubMed
| 步骤 | 检索式 | 命中数量(篇) |
|---|---|---|
| #1 | "Breast Neoplasms" [Mesh] | 315 036 |
| #2 | "breast cancer" [Title/Abstract] OR "breast neoplasm*" [Title/Abstract] OR "breast tumor*" [Title/Abstract] OR "breast tumour*" [Title/Abstract] OR "Breast Carcinoma" [Title/Abstract] | 328 162 |
| #3 | #1 OR #2 | 409 101 |
| #4 | "lymphedema" [MeSH Terms] OR "Breast Cancer Lymphedema" [MeSH Terms] | 13 039 |
| #5 | "lymphoedema*" [Title/Abstract] OR "lymphedema*" [Title/Abstract] OR "lymphatic oedema*" [Title/Abstract] OR "lymphatic edema*" [Title/Abstract] OR "oedema*" [Title/Abstract] OR "edema*" [Title/Abstract] OR "arm oedema" [Title/Abstract] OR "arm edema" [Title/Abstract] OR "upper extremity oedema" [Title/Abstract] OR "upper limb oedema" [Title/Abstract] OR "upper extremity edema" [Title/Abstract] OR "upper limb edema" [Title/Abstract] OR "breast cancer lymphedema" [Title/Abstract] OR "breast cancer related lymphedema" [Title/Abstract] OR "breast cancer treatment related lymphedema" [Title/Abstract] OR "breast cancer lymphoedema" [Title/Abstract] OR "breast cancer related lymphoedema" [Title/Abstract] OR "breast cancer treatment related lymphoedema" [Title/Abstract] OR "breast cancer related arm lymphedema" [Title/Abstract] OR "lymphedemic" [Title/Abstract] OR "lymphedemic" [Title/Abstract] OR "swelling" [Title/Abstract] | 252 930 |
| #6 | #4 OR #5 | 257 765 |
| #7 | "Risk Factors" [MeSH Terms] OR "epidemiologic factors" [MeSH Terms] | 1 656 289 |
| #8 | "risk factor*" [Title/Abstract] OR "risk variable*" [Title/Abstract] OR "predictor*" [Title/Abstract] OR "prediction" [Title/Abstract] OR "predict factor*" [Title/Abstract] OR "prognostic factor*" [Title/Abstract] OR "prognostic variable*" [Title/Abstract] OR "epidemiologic factor*" [Title/Abstract] OR "epidemiologic variable*" [Title/Abstract] OR "relevant factor*" [Title/Abstract] OR "relevant variable*" [Title/Abstract] OR "related factor*" [Title/Abstract] OR "related variable*" [Title/Abstract] OR "contributing factor*" [Title/Abstract] | 1 445 977 |
| #9 | #7 OR #8 | 2 646 906 |
| #10 | #3 AND #7 AND #11 | 768 |
| #11 | #10 AND ((humans [Filter]) AND (Chinese [Filter] OR English [Filter])) | 626 |
| 第一作者 | 发表时间(年) | 国家 | 样本量(例) | 年龄(岁) | 水肿例数(例) | 发生率(%) | 诊断标准 | 危险因素 |
|---|---|---|---|---|---|---|---|---|
| KUIJER[ | 2021 | 美国 | 888 | 37(22~40) | 122 | 13.7 | ① | ABC |
| KEELY[ | 2021 | 美国 | 1 100 | 56±12 | 251 | 22.8 | ② | E |
| KIM[ | 2021 | 韩国 | 910 | 腋窝淋巴结清扫(n=595):52.5±10.4;前哨淋巴结活检(n=315):51.6±10.5 | 121 | 13.3 | ③ | ABCD |
| BIDYUT[ | 2021 | 印度 | 342 | 47 | 144 | 42.1 | ① | AB |
| 佟洋[ | 2021 | 中国 | 713 | 水肿(n=61):55.17±13.26;非水肿(n=652):54.81±11.59 | 61 | 8.6 | ③ | AD |
| 袁芊芊[ | 2021 | 中国 | 312 | 48 | 45 | 14.4 | ② | AD |
| BRUNELLE[ | 2020 | 美国 | 647 | 56.6(27~83) | 64 | 9.9 | ② | ABCD |
| BRUNELLE[ | 2020 | 美国 | 1 181 | 569例≥55,612例<55 | 129 | 10.9 | ② | ABCDE |
| BUNDRED[ | 2020 | 英国 | 545 | 55.7±12.4 | 122 | 22.4 | ② | AE |
| NAOUM[ | 2020 | 美国 | 1 815 | 56(24.4,87.9) | 171 | 9.4 | ② | C |
| 王季[ | 2020 | 中国 | 472 | 水肿(n=23):55.57±13.14;非水肿(n=449):54.83±11.10 | 23 | 4.9 | ①或③ | ACD |
| ARMER[ | 2019 | 美国 | 486 | 50.1±10.8 | 284 | 58.4 | ② | AD |
| GROSS[ | 2019 | 美国 | 265 | 52.6(42.7,62.1) | 39 | 14.7 | ③ | A |
| KHANNA[ | 2019 | 印度 | 98 | 76.8%年龄41~60 | 23 | 23.5 | ③ | DE |
| GROSS[ | 2018 | 美国 | 492 | 50(40~60) | 83 | 16.9 | ③ | AD |
| RASTOGI[ | 2018 | 印度 | 100 | 49.5(21~79) | 13 | 13.0 | ③ | AD |
| TSAI[ | 2018 | 美国 | 522 | 63 | 102 | 19.5 | ①或③ | ABCD |
| ZOU[ | 2018 | 中国 | 387 | 50(24,81) | 114 | 29.4 | ③ | ABCD |
| 张顺康[ | 2018 | 中国 | 197 | 55.94(28~79) | 38 | 19.3 | ③ | C |
| RIBEIRO PEREIRA[ | 2017 | 巴西 | 964 | 55.31±12.98 | 300 | 31.1 | ④ | ADE |
| ZHANG[ | 2017 | 中国 | 2 597 | 49.9±10.1 | 277 | 10.7 | ③ | AE |
| ZHU[ | 2017 | 中国 | 319 | 18~75 | 88 | 27.6 | ⑤ | B |
| KWAN[ | 2016 | 美国 | 2 953 | 非水肿60.0±11.9;水肿患者56.0±11.1 | 342 | 11.6 | ① | — |
| MENEZES[ | 2016 | 巴西 | 622 | 258例年龄<50,364例年龄≥50 | 204 | 32.8 | ④ | B |
| WANG[ | 2016 | 中国 | 358 | >18 | 114 | 31.8 | ③ | CDE |
| KILBREATH[ | 2016 | 澳大利亚 | 450 | 56.9±11.2 | 46 | 10.2 | ⑥ | D |
| 刘风华[ | 2016 | 中国 | 141 | 51(24,81) | 39 | 27.7 | ①或③ | ABCD |
| SWAROOP[ | 2015 | 美国 | 1 121 | 不清楚 | 59 | 5.3 | ⑦ | ACD |
| BOUGHEY[ | 2014 | 美国 | 124 | 59(36~85) | 38 | 30.7 | ⑧ | AC |
| IKEDA[ | 2014 | 日本 | 76 | 非水肿(n=52):60.8±13.7;水肿患者(n=24):55.3±9.6 | 24 | 31.6 | ③ | CD |
| TOGAWA[ | 2014 | 美国 | 666 | 51.5±7.2 | 190 | 28.5 | ① | AB |
| JAMMOLLO[ | 2013 | 美国 | 787 | 56(27~89) | 39 | 5.0 | ② | ACD |
| RIDENER[ | 2011 | 美国 | 138 | 58.9±12.3 | 27 | 19.6 | ②或④ | A |
| AVRAHAM[ | 2010 | 美国 | 316 | 非乳房重建(n=130):61(30~83);乳房重建(n=186):45(27~74) | 34 | 10.8 | ③ | B |
| CLOUGH-GORR[ | 2010 | 美国 | 400 | >65 | 145 | 36.3 | ① | AB |
| GOLDBERG[ | 2010 | 美国 | 600 | 56(24~83) | 31 | 5.2 | ③ | ABCDE |
| HAYES[ | 2010 | 澳大利亚 | 287 | 54±10 | 不清楚 | NR | ⑥ | E |
| HELYER[ | 2010 | 加拿大 | 137 | 56(36~78) | 16 | 11.7 | ④ | A |
| KWAN[ | 2010 | 美国 | 997 | 水肿(n=133):55.3±11.1;非水肿(n=864):55.3±11.1 | 133 | 13.3 | ⑧ | ABCD |
| NORMAN[ | 2010 | 美国 | 631 | 196例<50,435例≥50 | 238 | 37.7 | ① | ABCDE |
| YANG[ | 2010 | 韩国 | 183 | 不清楚 | 22 | 12.0 | ⑨ | BCD |
| MEESK[ | 2009 | 美国 | 494 | 35~64 | 120 | 24.2 | ① | AC |
| YEN[ | 2009 | 美国 | 1 338 | 水肿(n=193):71.9±5.2;非水肿(n=1 145):72.9±5.6 | 193 | 14.4 | ① | BCD |
| HAYES[ | 2008 | 澳大利亚 | 287 | 54±10 | 41 | 23.6 | ①或⑥ | AC |
| PASKETT[ | 2007 | 美国 | 622 | 38.5±4.9 | 336 | 54.0 | ① | BCD |
| WILKE[ | 2006 | 美国 | 2 904 | 56(23~95) | 203 | 7.0 | ③ | A |
| NIWIN'SKA[ | 2005 | 波兰 | 174 | 53(28~76) | 17 | 9.8 | ③ | C |
| OZASLAN[ | 2004 | 土耳其 | 240 | 50(28~80) | 68 | 28.3 | ③ | AD |
| GELLER[ | 2003 | 美国 | 145 | 水肿(n=55):49.7±8.5;非水肿(n=90):59.5±12.4 | 55 | 37.9 | ① | BCD |
表2 纳入研究基本特征
Table 2 Characteristics of included studies
| 第一作者 | 发表时间(年) | 国家 | 样本量(例) | 年龄(岁) | 水肿例数(例) | 发生率(%) | 诊断标准 | 危险因素 |
|---|---|---|---|---|---|---|---|---|
| KUIJER[ | 2021 | 美国 | 888 | 37(22~40) | 122 | 13.7 | ① | ABC |
| KEELY[ | 2021 | 美国 | 1 100 | 56±12 | 251 | 22.8 | ② | E |
| KIM[ | 2021 | 韩国 | 910 | 腋窝淋巴结清扫(n=595):52.5±10.4;前哨淋巴结活检(n=315):51.6±10.5 | 121 | 13.3 | ③ | ABCD |
| BIDYUT[ | 2021 | 印度 | 342 | 47 | 144 | 42.1 | ① | AB |
| 佟洋[ | 2021 | 中国 | 713 | 水肿(n=61):55.17±13.26;非水肿(n=652):54.81±11.59 | 61 | 8.6 | ③ | AD |
| 袁芊芊[ | 2021 | 中国 | 312 | 48 | 45 | 14.4 | ② | AD |
| BRUNELLE[ | 2020 | 美国 | 647 | 56.6(27~83) | 64 | 9.9 | ② | ABCD |
| BRUNELLE[ | 2020 | 美国 | 1 181 | 569例≥55,612例<55 | 129 | 10.9 | ② | ABCDE |
| BUNDRED[ | 2020 | 英国 | 545 | 55.7±12.4 | 122 | 22.4 | ② | AE |
| NAOUM[ | 2020 | 美国 | 1 815 | 56(24.4,87.9) | 171 | 9.4 | ② | C |
| 王季[ | 2020 | 中国 | 472 | 水肿(n=23):55.57±13.14;非水肿(n=449):54.83±11.10 | 23 | 4.9 | ①或③ | ACD |
| ARMER[ | 2019 | 美国 | 486 | 50.1±10.8 | 284 | 58.4 | ② | AD |
| GROSS[ | 2019 | 美国 | 265 | 52.6(42.7,62.1) | 39 | 14.7 | ③ | A |
| KHANNA[ | 2019 | 印度 | 98 | 76.8%年龄41~60 | 23 | 23.5 | ③ | DE |
| GROSS[ | 2018 | 美国 | 492 | 50(40~60) | 83 | 16.9 | ③ | AD |
| RASTOGI[ | 2018 | 印度 | 100 | 49.5(21~79) | 13 | 13.0 | ③ | AD |
| TSAI[ | 2018 | 美国 | 522 | 63 | 102 | 19.5 | ①或③ | ABCD |
| ZOU[ | 2018 | 中国 | 387 | 50(24,81) | 114 | 29.4 | ③ | ABCD |
| 张顺康[ | 2018 | 中国 | 197 | 55.94(28~79) | 38 | 19.3 | ③ | C |
| RIBEIRO PEREIRA[ | 2017 | 巴西 | 964 | 55.31±12.98 | 300 | 31.1 | ④ | ADE |
| ZHANG[ | 2017 | 中国 | 2 597 | 49.9±10.1 | 277 | 10.7 | ③ | AE |
| ZHU[ | 2017 | 中国 | 319 | 18~75 | 88 | 27.6 | ⑤ | B |
| KWAN[ | 2016 | 美国 | 2 953 | 非水肿60.0±11.9;水肿患者56.0±11.1 | 342 | 11.6 | ① | — |
| MENEZES[ | 2016 | 巴西 | 622 | 258例年龄<50,364例年龄≥50 | 204 | 32.8 | ④ | B |
| WANG[ | 2016 | 中国 | 358 | >18 | 114 | 31.8 | ③ | CDE |
| KILBREATH[ | 2016 | 澳大利亚 | 450 | 56.9±11.2 | 46 | 10.2 | ⑥ | D |
| 刘风华[ | 2016 | 中国 | 141 | 51(24,81) | 39 | 27.7 | ①或③ | ABCD |
| SWAROOP[ | 2015 | 美国 | 1 121 | 不清楚 | 59 | 5.3 | ⑦ | ACD |
| BOUGHEY[ | 2014 | 美国 | 124 | 59(36~85) | 38 | 30.7 | ⑧ | AC |
| IKEDA[ | 2014 | 日本 | 76 | 非水肿(n=52):60.8±13.7;水肿患者(n=24):55.3±9.6 | 24 | 31.6 | ③ | CD |
| TOGAWA[ | 2014 | 美国 | 666 | 51.5±7.2 | 190 | 28.5 | ① | AB |
| JAMMOLLO[ | 2013 | 美国 | 787 | 56(27~89) | 39 | 5.0 | ② | ACD |
| RIDENER[ | 2011 | 美国 | 138 | 58.9±12.3 | 27 | 19.6 | ②或④ | A |
| AVRAHAM[ | 2010 | 美国 | 316 | 非乳房重建(n=130):61(30~83);乳房重建(n=186):45(27~74) | 34 | 10.8 | ③ | B |
| CLOUGH-GORR[ | 2010 | 美国 | 400 | >65 | 145 | 36.3 | ① | AB |
| GOLDBERG[ | 2010 | 美国 | 600 | 56(24~83) | 31 | 5.2 | ③ | ABCDE |
| HAYES[ | 2010 | 澳大利亚 | 287 | 54±10 | 不清楚 | NR | ⑥ | E |
| HELYER[ | 2010 | 加拿大 | 137 | 56(36~78) | 16 | 11.7 | ④ | A |
| KWAN[ | 2010 | 美国 | 997 | 水肿(n=133):55.3±11.1;非水肿(n=864):55.3±11.1 | 133 | 13.3 | ⑧ | ABCD |
| NORMAN[ | 2010 | 美国 | 631 | 196例<50,435例≥50 | 238 | 37.7 | ① | ABCDE |
| YANG[ | 2010 | 韩国 | 183 | 不清楚 | 22 | 12.0 | ⑨ | BCD |
| MEESK[ | 2009 | 美国 | 494 | 35~64 | 120 | 24.2 | ① | AC |
| YEN[ | 2009 | 美国 | 1 338 | 水肿(n=193):71.9±5.2;非水肿(n=1 145):72.9±5.6 | 193 | 14.4 | ① | BCD |
| HAYES[ | 2008 | 澳大利亚 | 287 | 54±10 | 41 | 23.6 | ①或⑥ | AC |
| PASKETT[ | 2007 | 美国 | 622 | 38.5±4.9 | 336 | 54.0 | ① | BCD |
| WILKE[ | 2006 | 美国 | 2 904 | 56(23~95) | 203 | 7.0 | ③ | A |
| NIWIN'SKA[ | 2005 | 波兰 | 174 | 53(28~76) | 17 | 9.8 | ③ | C |
| OZASLAN[ | 2004 | 土耳其 | 240 | 50(28~80) | 68 | 28.3 | ③ | AD |
| GELLER[ | 2003 | 美国 | 145 | 水肿(n=55):49.7±8.5;非水肿(n=90):59.5±12.4 | 55 | 37.9 | ① | BCD |
| 第一作者 | 人群选择 | 组间可比性 | 结局测量 | 总分 | 第一作者 | 人群选择 | 组间可比性 | 结局测量 | 总分 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ① | ② | ③ | ④ | ⑤ | ⑥ | ⑦ | ⑧ | ① | ② | ③ | ④ | ⑤ | ⑥ | ⑦ | ⑧ | ||||
| KUIJER[ | 1 | 1 | 1 | 1 | 2 | 0 | 0 | 1 | 7 | KILBREATH[ | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 1 | 7 |
| KEELY[ | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 7 | 刘风华[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 |
| KIM[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | SWAROOP[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| BIDYUF[ | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 7 | BOUGHEY[ | 1 | 0 | 1 | 1 | 2 | 1 | 1 | 1 | 8 |
| 佟洋[ | 1 | 1 | 0 | 1 | 2 | 1 | 0 | 1 | 7 | IKEDA[ | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 |
| 袁芊芊[ | 1 | 1 | 1 | 1 | 2 | 1 | 0 | 0 | 7 | TOGAWA[ | 1 | 1 | 1 | 0 | 2 | 0 | 1 | 1 | 7 |
| BRUNELLE[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | JAMMOLLO[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| BRUNELLE[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | RIDENER[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| BUNDRED[ | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 | AVRAHAM[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| NAOUM[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | CLOUGH-GORR[ | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 1 | 8 |
| 王季[ | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 7 | GOLDBERG[ | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 8 |
| ARMER[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | HAYES[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| GROSS[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | HELYER[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 |
| KHANNA[ | 1 | 1 | 0 | 1 | 2 | 1 | 0 | 1 | 7 | KWAN[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 |
| GROSS[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | NORMAN[ | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 1 | 8 |
| RASTOGI[ | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 | YANG[ | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 1 | 7 |
| TSAI[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | MEESK[ | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 1 | 8 |
| ZOU[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | YEN[ | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 1 | 8 |
| 张顺康[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | HAYES[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| RIBEIRO PEREIRA[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | PASKETT[ | 1 | 1 | 1 | 0 | 2 | 0 | 1 | 1 | 7 |
| ZHANG[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | WILKE[ | 1 | 1 | 0 | 0 | 2 | 1 | 1 | 1 | 7 |
| ZHU[ | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 7 | NIWIN'SKA[ | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 7 |
| KWAN[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | OZASLAN[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| MENEZES[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | GELLER[ | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 1 | 8 |
| WANG[ | 1 | 1 | 1 | 1 | 2 | 1 | 0 | 1 | 8 | ||||||||||
表3 纳入文献质量评价结果(分)
Table 3 Quality appraisal results of included studies
| 第一作者 | 人群选择 | 组间可比性 | 结局测量 | 总分 | 第一作者 | 人群选择 | 组间可比性 | 结局测量 | 总分 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ① | ② | ③ | ④ | ⑤ | ⑥ | ⑦ | ⑧ | ① | ② | ③ | ④ | ⑤ | ⑥ | ⑦ | ⑧ | ||||
| KUIJER[ | 1 | 1 | 1 | 1 | 2 | 0 | 0 | 1 | 7 | KILBREATH[ | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 1 | 7 |
| KEELY[ | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 7 | 刘风华[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 |
| KIM[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | SWAROOP[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| BIDYUF[ | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 7 | BOUGHEY[ | 1 | 0 | 1 | 1 | 2 | 1 | 1 | 1 | 8 |
| 佟洋[ | 1 | 1 | 0 | 1 | 2 | 1 | 0 | 1 | 7 | IKEDA[ | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 |
| 袁芊芊[ | 1 | 1 | 1 | 1 | 2 | 1 | 0 | 0 | 7 | TOGAWA[ | 1 | 1 | 1 | 0 | 2 | 0 | 1 | 1 | 7 |
| BRUNELLE[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | JAMMOLLO[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| BRUNELLE[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | RIDENER[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| BUNDRED[ | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 | AVRAHAM[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| NAOUM[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | CLOUGH-GORR[ | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 1 | 8 |
| 王季[ | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 7 | GOLDBERG[ | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 8 |
| ARMER[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | HAYES[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| GROSS[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | HELYER[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 |
| KHANNA[ | 1 | 1 | 0 | 1 | 2 | 1 | 0 | 1 | 7 | KWAN[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 |
| GROSS[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | NORMAN[ | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 1 | 8 |
| RASTOGI[ | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 | YANG[ | 1 | 1 | 1 | 0 | 2 | 1 | 0 | 1 | 7 |
| TSAI[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | MEESK[ | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 1 | 8 |
| ZOU[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | YEN[ | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 1 | 8 |
| 张顺康[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | HAYES[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| RIBEIRO PEREIRA[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | PASKETT[ | 1 | 1 | 1 | 0 | 2 | 0 | 1 | 1 | 7 |
| ZHANG[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | WILKE[ | 1 | 1 | 0 | 0 | 2 | 1 | 1 | 1 | 7 |
| ZHU[ | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 7 | NIWIN'SKA[ | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 7 |
| KWAN[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | OZASLAN[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| MENEZES[ | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | GELLER[ | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 1 | 8 |
| WANG[ | 1 | 1 | 1 | 1 | 2 | 1 | 0 | 1 | 8 | ||||||||||
| 危险因素 | 分组 | 研究数量(篇) | 病例数(例) | 样本量(例) | 模型 | I2(%) | P值 | RR(95%CI) | Egger's P值 | β |
|---|---|---|---|---|---|---|---|---|---|---|
| BMI | ≥30 kg/m2与<30 kg/m2 | 14[ | 1 945 | 8 819 | 随机效应模型 | 30.00 | 0.144 | 1.777(1.515,2.085) | 0.488 | 0.575 |
| 乳腺手术类型 | 乳腺切除术与肿物切除术 | 16[ | 1 786 | 9 955 | 随机效应模型 | 26.50 | 0.157 | 1.320(1.125,1.549) | 0.809 | 0.278 |
| 腋窝手术类型 | ALND与SLNB | 10[ | 1 132 | 7 327 | 随机效应模型 | 16.30 | 0.289 | 3.058(2.325,4.020) | 0.465 | 1.118 |
| 放疗 | 是与否 | 12[ | 1 652 | 6 849 | 随机效应模型 | 61.50 | 0.003 | 1.620(1.214,2.160) | 0.853 | 0.482 |
| 术后并发症 | 是与否 | 6[ | 1 089 | 6 331 | 随机效应模型 | 74.00 | 0.002 | 2.373(1.278,4.405) | — | 0.864 |
表4 BCRL风险因素的Meta分析及异质性检验结果
Table 4 Meta-analysis and heterogeneity test of risk factors for breast cancer-related lymphedema
| 危险因素 | 分组 | 研究数量(篇) | 病例数(例) | 样本量(例) | 模型 | I2(%) | P值 | RR(95%CI) | Egger's P值 | β |
|---|---|---|---|---|---|---|---|---|---|---|
| BMI | ≥30 kg/m2与<30 kg/m2 | 14[ | 1 945 | 8 819 | 随机效应模型 | 30.00 | 0.144 | 1.777(1.515,2.085) | 0.488 | 0.575 |
| 乳腺手术类型 | 乳腺切除术与肿物切除术 | 16[ | 1 786 | 9 955 | 随机效应模型 | 26.50 | 0.157 | 1.320(1.125,1.549) | 0.809 | 0.278 |
| 腋窝手术类型 | ALND与SLNB | 10[ | 1 132 | 7 327 | 随机效应模型 | 16.30 | 0.289 | 3.058(2.325,4.020) | 0.465 | 1.118 |
| 放疗 | 是与否 | 12[ | 1 652 | 6 849 | 随机效应模型 | 61.50 | 0.003 | 1.620(1.214,2.160) | 0.853 | 0.482 |
| 术后并发症 | 是与否 | 6[ | 1 089 | 6 331 | 随机效应模型 | 74.00 | 0.002 | 2.373(1.278,4.405) | — | 0.864 |
| 风险因素 | Logistic评分 | Additive评分 |
|---|---|---|
| BMI(kg/m2) | ||
| ≥30 | 6 | 2 |
| <30 | 0 | 1 |
| 乳腺手术类型 | ||
| 全乳切除 | 3 | 2 |
| 肿物切除 | 0 | 1 |
| 腋窝手术类型 | ||
| ALND | 11 | 3 |
| SLNB | 0 | 1 |
| 放疗 | ||
| 是 | 5 | 2 |
| 否 | 0 | 1 |
| 术后并发症 | ||
| 是 | 9 | 2 |
| 否 | 0 | 1 |
表5 Logistic和Additive评分模型(分)
Table 5 Logistic and Additive risk scoring models for breast cancer-related lymphedema
| 风险因素 | Logistic评分 | Additive评分 |
|---|---|---|
| BMI(kg/m2) | ||
| ≥30 | 6 | 2 |
| <30 | 0 | 1 |
| 乳腺手术类型 | ||
| 全乳切除 | 3 | 2 |
| 肿物切除 | 0 | 1 |
| 腋窝手术类型 | ||
| ALND | 11 | 3 |
| SLNB | 0 | 1 |
| 放疗 | ||
| 是 | 5 | 2 |
| 否 | 0 | 1 |
| 术后并发症 | ||
| 是 | 9 | 2 |
| 否 | 0 | 1 |
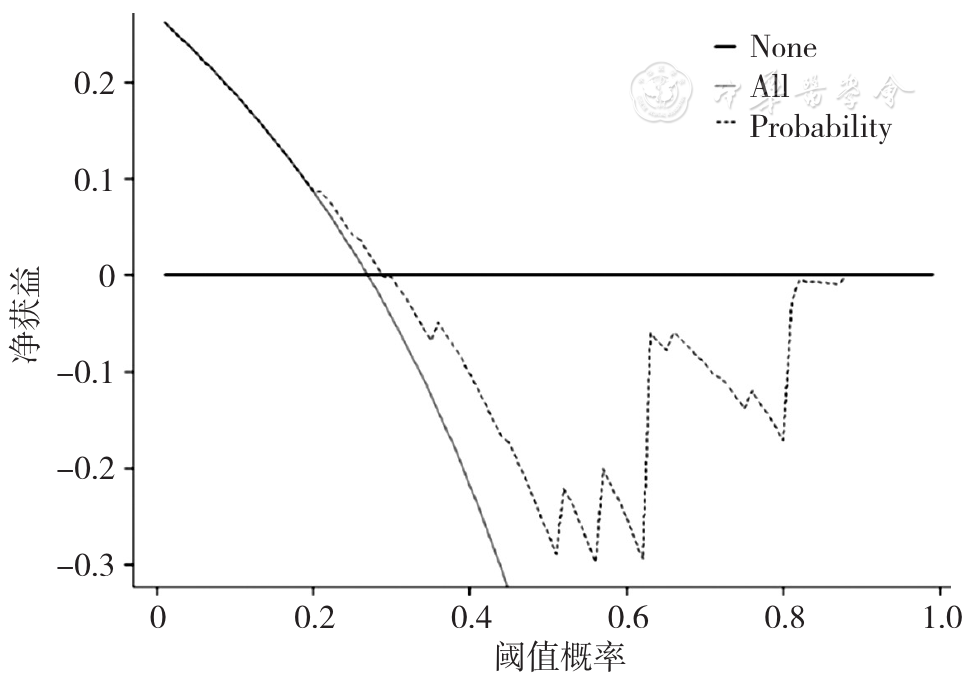
图3 BCRL Logistic评分模型的决策曲线注:None表示所有样本是阴性,无干预,净获益为0;All表示所有样本是阳性,接受干预,净获益是斜率为负值的反斜线;Probability表示使用Logistic评分模型
Figure 3 Decision curve of Logistic risk prediction model for breast cancer-related lymphedema
| [1] |
|
| [2] |
|
| [3] |
张蕊,郑黎强,潘国伟. 疾病发病风险预测模型的应用与建立[J]. 中国卫生统计,2015,32(4):724-726.
|
| [4] |
王艺璇,李惠萍,丁晓彤,等. 乳腺癌术后淋巴水肿风险预测模型的研究进展[J]. 中华护理杂志,2018,53(6):740-743. DOI:10.3761/j.issn.0254-1769.2018.06.020.
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
李惠萍,王玲,杨娅娟,等. 乳腺癌患者术后淋巴水肿风险评分系统的构建和评价[J]. 中国全科医学,2014,17(18):2056-2061,2069. DOI:10.3969/j.issn.1007-9572.2014.18.002.
|
| [12] |
|
| [13] |
黄悦勤. 临床流行病学[M]. 4版.北京:人民卫生出版社,2014.
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
佟洋,史妍萍,翟海昕. 乳腺癌术后乳房再造患者上肢淋巴水肿与体质量指数的相关性分析[J]. 中国医学前沿杂志(电子版),2021,13(10):104-107. DOI:10.12037/YXQY.2021.10-21.
|
| [19] |
袁芊芊,侯晋轩,苏科华,等. 基于上肢淋巴引流的乳腺癌术后水肿风险因素分析[J]. 中华普通外科杂志,2021,36(8):579-584. DOI:10.3760/cma.j.cn113855-20210203-00084.
|
| [20] |
|
| [21] |
|
| [22] |
|
| [23] |
|
| [24] |
王季,张意辉,张丽娟,等. 体重指数及体重波动对乳腺癌患者上肢淋巴水肿的影响[J]. 中国康复医学杂志,2020,35(2):182-185. DOI:10.3969/j.issn.1001-1242.2020.02.011.
|
| [25] |
|
| [26] |
|
| [27] |
|
| [28] |
|
| [29] |
|
| [30] |
|
| [31] |
|
| [32] |
张顺康,孙丽云,陈刚. 乳腺癌改良根治术后放疗患者上肢淋巴水肿与腋淋巴结手术结果的相关性分析[J]. 中国癌症杂志,2018,28(1):55-61. DOI:10.19401/j.cnki.1007-3639.2018.01.008.
|
| [33] |
|
| [34] |
|
| [35] |
|
| [36] |
|
| [37] |
|
| [38] |
|
| [39] |
刘风华,胡艳,沈培佩,等. 乳腺癌相关淋巴水肿发病情况及危险因素前瞻性队列研究[J]. 中华放射肿瘤学杂志,2016,25(6):593-597. DOI:10.3760/cma.j.issn.1004-4221.2016.06.011.
|
| [40] |
|
| [41] |
|
| [42] |
|
| [43] |
|
| [44] |
|
| [45] |
|
| [46] |
|
| [47] |
|
| [48] |
|
| [49] |
|
| [50] |
|
| [51] |
|
| [52] |
|
| [53] |
|
| [54] |
|
| [55] |
|
| [56] |
|
| [57] |
|
| [58] |
|
| [59] |
|
| [60] |
|
| [61] |
|
| [62] |
|
| [63] |
李娟,苑博,王轶书,等. 乳腺癌患者决策辅助的研究进展[J]. 中南大学学报(医学版),2021,46(2):176-182. DOI:10.11817/j.issn.1672-7347.2021.190584.
|
| [64] |
|
| [65] |
|
| [66] |
|
| [67] |
张浩,刘锐芮,朱琳,等. 中国女性乳腺癌相关淋巴水肿危险因素的Meta分析[J]. 中国全科医学,2021,24(26):3349-3358,3376. DOI:10.12114/j.issn.1007-9572.2021.01.206.
|
| [68] |
|
| [69] |
|
| [70] |
|
| [71] |
|
| [72] |
|
| [73] |
郑思娣. 基于前瞻性监测模型的乳腺癌患者术后康复研究[D]. 广州:广东药科大学,2019.
|
| [1] | 许佳兰, 阎红, 文君, 周紫彤, 王思宇. 老年癌症患者潜在不适当用药发生率的Meta分析[J]. 中国全科医学, 2025, 28(30): 3815-3822. |
| [2] | 徐百川, 王艳, 张彭, 李艺婷, 刘飞来, 谢洋. 慢性阻塞性肺疾病共病肺癌筛查工具分析[J]. 中国全科医学, 2025, 28(30): 3847-3852. |
| [3] | 邵晓颖, 邵洁, 朱焱, 邵金玲, 尚灵, 吴振莲, 赵钰, 张加才. 贵州省6~36月龄儿童铁缺乏现状及缺铁性贫血影响因素研究[J]. 中国全科医学, 2025, 28(27): 3368-3374. |
| [4] | 张天宇, 于海搏, 陈飞, 李新, 张佳佳, 詹晓凯, 申曼, 汤然, 范斯斌, 赵凤仪, 黄仲夏. POEMS综合征全身系统性治疗疗效和安全性的Meta分析[J]. 中国全科医学, 2025, 28(27): 3447-3455. |
| [5] | 全家霖, 朱琳, 苏煜, 陈泽恺, 陈梓淇, 张卓凡. 运动方式对超重或肥胖儿童青少年执行功能改善效果的网状Meta分析[J]. 中国全科医学, 2025, 28(27): 3422-3431. |
| [6] | 刘银银, 隋鸿平, 李婷婷, 姜桐桐, 史铁英, 夏云龙. 乳腺癌治疗相关心脏毒性风险预测模型的研究进展[J]. 中国全科医学, 2025, 28(24): 3072-3078. |
| [7] | 蒋世华, 朱政, 任盈盈, 朱垚磊, 王越, 高希彬. 中国儿童青少年近视患病率及影响因素的Meta分析[J]. 中国全科医学, 2025, 28(24): 3043-3052. |
| [8] | 李浩, 李江涛, 刘丹, 王建军. 贝利尤单抗和阿尼鲁单抗及泰它西普治疗系统性红斑狼疮疗效和安全性的网状Meta分析[J]. 中国全科医学, 2025, 28(23): 2924-2933. |
| [9] | 王笑林, 李秋月, 周彦君, 张金辉, 梁涛. 转移性结直肠癌患者呋喹替尼治疗相关心血管毒性发生率和风险的Meta分析[J]. 中国全科医学, 2025, 28(23): 2934-2940. |
| [10] | 周倩, 吴晓敏, 王宝华, 严若菡, 蔚苗, 吴静. 胃癌发生风险的列线图预测模型研究[J]. 中国全科医学, 2025, 28(23): 2870-2877. |
| [11] | 马盼盼, 王思静, 游娜, 丁大法, 鲁一兵. Danuglipron与Orforglipron治疗2型糖尿病疗效及安全性的Meta分析[J]. 中国全科医学, 2025, 28(21): 2679-2685. |
| [12] | 胡婉琴, 余深艳, 曹学华, 向凤, 贾钰. 中国儿童性早熟影响因素的Meta分析[J]. 中国全科医学, 2025, 28(21): 2661-2671. |
| [13] | 阿迪力·吐尔孙, 程刚. 非奈利酮治疗2型糖尿病肾病有效性和安全性的Meta分析[J]. 中国全科医学, 2025, 28(21): 2686-2691. |
| [14] | 郭盛滕, 张芬芬, 万迪, 于冬梅, 王庆华. 重症急性胰腺炎并发急性肺损伤危险因素的Meta分析[J]. 中国全科医学, 2025, 28(20): 2546-2554. |
| [15] | 罗云昭, 蒋宏传, 徐峰. 基于深度学习模型辅助穿刺病理图像预测乳腺癌新辅助治疗疗效的研究[J]. 中国全科医学, 2025, 28(19): 2407-2413. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





