中国全科医学 ›› 2023, Vol. 26 ›› Issue (09): 1151-1158.DOI: 10.12114/j.issn.1007-9572.2022.0676
所属专题: 骨健康最新文章合辑; 运动相关研究最新文章合辑; 骨质疏松最新文章合辑; 生活方式干预相关研究最新文章合集
• 最佳证据 • 上一篇
收稿日期:2022-09-01
修回日期:2022-10-25
出版日期:2023-03-20
发布日期:2022-10-31
通讯作者:
王俊杰
WANG Xixi, SHEN Rui, WANG Junjie*( ), XU Niying
), XU Niying
Received:2022-09-01
Revised:2022-10-25
Published:2023-03-20
Online:2022-10-31
Contact:
WANG Junjie
摘要: 背景 运动为防治绝经后骨质疏松症经济有效的干预措施之一,但目前其相关证据内容广泛且分散,临床尚无规范、全面的运动指导方案。 目的 检索、评价并总结绝经后骨质疏松症患者运动干预的最佳证据。 方法 系统检索BMJ Best Practice、Up To Date临床顾问、DynaMed,英国国家临床医学研究所指南网、国际指南网、苏格兰学院间指南网、美国指南网,加拿大安大略注册护士协会、国际骨质疏松症基金会、英国皇家骨质疏松协会、美国骨质疏松症基金会、澳大利亚皇家全科医师学院、美国妇产科医师学会、加拿大妇产科医师协会、医脉通、澳大利亚乔安娜循证研究所网站,Cochrane Library、CINAHL、Web of Science、PubMed、Embase、中国知网、中国生物医学文献服务系统中关于绝经后骨质疏松症运动干预的临床实践指南、临床决策、证据总结、专家共识、系统评价。检索时限为建库至2022年1月。采用临床指南研究与评价系统(AGREE Ⅱ)对指南进行质量评价,采用证据总结评价工作表(CASE)对临床决策进行质量评价,采用澳大利亚JBI循证卫生保健中心专家共识的真实性评价工具(2016版)对专家共识进行质量评价,采用澳大利亚JBI循证卫生保健中心系统评价方法学质量评价工具(2016版)对系统评价进行质量评价。 结果 共纳入18篇文献,其中指南7篇、临床决策2篇、专家共识4篇、系统评价5篇,从运动前评估、运动类型、运动强度和时间、健康教育及注意事项5个方面提取了22条证据。 结论 本文从运动前评估、运动类型、运动强度和时间、健康教育及注意事项5个方面提取了绝经后骨质疏松症患者运动干预的最佳证据,医护人员可参考最佳证据为绝经后骨质疏松症患者提供合理的运动指导方案,减少其跌倒和骨折发生率以提高生活质量。
| 第一作者 | 发表年份(年) | 来源 | 文献类型 | 文献主题 |
|---|---|---|---|---|
| CAMACHO[ | 2020 | PubMed | 指南 | 绝经后骨质疏松症诊断和治疗临床实践指南 |
| Osteoporosis Australia[ | 2017 | RACGP | 指南 | 绝经后50岁以上女性和男性骨质疏松症的预防、诊断和管理 |
| SIGN[ | 2021 | SIGN | 指南 | 骨质疏松症的治疗和脆性骨折的预防 |
| ACOG[ | 2021 | 医脉通 | 指南 | 骨质疏松症的预防、筛查和诊断 |
| 中国康复医学会[ | 2019 | 中国知网 | 指南 | 骨质疏松症康复指南 |
| TARANTINO[ | 2017 | PubMed | 指南 | 预防和治疗骨质疏松症的临床指南 |
| SANCHEZ-RODRIGUEZ[ | 2020 | PubMed | 指南 | 绝经后妇女骨质疏松症管理指南 |
| TANGPRICHA[ | 2018 | DynaMed | 临床决策 | 绝经后女性的骨质疏松 |
| ROSEN[ | 2021 | Up to Date | 临床决策 | 绝经后女性骨质疏松症管理 |
| GIANGREGORIO[ | 2015 | PubMed | 专家共识 | 关于成人骨质疏松症伴或不伴椎体骨折的体育活动和运动建议 |
| 中国营养学会骨营养与健康分会[ | 2020 | 中国知网 | 专家共识 | 原发性骨质疏松症患者的营养和运动管理专家共识 |
| BECK[ | 2017 | PubMed | 专家共识 | 关于预防和管理骨质疏松症运动处方的立场声明 |
| SONGPATANASILP[ | 2016 | PubMed | 专家共识 | 关于骨质疏松症管理的立场声明 |
| XU[ | 2016 | PubMed | 系统评价 | 从年轻女孩到绝经后妇女,运动对女性受试者骨骼状况的影响 |
| KISTLER-FISCHBACHER[ | 2021 | PubMed | 系统评价 | 运动强度对绝经后妇女骨骼的影响 |
| MARÍN-CASCALES[ | 2018 | PubMed | 系统评价 | 绝经后妇女全身振动训练与骨健康 |
| 吴志建[ | 2020 | 中国知网 | 系统评价 | 运动锻炼改善绝经后妇女骨密度效果 |
| PONZANO[ | 2021 | PubMed | 系统评价 | 改善骨折风险人群健康相关结果的渐进抗阻训练 |
表1 纳入文献的一般特征(n=18)
Table 1 Basic characteristics of included studies
| 第一作者 | 发表年份(年) | 来源 | 文献类型 | 文献主题 |
|---|---|---|---|---|
| CAMACHO[ | 2020 | PubMed | 指南 | 绝经后骨质疏松症诊断和治疗临床实践指南 |
| Osteoporosis Australia[ | 2017 | RACGP | 指南 | 绝经后50岁以上女性和男性骨质疏松症的预防、诊断和管理 |
| SIGN[ | 2021 | SIGN | 指南 | 骨质疏松症的治疗和脆性骨折的预防 |
| ACOG[ | 2021 | 医脉通 | 指南 | 骨质疏松症的预防、筛查和诊断 |
| 中国康复医学会[ | 2019 | 中国知网 | 指南 | 骨质疏松症康复指南 |
| TARANTINO[ | 2017 | PubMed | 指南 | 预防和治疗骨质疏松症的临床指南 |
| SANCHEZ-RODRIGUEZ[ | 2020 | PubMed | 指南 | 绝经后妇女骨质疏松症管理指南 |
| TANGPRICHA[ | 2018 | DynaMed | 临床决策 | 绝经后女性的骨质疏松 |
| ROSEN[ | 2021 | Up to Date | 临床决策 | 绝经后女性骨质疏松症管理 |
| GIANGREGORIO[ | 2015 | PubMed | 专家共识 | 关于成人骨质疏松症伴或不伴椎体骨折的体育活动和运动建议 |
| 中国营养学会骨营养与健康分会[ | 2020 | 中国知网 | 专家共识 | 原发性骨质疏松症患者的营养和运动管理专家共识 |
| BECK[ | 2017 | PubMed | 专家共识 | 关于预防和管理骨质疏松症运动处方的立场声明 |
| SONGPATANASILP[ | 2016 | PubMed | 专家共识 | 关于骨质疏松症管理的立场声明 |
| XU[ | 2016 | PubMed | 系统评价 | 从年轻女孩到绝经后妇女,运动对女性受试者骨骼状况的影响 |
| KISTLER-FISCHBACHER[ | 2021 | PubMed | 系统评价 | 运动强度对绝经后妇女骨骼的影响 |
| MARÍN-CASCALES[ | 2018 | PubMed | 系统评价 | 绝经后妇女全身振动训练与骨健康 |
| 吴志建[ | 2020 | 中国知网 | 系统评价 | 运动锻炼改善绝经后妇女骨密度效果 |
| PONZANO[ | 2021 | PubMed | 系统评价 | 改善骨折风险人群健康相关结果的渐进抗阻训练 |
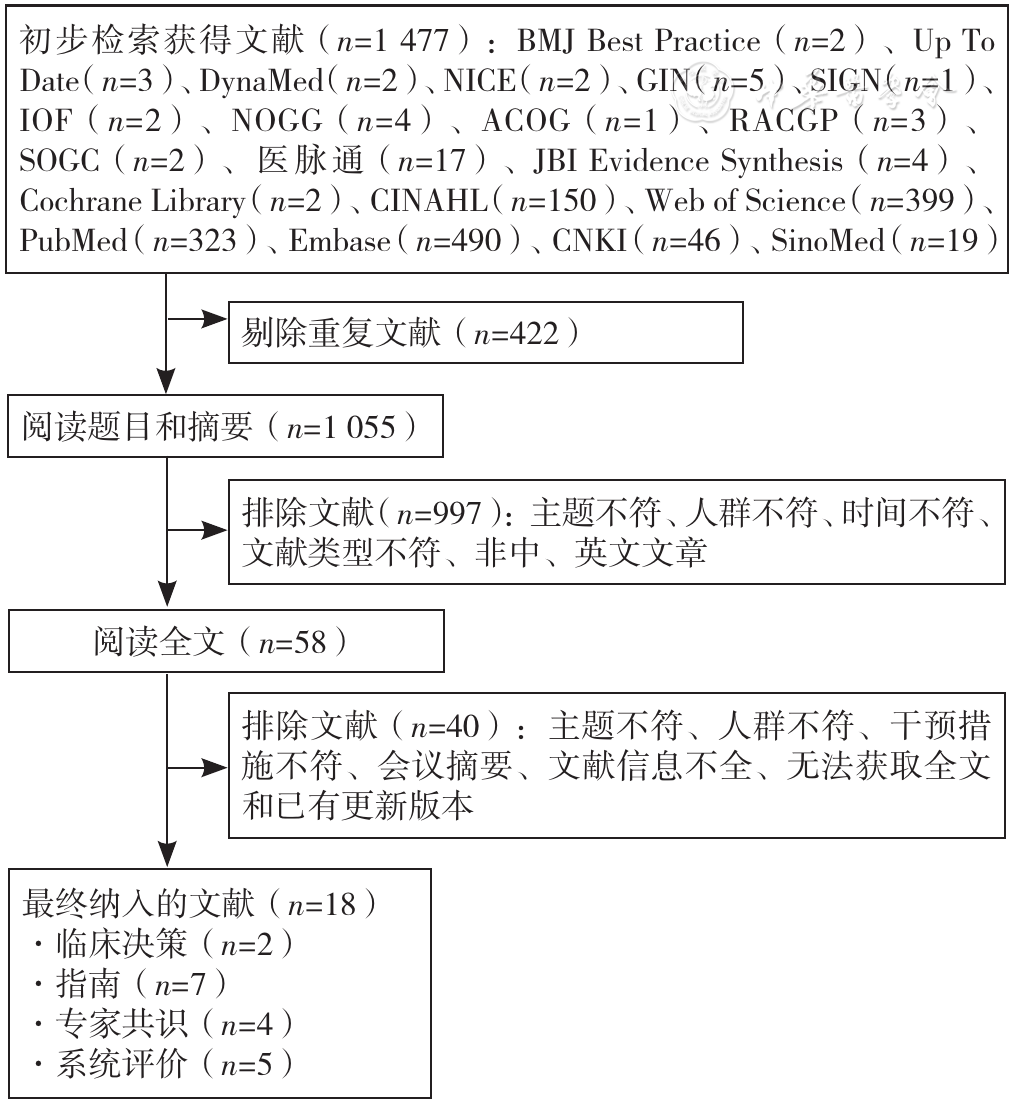
图1 文献筛选流程图注:NICE=英国国家临床医学研究所指南网,GIN=国际指南网,SIGN=苏格兰学院间指南网,IOF=国际骨质疏松症基金会,NOGG=英国皇家骨质疏松协会,ACOG=美国妇产科医师学会,RACGP=澳大利亚皇家全科医师学院,SOGC=加拿大妇产科医师协会,JBI=澳大利亚乔安娜循证研究所,CNKI=中国知网,SinoMed=中国生物医学文献服务系统
Figure 1 Literature screening flowchart
| 纳入文献 | 各领域标准化百分比(%) | ≥60%的领域数(个) | ≥30%的领域数(个) | 推荐级别 | |||||
|---|---|---|---|---|---|---|---|---|---|
| 范围和目的 | 参与人员 | 制订的严谨性 | 呈现的清晰性 | 应用性 | 编写的独立性 | ||||
| CAMACHO[ | 100.00 | 94.44 | 87.50 | 100.00 | 61.11 | 75.00 | 6 | 6 | A |
| Osteoporosis Australia[ | 100.00 | 70.37 | 94.44 | 94.44 | 73.61 | 22.22 | 5 | 6 | B |
| SIGN[ | 100.00 | 81.48 | 85.42 | 100.00 | 81.94 | 88.89 | 6 | 6 | A |
| ACOG[ | 88.89 | 37.04 | 65.97 | 70.37 | 16.67 | 66.67 | 4 | 5 | B |
| 中国康复医学会[ | 100.00 | 100.00 | 97.22 | 90.74 | 87.50 | 100.00 | 6 | 6 | A |
| TARANTINO[ | 90.74 | 66.67 | 65.28 | 79.63 | 62.50 | 41.67 | 5 | 6 | B |
| SANCHEZ-RODRIGUEZ[ | 100.00 | 61.11 | 90.97 | 100.00 | 63.89 | 100.00 | 6 | 6 | A |
表2 指南质量评价结果
Table 2 Quality evaluation of included guidelines
| 纳入文献 | 各领域标准化百分比(%) | ≥60%的领域数(个) | ≥30%的领域数(个) | 推荐级别 | |||||
|---|---|---|---|---|---|---|---|---|---|
| 范围和目的 | 参与人员 | 制订的严谨性 | 呈现的清晰性 | 应用性 | 编写的独立性 | ||||
| CAMACHO[ | 100.00 | 94.44 | 87.50 | 100.00 | 61.11 | 75.00 | 6 | 6 | A |
| Osteoporosis Australia[ | 100.00 | 70.37 | 94.44 | 94.44 | 73.61 | 22.22 | 5 | 6 | B |
| SIGN[ | 100.00 | 81.48 | 85.42 | 100.00 | 81.94 | 88.89 | 6 | 6 | A |
| ACOG[ | 88.89 | 37.04 | 65.97 | 70.37 | 16.67 | 66.67 | 4 | 5 | B |
| 中国康复医学会[ | 100.00 | 100.00 | 97.22 | 90.74 | 87.50 | 100.00 | 6 | 6 | A |
| TARANTINO[ | 90.74 | 66.67 | 65.28 | 79.63 | 62.50 | 41.67 | 5 | 6 | B |
| SANCHEZ-RODRIGUEZ[ | 100.00 | 61.11 | 90.97 | 100.00 | 63.89 | 100.00 | 6 | 6 | A |
| 主题 | 证据描述 | 证据等级 |
|---|---|---|
| 运动前评估 | 1.建议运动前应评估患者合并症、用药史、是否存在骨折跌倒风险因素[ | 5b |
| 2.建议评估患者身体活动的障碍和促进因素,包括当前活动水平、自我效能、疼痛程度、经济水平、个人目标和患者偏好,以促进长期依从性[ | 2c | |
| 运动类型 | 3.建议采用以抗阻运动为主并结合其他类型的多样化运动方案,包括负重运动、冲击训练、有氧运动和平衡训练等[ | 1a |
| 4.建议进行渐进性抗阻运动以缓解股骨颈骨密度下降,如高抬腿、推举杠铃、深蹲、拉弹力带、膝关节伸展、髋外展或屈曲和俯卧背部伸展等[ | 1a | |
| 5.抗阻运动联合冲击运动(带负重背心进行跳跃、踏步、跳绳等)是维持和提高PMOP患者股骨颈和腰椎骨密度的最佳选择[ | 1a | |
| 6.静态负重如单腿站立,可缓解PMOP患者髋部骨密度的下降,动态负重如全身振动训练(WBV)可作为改善PMOP患者腰椎骨密度、运动能力和相关功能参数的治疗手段[ | 1a | |
| 7.负重有氧运动对骨密度和增强肌力有益,如步行、打太极、慢跑、网球、排球、爬楼梯、跳舞等,非负重有氧运动如游泳、骑自行车等对骨骼健康无益[ | 3b | |
| 8.平衡训练可以减少PMOP患者跌倒的频率,如太极、跳舞、踏步走直线、顶书平衡走、从坐姿到站立的练习等[ | 1c | |
| 9.推荐PMOP患者进行中国传统运动如八段锦、五禽戏和太极拳,或与常规运动联合使用,有助于改善患者骨密度,减轻疼痛症状,提高平衡能力,降低跌倒风险[ | 1a | |
| 运动强度和时间 | 10.建议每周进行中高强度的渐进性抗阻运动,负荷量在65%~85% 1 RM的水平中逐渐增加,训练2~3组/次、重复8~12次/组[ | 1b |
| 12.建议进行抗阻运动联合冲击运动30~60 min/次,3次/周,至少持续10个月[ | 1a | |
| 11.建议终生进行定期负重有氧锻炼,如步行30 min/次,包括5~10 min的肢体伸展等运动后缓和放松,或每天30 min/d打太极、跳交际舞等中高强度平衡训练,3~4次/周[ | 1a | |
| 健康教育 | 13.建议绝经后女性尽早开始并坚持长期运动锻炼[ | 1a |
| 14.运动前先进行热身训练,如充分伸展和步行[ | 1c | |
| 15.建议鼓励PMOP患者定期、渐进地进行有规律的运动[ | 1b | |
| 16.建议以前久坐不动、不熟悉抗阻运动或骨折风险高的患者从较低强度训练开始,逐渐增加[ | 5b | |
| 17.建议提供安全运动的培训教育,包括运动姿势、运动范围和举重方式等[ | 1a | |
| 注意事项 | 18.绝经前女性过度运动可能会导致体质量减轻和闭经,从而导致骨质疏松症[ | 1c |
| 19.对于晚期PMOP患者,建议进行预防跌倒和物理治疗的多组分团体或家庭锻炼计划[ | 5b | |
| 20.脊椎骨质疏松或脊椎后凸的患者在日常活动中应避免躯干屈曲和扭转(尤其在弯腰举物、划船、瑜伽、普拉提、保龄球和仰卧起坐等活动中)[ | 5b | |
| 21.高骨折风险的患者,尤其是有脊椎骨质疏松、平衡不良或骨关节炎的患者,禁止进行需要快速、扭转或突然动作的高冲击活动(网球运动、打高尔夫球、跳跃等),用快走、爬楼梯或坐姿举重等低中强度运动替代[ | 5b | |
| 22.如果运动后肌肉酸痛症状超过2 d,建议停止运动,疼痛缓解后可恢复运动,需降低之前的运动强度[ | 5b |
表3 PMOP患者运动干预的最佳证据总结
Table 3 Summary of the best evidence on exercise interventions for osteoporosis in postmenopausal women
| 主题 | 证据描述 | 证据等级 |
|---|---|---|
| 运动前评估 | 1.建议运动前应评估患者合并症、用药史、是否存在骨折跌倒风险因素[ | 5b |
| 2.建议评估患者身体活动的障碍和促进因素,包括当前活动水平、自我效能、疼痛程度、经济水平、个人目标和患者偏好,以促进长期依从性[ | 2c | |
| 运动类型 | 3.建议采用以抗阻运动为主并结合其他类型的多样化运动方案,包括负重运动、冲击训练、有氧运动和平衡训练等[ | 1a |
| 4.建议进行渐进性抗阻运动以缓解股骨颈骨密度下降,如高抬腿、推举杠铃、深蹲、拉弹力带、膝关节伸展、髋外展或屈曲和俯卧背部伸展等[ | 1a | |
| 5.抗阻运动联合冲击运动(带负重背心进行跳跃、踏步、跳绳等)是维持和提高PMOP患者股骨颈和腰椎骨密度的最佳选择[ | 1a | |
| 6.静态负重如单腿站立,可缓解PMOP患者髋部骨密度的下降,动态负重如全身振动训练(WBV)可作为改善PMOP患者腰椎骨密度、运动能力和相关功能参数的治疗手段[ | 1a | |
| 7.负重有氧运动对骨密度和增强肌力有益,如步行、打太极、慢跑、网球、排球、爬楼梯、跳舞等,非负重有氧运动如游泳、骑自行车等对骨骼健康无益[ | 3b | |
| 8.平衡训练可以减少PMOP患者跌倒的频率,如太极、跳舞、踏步走直线、顶书平衡走、从坐姿到站立的练习等[ | 1c | |
| 9.推荐PMOP患者进行中国传统运动如八段锦、五禽戏和太极拳,或与常规运动联合使用,有助于改善患者骨密度,减轻疼痛症状,提高平衡能力,降低跌倒风险[ | 1a | |
| 运动强度和时间 | 10.建议每周进行中高强度的渐进性抗阻运动,负荷量在65%~85% 1 RM的水平中逐渐增加,训练2~3组/次、重复8~12次/组[ | 1b |
| 12.建议进行抗阻运动联合冲击运动30~60 min/次,3次/周,至少持续10个月[ | 1a | |
| 11.建议终生进行定期负重有氧锻炼,如步行30 min/次,包括5~10 min的肢体伸展等运动后缓和放松,或每天30 min/d打太极、跳交际舞等中高强度平衡训练,3~4次/周[ | 1a | |
| 健康教育 | 13.建议绝经后女性尽早开始并坚持长期运动锻炼[ | 1a |
| 14.运动前先进行热身训练,如充分伸展和步行[ | 1c | |
| 15.建议鼓励PMOP患者定期、渐进地进行有规律的运动[ | 1b | |
| 16.建议以前久坐不动、不熟悉抗阻运动或骨折风险高的患者从较低强度训练开始,逐渐增加[ | 5b | |
| 17.建议提供安全运动的培训教育,包括运动姿势、运动范围和举重方式等[ | 1a | |
| 注意事项 | 18.绝经前女性过度运动可能会导致体质量减轻和闭经,从而导致骨质疏松症[ | 1c |
| 19.对于晚期PMOP患者,建议进行预防跌倒和物理治疗的多组分团体或家庭锻炼计划[ | 5b | |
| 20.脊椎骨质疏松或脊椎后凸的患者在日常活动中应避免躯干屈曲和扭转(尤其在弯腰举物、划船、瑜伽、普拉提、保龄球和仰卧起坐等活动中)[ | 5b | |
| 21.高骨折风险的患者,尤其是有脊椎骨质疏松、平衡不良或骨关节炎的患者,禁止进行需要快速、扭转或突然动作的高冲击活动(网球运动、打高尔夫球、跳跃等),用快走、爬楼梯或坐姿举重等低中强度运动替代[ | 5b | |
| 22.如果运动后肌肉酸痛症状超过2 d,建议停止运动,疼痛缓解后可恢复运动,需降低之前的运动强度[ | 5b |
| [1] |
|
| [2] |
贾鹏,徐又佳. 绝经后骨质疏松骨折的治疗[J]. 实用妇产科杂志,2020,36(7):492-494.
|
| [3] |
|
| [4] |
|
| [5] |
夏维波,章振林,林华,等. 原发性骨质疏松症诊疗指南(2017)[J]. 中国骨质疏松杂志,2019,25(3):281-309.
|
| [6] |
|
| [7] |
邹军,章岚,任弘,等. 运动防治骨质疏松专家共识[J]. 中国骨质疏松杂志,2015,21(11):1291-1302,1306.
|
| [8] | |
| [9] |
|
| [10] |
韦当,王聪尧,肖晓娟,等. 指南研究与评价(AGREEⅡ)工具实例解读[J]. 中国循证儿科杂志,2013,8(4):316-319. DOI:10.3969/j.issn.1673-5501.2013.04.017.
|
| [11] |
乔舰. 组内相关系数的理论基础及建模应用[J]. 统计与信息论坛,2016,31(11):44-48.
|
| [12] |
|
| [13] |
胡雁,郝玉芳. 循证护理学[M]. 2版. 北京:人民卫生出版社,2018.
|
| [14] |
顾莺,张慧文,周英凤,等. JBI循证卫生保健中心关于不同类型研究的质量评价工具——系统评价的方法学质量评价[J]. 护士进修杂志,2018,33(8):701-703. DOI:10.16821/j.cnki.hsjx.2018.08.008.
|
| [15] |
王春青,胡雁. JBI证据预分级及证据推荐级别系统(2014版)[J]. 护士进修杂志,2015,30(11):964-967. DOI:10.16821/j.cnki.hsjx.2015.11.002.
|
| [16] |
Osteoporosis Australia. Osteoporosis prevention,diagnosis and management in postmenopausal women and men over 50 years of age[EB/OL]. [2022-02-27].
|
| [17] |
Scottish Intercollegiate Guidelines Network(SIGN). Management of osteoporosis and the prevention of fragility fractures[EB/OL]. [2022-02-27].
|
| [18] |
American College of Obstetricians and Gynecologists' Committee on Clinical Practice Guidelines-Gynecology. Osteoporosis prevention,screening,and diagnosis:ACOG clinical practice guideline No. 1[J]. Obstet Gynecol,2021,138(3):494-506. DOI:10.1097/AOG.0000000000004514.
|
| [19] |
中国康复医学会,兰州大学循证医学中心,中国康复研究中心康复信息研究所,等. 骨质疏松症康复指南(上)[J]. 中国康复医学杂志,2019,34(11):1265-1272. DOI:10.3969/j.issn.1001-1242.2019.11.001.
|
| [20] |
中国康复医学会,兰州大学循证医学中心,中国康复研究中心康复信息研究所,等. 骨质疏松症康复指南(下)[J]. 中国康复医学杂志,2019,34(12):1511-1519. DOI:10.3969/j.issn.1001-1242.2019.12.023.
|
| [21] |
|
| [22] |
|
| [23] |
|
| [24] |
|
| [25] |
|
| [26] |
中国营养学会骨营养与健康分会,中华医学会骨质疏松和骨矿盐疾病分会. 原发性骨质疏松症患者的营养和运动管理专家共识[J]. 中华内分泌代谢杂志,2020,36(8):643-653. DOI:10.3760/cma.j.cn311282-20200408-00261.
|
| [27] |
|
| [28] |
|
| [29] |
|
| [30] |
|
| [31] |
|
| [32] |
吴志建,王竹影,胡冰倩,等. 运动锻炼改善绝经后妇女骨密度效果的meta分析[J]. 中国康复医学杂志,2020,35(8):963-971. DOI:10.3969/j.issn.1001-1242.2020.08.015.
|
| [33] |
|
| [34] |
孙兢,包少瑜,张智海. FRAX在绝经后骨质疏松症中骨折风险评估的Meta分析[J]. 中国骨质疏松杂志,2021,27(12):1767-1773.
|
| [35] |
|
| [36] |
|
| [37] |
|
| [38] |
|
| [1] | 田晨, 刘佳宁, 田金徽, 葛龙. 动态系统评价制作方法与流程[J]. 中国全科医学, 2025, 28(30): 3853-3860. |
| [2] | 崔译元, 闫逸婧, 王颖, 孟祥聚, 张庆林, 刘丽星, 李思聪, 冯利, 癌因性疲乏中西医结合诊疗指南工作组. 癌因性疲乏中西医结合诊疗指南[J]. 中国全科医学, 2025, 28(27): 3345-3358. |
| [3] | 智从从, 李雪, 程一乘, 王孝龙, 郑丽华. 痔中西医结合诊疗指南(2025版)[J]. 中国全科医学, 2025, 28(26): 3217-3228. |
| [4] | 王颖, 颜轶隽, 刘蕾, 胡毓敏, 张扬, 刘凯, 姜博仁. 抗阻力运动联合营养干预对老年2型糖尿病合并肌少症患者血糖稳定性影响的临床研究[J]. 中国全科医学, 2025, 28(21): 2604-2610. |
| [5] | 马盼盼, 王思静, 游娜, 丁大法, 鲁一兵. Danuglipron与Orforglipron治疗2型糖尿病疗效及安全性的Meta分析[J]. 中国全科医学, 2025, 28(21): 2679-2685. |
| [6] | 文永霞, 孙海, 陈小菊, 蔡婉静, 李淑妮, 郭洪花. 孕产妇分娩心理创伤评估工具的系统评价[J]. 中国全科医学, 2025, 28(20): 2555-2561. |
| [7] | 杨江, 李建生, 陈耀龙, 刘辉国, 王建新, 喻佳洁, 李慧茹, 肖琼华, 谢洋, 李素云, 王明航. 中成药治疗成人社区获得性肺炎临床应用指南(2025版)[J]. 中国全科医学, 2025, 28(20): 2464-2480. |
| [8] | 曹沁涵, 卓肖, 夏雨菡, 车杨曦, 陈敏. 2024年V1/V2版《NCCN直肠癌临床实践指南》更新要点解读[J]. 中国全科医学, 2025, 28(17): 2070-2074. |
| [9] | 陈典, 隆寰宇, 张丛溪, 褚岚和, 李姝润, 陈亚红. 2025年GOLD慢性阻塞性肺疾病诊断、治疗、管理及预防全球策略更新要点解读[J]. 中国全科医学, 2025, 28(16): 1937-1949. |
| [10] | 章琪, 和申, 李华. 2022年美国预防临床服务指南工作组《儿童和青少年抑郁症和自杀风险筛查推荐声明》解读[J]. 中国全科医学, 2025, 28(15): 1823-1830. |
| [11] | 夏雨菡, 卓肖, 曹沁涵, 廖星雨, 罗国樑, 唐太春, 陈敏. 2024年V4版《NCCN结肠癌临床实践指南》更新解读[J]. 中国全科医学, 2025, 28(14): 1689-1693. |
| [12] | 马桂芬, 章倩, 孙菁. 2024年《NCCN胃癌临床实践指南》更新要点解读[J]. 中国全科医学, 2025, 28(14): 1681-1688. |
| [13] | 王晓雨, 冯贞贞, 王军, 郭小川, 李建生. 急性呼吸窘迫综合征患者并发急性肾损伤危险因素的系统评价[J]. 中国全科医学, 2025, 28(12): 1527-1537. |
| [14] | 孙清, 吴玉霄, 崔立敏. 中国2型糖尿病患者肌少-骨质疏松症患病率的Meta分析[J]. 中国全科医学, 2025, 28(12): 1520-1526. |
| [15] | 中国医师协会睡眠医学专业委员会, 中国医师协会神经内科医师分会睡眠学组. 中国成人失眠共病阻塞性睡眠呼吸暂停诊治指南(2024版)[J]. 中国全科医学, 2025, 28(11): 1289-1303. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





