中国全科医学 ›› 2023, Vol. 26 ›› Issue (31): 3963-3974.DOI: 10.12114/j.issn.1007-9572.2022.0707
• 论著·医学循证 • 上一篇
收稿日期:2022-09-29
修回日期:2023-05-20
出版日期:2023-11-05
发布日期:2023-07-06
通讯作者:
王芳
HE Jingyi1, WANG Fang2,*( ), SHUI Xiaoling1, LI Ling1, LIANG Qian1
), SHUI Xiaoling1, LI Ling1, LIANG Qian1
Received:2022-09-29
Revised:2023-05-20
Published:2023-11-05
Online:2023-07-06
Contact:
WANG Fang
摘要: 背景 失眠症状的出现会降低围绝经期女性生活质量,并且会增加其罹患其他疾病的风险。目前,可用于改善围绝经期失眠症状的非药物干预措施众多,何种干预措施效果最好尚有分歧。 目的 采用网状Meta分析方法评价非药物干预对改善围绝经期失眠症状的效果。 方法 于2022年3月,检索Cochrane Library、PubMed、EmBase、Web of Science、中国知网、万方数据知识服务平台、维普中文科技期刊全文数据库和中国生物医学文献数据库中关于非药物干预改善围绝经期失眠症状的随机对照试验(RCT),检索时限均为建库至2022年3月。在两名研究者独立筛选文献、提取数据,并采用Cochrane系统评价手册5.1.0推荐的RCT偏倚风险评估工具评价纳入文献的偏倚风险之后,采用R 4.1.3软件和GeMTC包对不同非药物干预措施下,围绝经期失眠症状改善的总有效率,以及匹兹堡睡眠质量指数量表(PSQI)评分、kupperman评分、雌二醇(E2)水平改善情况进行贝叶斯网状Meta分析。 结果 共纳入44项RCT,包括3 354例患者,涉及12种非药物干预措施(艾灸、电针、耳穴压豆、刮痧、火龙罐、揿针、推拿、温针、蜂针、穴位埋线、音乐疗法、针刺)。网状Meta分析结果显示:在改善围绝经期失眠症状的总有效率方面,艾灸、电针、针刺的效果优于镇静安眠西药(P<0.05),艾灸成为最佳干预措施的可能性最大。在改善PSQI评分方面,艾灸、电针、刮痧、针刺的效果优于镇静安眠西药(P<0.05),艾灸的效果优于温针(P<0.05),艾灸成为最佳干预措施的可能性最大。在改善kupperman评分方面,不同干预措施的效果比较,差异均无统计学意义(P>0.05),刮痧成为最佳干预措施的可能性最大。在改善E2水平方面,不同干预措施的效果比较,差异均无统计学意义(P>0.05),针刺成为最佳干预措施的可能性最大。 结论 当前证据显示,对于围绝经期女性而言,艾灸在改善失眠症状总有效率和PSQI评分,刮痧在改善kupperman评分,针刺在提高E2水平方面具有优势,但还需要通过开展更多高质量的研究进一步验证此结论。
| 作者 | 发表年份(年) | 国家 | 样本量 | 平均年龄( | 平均病程( | 干预措施 | 干预时长 | 结局指标 |
|---|---|---|---|---|---|---|---|---|
| 刘航等[ | 2022 | 中国 | T1:30 | 49.2±2.3 | 12.6±6.1 | 艾灸 | 4周 | ①② |
| T2:30 | 49.4±2.3 | 12.5±6.0 | 针刺 | |||||
| C:30 | 49.0±2.5 | 12.5±5.8 | 镇静安眠西药 | |||||
| 李佳[ | 2012 | 中国 | T:29 | 50.00±3.94 | 4.41±2.89 | 艾灸 | 2周 | ①② |
| C:29 | 50.07±4.17 | 4.55±2.26 | 镇静安眠西药 | |||||
| 陈秀玲等[ | 2011 | 中国 | T:38 | 48±6 | 6.9±0.2 | 电针 | 5周 | ① |
| C:32 | 48±7 | 6.5±0.3 | 镇静安眠西药 | |||||
| 柯庆宗[ | 2015 | 中国 | T:45 | 50.04±2.67 | 13.36±7.47 | 电针 | 4周 | ①② |
| C:45 | 50.04±2.96 | 13.51±7.76 | 镇静安眠西药 | |||||
| 王婉娣[ | 2015 | 中国 | T:30 | 49.80±3.55 | 19.47±7.65 | 电针 | 8周 | ② |
| C:30 | 49.53±3.03 | 17.5±9.0 | 安慰剂针刺 | |||||
| LI等[ | 2020 | 中国 | T:40 | 52.12±4.19 | — | 电针 | 8周 | ② |
| C:41 | 53.07±3.81 | 安慰剂针刺 | ||||||
| 师维[ | 2017 | 中国 | T:32 | 46.66±4.88 | 20.42±17.07 | 电针 | 4周 | ② |
| C:30 | 48.00±4.55 | 29.85±21.80 | 针刺 | |||||
| 于心同等[ | 2022 | 中国 | T:30 | 49.7±3.2 | 12.2±4.7 | 电针 | 4周 | ①②③ |
| C:30 | 48.8±3.4 | 11.6±4.5 | 安慰剂针刺 | |||||
| 贾美君等[ | 2018 | 中国 | T:32 | 53.56±6.35 | — | 耳穴压豆 | 8周 | ② |
| C:32 | 54.22±5.22 | 镇静安眠西药 | ||||||
| 杨松柏等[ | 2013 | 中国 | T:32 | — | — | 耳穴压豆 | 4周 | ①② |
| C:32 | 针刺 | |||||||
| 陈丽兰等[ | 2021 | 中国 | T:30 | 51.22±2.24 | 11.59±8.54 | 刮痧 | 4周 | ①② |
| C:30 | 50.37±2.83 | 10.38±7.75 | 镇静安眠西药 | |||||
| 彭德忠等[ | 2014 | 中国 | T:57 | — | — | 刮痧 | 12周 | ② |
| C:57 | 镇静安眠西药 | |||||||
| 王子岳[ | 2015 | 中国 | T:42 | — | 18.13±9.15 | 刮痧 | 4周 | ①② |
| C:41 | 17.90±9.74 | 镇静安眠西药 | ③④ | |||||
| 杨娟[ | 2020 | 中国 | T:20 | 51.62±2.80 | — | 刮痧 | 4周 | ② |
| C:20 | 52.14±2.60 | 镇静安眠西药 | ||||||
| 施兰来等[ | 2021 | 中国 | T:35 | 48.83±2.31 | 7.11±1.89 | 火龙罐 | 4周 | ① |
| C:34 | 49.82±2.83 | 7.53±1.64 | 针刺 | |||||
| 陈阳等[ | 2021 | 中国 | T:30 | 50.6±2.2 | — | 揿针 | 2周 | ①② |
| C:30 | 51.2±3.0 | 镇静安眠西药 | ||||||
| 李清玲[ | 2017 | 中国 | T:52 | — | — | 揿针 | 30 d | ①② |
| C:52 | 针刺 | |||||||
| 高亮[ | 2016 | 中国 | T:24 | 55.0±3.5 | 4.13±2.65 | 推拿 | 12周 | ① |
| C:24 | 54.7±4.7 | 4.49±2.71 | 镇静安眠西药 | |||||
| 王艺晴[ | 2018 | 中国 | T:28 | 50.43±2.56 | 24.18±13.89 | 推拿 | 8周 | ①② |
| C:29 | 49.86±2.92 | 22.62±17.66 | 镇静安眠西药 | |||||
| 王甜[ | 2018 | 中国 | T:30 | 49.60±3.31 | 5.33±3.00 | 温针 | 16周 | ①②③ |
| C:30 | 50.13±3.00 | 5.27±3.11 | 针刺 | |||||
| 崔威等[ | 2017 | 中国 | T:35 | — | — | 无痛蜂针疗法 | 4周 | ①② |
| C:35 | 镇静安眠西药 | |||||||
| 韩慧等[ | 2020 | 中国 | T:30 | 49.52±5.81 | 8.92±3.68 | 穴位埋线 | 4周 | ①②④ |
| C:30 | 48.92±5.02 | 9.57±3.19 | 针刺 | |||||
| 李霞等[ | 2019 | 中国 | T:25 | 49.93±3.22 | — | 穴位埋线 | 4周 | ① |
| C:25 | 50.04±3.01 | 镇静安眠西药 | ||||||
| 刘志霞等[ | 2014 | 中国 | T:40 | 49.8±6.3 | 5.5±4.1 | 穴位埋线 | 4周 | ① |
| C:40 | 49.6±6.4 | 5.4±4.2 | 镇静安眠西药 | |||||
| 俞鑫佳等[ | 2015 | 中国 | T:30 | 50±5 | 9.40±4.12 | 穴位埋线 | 3周 | ①② |
| C:30 | 48±5 | 9.77±5.28 | 针刺 | |||||
| 王苑等[ | 2020 | 中国 | T:32 | 47.8±6.7 | — | 音乐疗法 | 15 d | ① |
| C:31 | 48.6±5.9 | 空白对照 | ||||||
| ZHAO等[ | 2019 | 中国 | T:24 | 51.04±3.29 | 11.95±6.41 | 针刺 | 8周 | ②④ |
| C:25 | 49.64±3.55 | 12.15±5.71 | 安慰剂针刺 | |||||
| 郭琴[ | 2021 | 中国 | T:30 | — | — | 针刺 | 8周 | ①② |
| C:30 | 镇静安眠西药 | ③④ | ||||||
| 黄文雄等[ | 2021 | 中国 | T:45 | 50.8±4.1 | 12.1±3.7 | 针刺 | 8周 | ②③④ |
| C:45 | 50.2±4.3 | 11.7±3.8 | 镇静安眠西药 | |||||
| 李泓等[ | 2016 | 中国 | T1:30 | 58.63±5.28 | 34.03±14.33 | 针刺 | 4周 | ①③ |
| T2:30 | 58.87±5.01 | 34.17±14.27 | 电针 | |||||
| C:30 | 58.93±5.11 | 34.63±14.28 | 温针 | |||||
| 李欧静等[ | 2018 | 中国 | T:60 | 51±4 | 11.2±5.2 | 针刺 | 9周 | ①②④ |
| C:62 | 50±4 | 10.2±5.3 | 镇静安眠西药 | |||||
| 李亚男[ | 2014 | 中国 | T:120 | — | — | 针刺 | 4周 | ① |
| C:120 | 镇静安眠西药 | |||||||
| 林文馨等[ | 2017 | 中国 | T:33 | 50±3 | 14.16±13.08 | 针刺 | 4周 | ①②③ |
| C:32 | 50±3 | 14.63±10.83 | 空白对照 | |||||
| 秦媛媛[ | 2018 | 中国 | T:34 | 51.97±2.27 | 18.44±7.55 | 针刺 | 4周 | ①② |
| C:33 | 50.85±2.77 | 20.58±9.25 | 镇静安眠西药 | |||||
| 王延玉[ | 2017 | 中国 | T:28 | 50.28±2.32 | — | 针刺 | 4周 | ② |
| C:28 | 50.37±2.31 | 镇静安眠西药 | ||||||
| 向华平[ | 2020 | 中国 | T:56 | 48.8±5.8 | 11.2±5.3 | 针刺 | 9周 | ①②④ |
| C:56 | 49.2±6.1 | 10.3±5.1 | 镇静安眠西药 | |||||
| 杨继若等[ | 2017 | 中国 | T:81 | 48.17±4.12 | 7.13±1.96 | 针刺 | 12周 | ①②④ |
| C:81 | 49.45±3.98 | 7.53±2.11 | 镇静安眠西药 | |||||
| 杨玉婷[ | 2021 | 中国 | T:30 | 50.08±2.17 | — | 针刺 | 4周 | ①② |
| C:30 | 50.12±2.26 | 镇静安眠西药 | ||||||
| 张婉容等[ | 2019 | 中国 | T:29 | 49.3±4.2 | 7.9±3.7 | 针刺 | 20 d | ① |
| C:28 | 50.7±5.4 | 8.1±3.9 | 艾灸 | |||||
| 张巍等[ | 2017 | 中国 | T:31 | 50.45±3.50 | 20.38±20.53 | 针刺 | 4周 | ①②③ |
| C:30 | 48.97±2.88 | 20.36±20.44 | 镇静安眠西药 | |||||
| FU等[ | 2017 | 中国 | T:37 | 52.0±5.3 | — | 针刺 | 4周 | ② |
| C:37 | 52.5±5.9 | 安慰剂针刺 | ||||||
| 纪峰[ | 2008 | 中国 | T:30 | — | — | 针刺 | 12周 | ①② |
| C:30 | 镇静安眠西药 | |||||||
| 卢晨等[ | 2014 | 中国 | T:52 | — | — | 针刺 | 30 d | ①② |
| C:52 | 镇静安眠西药 | |||||||
| 孙枚等[ | 2016 | 中国 | T:24 | 52.32±1.63 | — | 针刺 | 12周 | ①④ |
| C:24 | 51.24±1.36 | 镇静安眠西药 |
表1 纳入文献的基本特征
Table 1 Basic characteristics of included studies
| 作者 | 发表年份(年) | 国家 | 样本量 | 平均年龄( | 平均病程( | 干预措施 | 干预时长 | 结局指标 |
|---|---|---|---|---|---|---|---|---|
| 刘航等[ | 2022 | 中国 | T1:30 | 49.2±2.3 | 12.6±6.1 | 艾灸 | 4周 | ①② |
| T2:30 | 49.4±2.3 | 12.5±6.0 | 针刺 | |||||
| C:30 | 49.0±2.5 | 12.5±5.8 | 镇静安眠西药 | |||||
| 李佳[ | 2012 | 中国 | T:29 | 50.00±3.94 | 4.41±2.89 | 艾灸 | 2周 | ①② |
| C:29 | 50.07±4.17 | 4.55±2.26 | 镇静安眠西药 | |||||
| 陈秀玲等[ | 2011 | 中国 | T:38 | 48±6 | 6.9±0.2 | 电针 | 5周 | ① |
| C:32 | 48±7 | 6.5±0.3 | 镇静安眠西药 | |||||
| 柯庆宗[ | 2015 | 中国 | T:45 | 50.04±2.67 | 13.36±7.47 | 电针 | 4周 | ①② |
| C:45 | 50.04±2.96 | 13.51±7.76 | 镇静安眠西药 | |||||
| 王婉娣[ | 2015 | 中国 | T:30 | 49.80±3.55 | 19.47±7.65 | 电针 | 8周 | ② |
| C:30 | 49.53±3.03 | 17.5±9.0 | 安慰剂针刺 | |||||
| LI等[ | 2020 | 中国 | T:40 | 52.12±4.19 | — | 电针 | 8周 | ② |
| C:41 | 53.07±3.81 | 安慰剂针刺 | ||||||
| 师维[ | 2017 | 中国 | T:32 | 46.66±4.88 | 20.42±17.07 | 电针 | 4周 | ② |
| C:30 | 48.00±4.55 | 29.85±21.80 | 针刺 | |||||
| 于心同等[ | 2022 | 中国 | T:30 | 49.7±3.2 | 12.2±4.7 | 电针 | 4周 | ①②③ |
| C:30 | 48.8±3.4 | 11.6±4.5 | 安慰剂针刺 | |||||
| 贾美君等[ | 2018 | 中国 | T:32 | 53.56±6.35 | — | 耳穴压豆 | 8周 | ② |
| C:32 | 54.22±5.22 | 镇静安眠西药 | ||||||
| 杨松柏等[ | 2013 | 中国 | T:32 | — | — | 耳穴压豆 | 4周 | ①② |
| C:32 | 针刺 | |||||||
| 陈丽兰等[ | 2021 | 中国 | T:30 | 51.22±2.24 | 11.59±8.54 | 刮痧 | 4周 | ①② |
| C:30 | 50.37±2.83 | 10.38±7.75 | 镇静安眠西药 | |||||
| 彭德忠等[ | 2014 | 中国 | T:57 | — | — | 刮痧 | 12周 | ② |
| C:57 | 镇静安眠西药 | |||||||
| 王子岳[ | 2015 | 中国 | T:42 | — | 18.13±9.15 | 刮痧 | 4周 | ①② |
| C:41 | 17.90±9.74 | 镇静安眠西药 | ③④ | |||||
| 杨娟[ | 2020 | 中国 | T:20 | 51.62±2.80 | — | 刮痧 | 4周 | ② |
| C:20 | 52.14±2.60 | 镇静安眠西药 | ||||||
| 施兰来等[ | 2021 | 中国 | T:35 | 48.83±2.31 | 7.11±1.89 | 火龙罐 | 4周 | ① |
| C:34 | 49.82±2.83 | 7.53±1.64 | 针刺 | |||||
| 陈阳等[ | 2021 | 中国 | T:30 | 50.6±2.2 | — | 揿针 | 2周 | ①② |
| C:30 | 51.2±3.0 | 镇静安眠西药 | ||||||
| 李清玲[ | 2017 | 中国 | T:52 | — | — | 揿针 | 30 d | ①② |
| C:52 | 针刺 | |||||||
| 高亮[ | 2016 | 中国 | T:24 | 55.0±3.5 | 4.13±2.65 | 推拿 | 12周 | ① |
| C:24 | 54.7±4.7 | 4.49±2.71 | 镇静安眠西药 | |||||
| 王艺晴[ | 2018 | 中国 | T:28 | 50.43±2.56 | 24.18±13.89 | 推拿 | 8周 | ①② |
| C:29 | 49.86±2.92 | 22.62±17.66 | 镇静安眠西药 | |||||
| 王甜[ | 2018 | 中国 | T:30 | 49.60±3.31 | 5.33±3.00 | 温针 | 16周 | ①②③ |
| C:30 | 50.13±3.00 | 5.27±3.11 | 针刺 | |||||
| 崔威等[ | 2017 | 中国 | T:35 | — | — | 无痛蜂针疗法 | 4周 | ①② |
| C:35 | 镇静安眠西药 | |||||||
| 韩慧等[ | 2020 | 中国 | T:30 | 49.52±5.81 | 8.92±3.68 | 穴位埋线 | 4周 | ①②④ |
| C:30 | 48.92±5.02 | 9.57±3.19 | 针刺 | |||||
| 李霞等[ | 2019 | 中国 | T:25 | 49.93±3.22 | — | 穴位埋线 | 4周 | ① |
| C:25 | 50.04±3.01 | 镇静安眠西药 | ||||||
| 刘志霞等[ | 2014 | 中国 | T:40 | 49.8±6.3 | 5.5±4.1 | 穴位埋线 | 4周 | ① |
| C:40 | 49.6±6.4 | 5.4±4.2 | 镇静安眠西药 | |||||
| 俞鑫佳等[ | 2015 | 中国 | T:30 | 50±5 | 9.40±4.12 | 穴位埋线 | 3周 | ①② |
| C:30 | 48±5 | 9.77±5.28 | 针刺 | |||||
| 王苑等[ | 2020 | 中国 | T:32 | 47.8±6.7 | — | 音乐疗法 | 15 d | ① |
| C:31 | 48.6±5.9 | 空白对照 | ||||||
| ZHAO等[ | 2019 | 中国 | T:24 | 51.04±3.29 | 11.95±6.41 | 针刺 | 8周 | ②④ |
| C:25 | 49.64±3.55 | 12.15±5.71 | 安慰剂针刺 | |||||
| 郭琴[ | 2021 | 中国 | T:30 | — | — | 针刺 | 8周 | ①② |
| C:30 | 镇静安眠西药 | ③④ | ||||||
| 黄文雄等[ | 2021 | 中国 | T:45 | 50.8±4.1 | 12.1±3.7 | 针刺 | 8周 | ②③④ |
| C:45 | 50.2±4.3 | 11.7±3.8 | 镇静安眠西药 | |||||
| 李泓等[ | 2016 | 中国 | T1:30 | 58.63±5.28 | 34.03±14.33 | 针刺 | 4周 | ①③ |
| T2:30 | 58.87±5.01 | 34.17±14.27 | 电针 | |||||
| C:30 | 58.93±5.11 | 34.63±14.28 | 温针 | |||||
| 李欧静等[ | 2018 | 中国 | T:60 | 51±4 | 11.2±5.2 | 针刺 | 9周 | ①②④ |
| C:62 | 50±4 | 10.2±5.3 | 镇静安眠西药 | |||||
| 李亚男[ | 2014 | 中国 | T:120 | — | — | 针刺 | 4周 | ① |
| C:120 | 镇静安眠西药 | |||||||
| 林文馨等[ | 2017 | 中国 | T:33 | 50±3 | 14.16±13.08 | 针刺 | 4周 | ①②③ |
| C:32 | 50±3 | 14.63±10.83 | 空白对照 | |||||
| 秦媛媛[ | 2018 | 中国 | T:34 | 51.97±2.27 | 18.44±7.55 | 针刺 | 4周 | ①② |
| C:33 | 50.85±2.77 | 20.58±9.25 | 镇静安眠西药 | |||||
| 王延玉[ | 2017 | 中国 | T:28 | 50.28±2.32 | — | 针刺 | 4周 | ② |
| C:28 | 50.37±2.31 | 镇静安眠西药 | ||||||
| 向华平[ | 2020 | 中国 | T:56 | 48.8±5.8 | 11.2±5.3 | 针刺 | 9周 | ①②④ |
| C:56 | 49.2±6.1 | 10.3±5.1 | 镇静安眠西药 | |||||
| 杨继若等[ | 2017 | 中国 | T:81 | 48.17±4.12 | 7.13±1.96 | 针刺 | 12周 | ①②④ |
| C:81 | 49.45±3.98 | 7.53±2.11 | 镇静安眠西药 | |||||
| 杨玉婷[ | 2021 | 中国 | T:30 | 50.08±2.17 | — | 针刺 | 4周 | ①② |
| C:30 | 50.12±2.26 | 镇静安眠西药 | ||||||
| 张婉容等[ | 2019 | 中国 | T:29 | 49.3±4.2 | 7.9±3.7 | 针刺 | 20 d | ① |
| C:28 | 50.7±5.4 | 8.1±3.9 | 艾灸 | |||||
| 张巍等[ | 2017 | 中国 | T:31 | 50.45±3.50 | 20.38±20.53 | 针刺 | 4周 | ①②③ |
| C:30 | 48.97±2.88 | 20.36±20.44 | 镇静安眠西药 | |||||
| FU等[ | 2017 | 中国 | T:37 | 52.0±5.3 | — | 针刺 | 4周 | ② |
| C:37 | 52.5±5.9 | 安慰剂针刺 | ||||||
| 纪峰[ | 2008 | 中国 | T:30 | — | — | 针刺 | 12周 | ①② |
| C:30 | 镇静安眠西药 | |||||||
| 卢晨等[ | 2014 | 中国 | T:52 | — | — | 针刺 | 30 d | ①② |
| C:52 | 镇静安眠西药 | |||||||
| 孙枚等[ | 2016 | 中国 | T:24 | 52.32±1.63 | — | 针刺 | 12周 | ①④ |
| C:24 | 51.24±1.36 | 镇静安眠西药 |
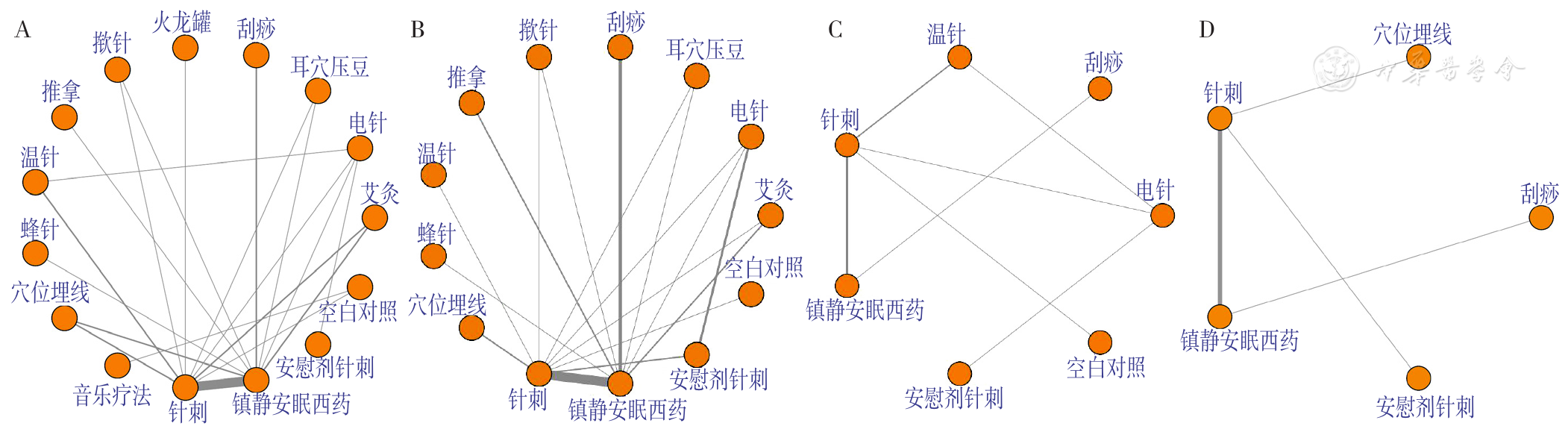
图3 不同结局指标下各干预措施间的网状关系注:PSQI=匹兹堡睡眠质量指数量表,E2=雌二醇;A表示基于围绝经期失眠症状改善总有效率的各干预措施间的网状关系图,B表示基于PSQI评分改善情况的各干预措施间的网状关系图,C表示基于kupperman评分改善情况的各干预措施间的网状关系图,D表示基于E2水平改善情况的各干预措施间的网状关系图。每个圆点表示1种干预措施,圆点与圆点之间的连线表示干预措施之间存在被直接比较的情况,连线越粗表示对两干预措施进行直接比较的研究越多。
Figure 3 Network diagram of each intervention under different outcome indicators
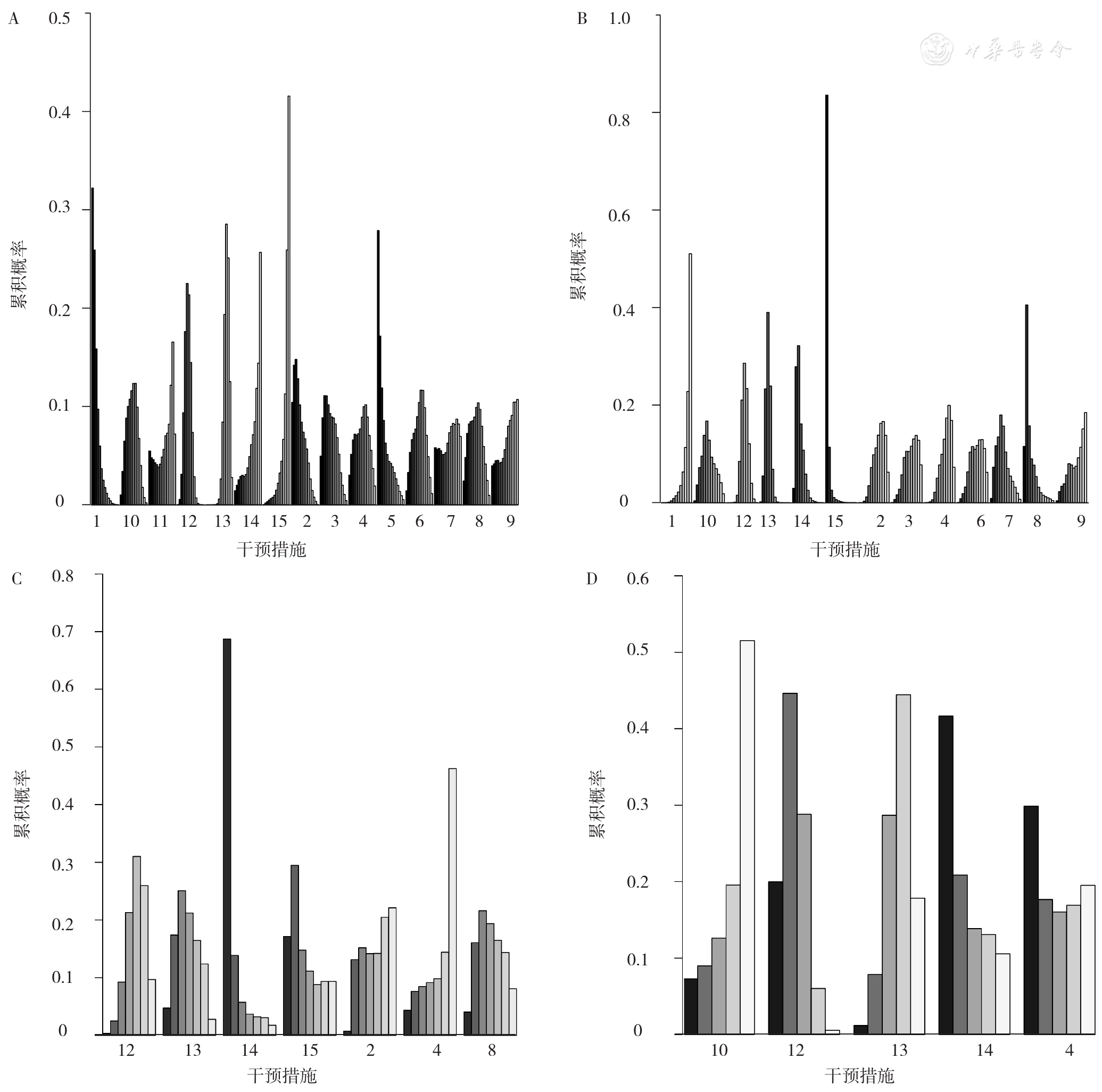
图4 非药物干预对改善围绝经期失眠症状效果的累积概率排序注:1表示艾灸,2表示电针,3表示耳穴压豆,4表示刮痧,5表示火龙罐,6表示揿针,7表示推拿,8表示温针,9表示蜂针,10表示穴位埋线,11表示音乐疗法,12表示针刺,13表示镇静安眠西药,14表示安慰剂针刺,15表示空白对照;A表示基于围绝经期失眠症状改善总有效率的累积概率排序图,B表示基于PSQI评分改善情况的累积概率排序图,C表示基于kupperman评分改善情况的累积概率排序图,D表示基于E2水平改善情况的累积概率排序图。
Figure 4 Cumulative probability ranking of the efficacy of nonpharmacological interventions on improving perimenopausal insomnia symptoms
| 干预措施 | 艾灸 | 电针 | 耳穴压豆 | 刮痧 | 火龙罐 | 揿针 | 推拿 | |
|---|---|---|---|---|---|---|---|---|
| 艾灸 | — | — | — | — | — | — | — | |
| 电针 | 2.17(0.16,29.80) | — | — | — | — | — | — | |
| 耳穴压豆 | 3.09(0.26,39.90) | 1.43(0.09,22.58) | — | — | — | — | — | |
| 刮痧 | 4.99(0.34,77.77) | 2.31(0.13,43.14) | 1.61(0.10,28.12) | — | — | — | — | |
| 火龙罐 | 1.38(0.06,33.16) | 0.63(0.02,18.45) | 0.44(0.02,11.72) | 0.28(0.01,8.82) | — | — | — | |
| 揿针 | 5.26(0.46,65.39) | 2.42(0.17,37.29) | 1.69(0.13,23.35) | 1.05(0.06,17.31) | 3.80(0.15,99.44) | — | — | |
| 推拿 | 6.57(0.20,197.72) | 3.02(0.08,107.36) | 2.10(0.06,68.14) | 1.31(0.03,46.51) | 4.72(0.08,261.56) | 1.25(0.03,38.09) | — | |
| 温针 | 4.44(0.35,63.20) | 2.03(0.18,25.69) | 1.43(0.10,22.50) | 0.89(0.05,17.19) | 3.23(0.12,94.93) | 0.85(0.06,12.39) | 0.68(0.02,27.18) | |
| 蜂针 | 8.98(0.28,291.43) | 4.16(0.11,154.03) | 2.88(0.08,98.81) | 1.78(0.04,71.26) | 6.51(0.11,393.10) | 1.70(0.05,57.99) | 1.37(0.02,99.95) | |
| 穴位埋线 | 4.13(0.49,38.76) | 1.90(0.18,22.67) | 1.33(0.13,14.15) | 0.83(0.06,11.02) | 3.01(0.15,65.60) | 0.78(0.08,7.84) | 0.63(0.03,18.64) | |
| 音乐疗法 | 9.94(0.18,547.82) | 4.59(0.07,300.54) | 3.21(0.05,184.35) | 1.99(0.03,137.43) | 7.18(0.08,632.03) | 1.90(0.03,105.35) | 1.52(0.01,183.22) | |
| 针刺 | 3.40(0.65,19.82) | 1.56(0.22,12.33) | 1.09(0.16,7.59) | 0.68 (0.07,6.45) | 2.46(0.17,36.97) | 0.65 (0.10,4.03) | 0.52(0.03,12.04) | |
| 镇静安眠西药 | 15.12(2.92,93.26)a | 6.95(1.01,56.64)a | 4.91(0.75,34.86) | 3.03(0.39,26.65) | 11.05(0.73,185.33) | 2.90 (0.47,18.80) | 2.32(0.13,50.94) | |
| 安慰剂针刺 | 18.66(0.42,959.87) | 8.51(0.56,155.75) | 6.02(0.12,319.48) | 3.74(0.07,222.57) | 13.68(0.17,1 152.46) | 3.56(0.07,180.16) | 2.87(0.03,295.99) | |
| 空白对照 | 41.14(1.89,941.27)a | 19.13(0.74,519.03) | 13.25(0.53,335.58) | 8.26(0.28,253.09) | 30.09(0.75,1 270.73) | 7.85(0.34,192.14) | 6.29(0.12,371.78) | |
| 干预措施 | 温针 | 蜂针 | 穴位埋线 | 音乐疗法 | 针刺 | 镇静安眠西药 | 安慰剂针刺 | 空白对照 |
| 艾灸 | — | — | — | — | — | — | — | — |
| 电针 | — | — | — | — | — | — | — | — |
| 耳穴压豆 | — | — | — | — | — | — | — | — |
| 刮痧 | — | — | — | — | — | — | — | — |
| 火龙罐 | — | — | — | — | — | — | — | — |
| 揿针 | — | — | — | — | — | — | — | — |
| 推拿 | — | — | — | — | — | — | — | — |
| 温针 | — | — | — | — | — | — | — | — |
| 蜂针 | 2.02(0.05,71.82) | — | — | — | — | — | — | — |
| 穴位埋线 | 0.93(0.08,10.41) | 0.46 (0.02,13.33) | — | — | — | — | — | — |
| 音乐疗法 | 2.23(0.04,131.77) | 1.11 (0.01,127.32) | 2.40 (0.05,114.79) | — | — | — | — | — |
| 针刺 | 0.77(0.10,5.27) | 0.38 (0.02,8.75) | 0.82 (0.19,3.49) | 0.35 (0.01,12.69) | — | — | — | — |
| 镇静安眠西药 | 3.45(0.44,26.84) | 1.70(0.09,36.11) | 3.68 (0.87,16.13) | 1.55 (0.04,62.20) | 4.46 (2.26,9.25)a | — | — | — |
| 安慰剂针刺 | 4.22(0.10,185.38) | 2.09(0.02,210.41) | 4.49(0.11,196.99) | 1.91(0.01,287.27) | 5.45(0.18,187.71) | 1.23(0.04,41.14) | — | — |
| 空白对照 | 9.31(0.35,228.23) | 4.63(0.08,269.95) | 10.01(0.51,191.03) | 4.18(0.34,51.79) | 12.02(0.94,161.32) | 2.70(0.18,39.19) | 2.21(0.03,164.99) | — |
表2 基于围绝经期失眠症状改善总有效率的网状Meta分析结果〔OR(95%CI)〕
Table 2 Results of network meta-analysis based on total response rate of improvement in perimenopausal insomnia symptoms
| 干预措施 | 艾灸 | 电针 | 耳穴压豆 | 刮痧 | 火龙罐 | 揿针 | 推拿 | |
|---|---|---|---|---|---|---|---|---|
| 艾灸 | — | — | — | — | — | — | — | |
| 电针 | 2.17(0.16,29.80) | — | — | — | — | — | — | |
| 耳穴压豆 | 3.09(0.26,39.90) | 1.43(0.09,22.58) | — | — | — | — | — | |
| 刮痧 | 4.99(0.34,77.77) | 2.31(0.13,43.14) | 1.61(0.10,28.12) | — | — | — | — | |
| 火龙罐 | 1.38(0.06,33.16) | 0.63(0.02,18.45) | 0.44(0.02,11.72) | 0.28(0.01,8.82) | — | — | — | |
| 揿针 | 5.26(0.46,65.39) | 2.42(0.17,37.29) | 1.69(0.13,23.35) | 1.05(0.06,17.31) | 3.80(0.15,99.44) | — | — | |
| 推拿 | 6.57(0.20,197.72) | 3.02(0.08,107.36) | 2.10(0.06,68.14) | 1.31(0.03,46.51) | 4.72(0.08,261.56) | 1.25(0.03,38.09) | — | |
| 温针 | 4.44(0.35,63.20) | 2.03(0.18,25.69) | 1.43(0.10,22.50) | 0.89(0.05,17.19) | 3.23(0.12,94.93) | 0.85(0.06,12.39) | 0.68(0.02,27.18) | |
| 蜂针 | 8.98(0.28,291.43) | 4.16(0.11,154.03) | 2.88(0.08,98.81) | 1.78(0.04,71.26) | 6.51(0.11,393.10) | 1.70(0.05,57.99) | 1.37(0.02,99.95) | |
| 穴位埋线 | 4.13(0.49,38.76) | 1.90(0.18,22.67) | 1.33(0.13,14.15) | 0.83(0.06,11.02) | 3.01(0.15,65.60) | 0.78(0.08,7.84) | 0.63(0.03,18.64) | |
| 音乐疗法 | 9.94(0.18,547.82) | 4.59(0.07,300.54) | 3.21(0.05,184.35) | 1.99(0.03,137.43) | 7.18(0.08,632.03) | 1.90(0.03,105.35) | 1.52(0.01,183.22) | |
| 针刺 | 3.40(0.65,19.82) | 1.56(0.22,12.33) | 1.09(0.16,7.59) | 0.68 (0.07,6.45) | 2.46(0.17,36.97) | 0.65 (0.10,4.03) | 0.52(0.03,12.04) | |
| 镇静安眠西药 | 15.12(2.92,93.26)a | 6.95(1.01,56.64)a | 4.91(0.75,34.86) | 3.03(0.39,26.65) | 11.05(0.73,185.33) | 2.90 (0.47,18.80) | 2.32(0.13,50.94) | |
| 安慰剂针刺 | 18.66(0.42,959.87) | 8.51(0.56,155.75) | 6.02(0.12,319.48) | 3.74(0.07,222.57) | 13.68(0.17,1 152.46) | 3.56(0.07,180.16) | 2.87(0.03,295.99) | |
| 空白对照 | 41.14(1.89,941.27)a | 19.13(0.74,519.03) | 13.25(0.53,335.58) | 8.26(0.28,253.09) | 30.09(0.75,1 270.73) | 7.85(0.34,192.14) | 6.29(0.12,371.78) | |
| 干预措施 | 温针 | 蜂针 | 穴位埋线 | 音乐疗法 | 针刺 | 镇静安眠西药 | 安慰剂针刺 | 空白对照 |
| 艾灸 | — | — | — | — | — | — | — | — |
| 电针 | — | — | — | — | — | — | — | — |
| 耳穴压豆 | — | — | — | — | — | — | — | — |
| 刮痧 | — | — | — | — | — | — | — | — |
| 火龙罐 | — | — | — | — | — | — | — | — |
| 揿针 | — | — | — | — | — | — | — | — |
| 推拿 | — | — | — | — | — | — | — | — |
| 温针 | — | — | — | — | — | — | — | — |
| 蜂针 | 2.02(0.05,71.82) | — | — | — | — | — | — | — |
| 穴位埋线 | 0.93(0.08,10.41) | 0.46 (0.02,13.33) | — | — | — | — | — | — |
| 音乐疗法 | 2.23(0.04,131.77) | 1.11 (0.01,127.32) | 2.40 (0.05,114.79) | — | — | — | — | — |
| 针刺 | 0.77(0.10,5.27) | 0.38 (0.02,8.75) | 0.82 (0.19,3.49) | 0.35 (0.01,12.69) | — | — | — | — |
| 镇静安眠西药 | 3.45(0.44,26.84) | 1.70(0.09,36.11) | 3.68 (0.87,16.13) | 1.55 (0.04,62.20) | 4.46 (2.26,9.25)a | — | — | — |
| 安慰剂针刺 | 4.22(0.10,185.38) | 2.09(0.02,210.41) | 4.49(0.11,196.99) | 1.91(0.01,287.27) | 5.45(0.18,187.71) | 1.23(0.04,41.14) | — | — |
| 空白对照 | 9.31(0.35,228.23) | 4.63(0.08,269.95) | 10.01(0.51,191.03) | 4.18(0.34,51.79) | 12.02(0.94,161.32) | 2.70(0.18,39.19) | 2.21(0.03,164.99) | — |
| 干预措施 | 艾灸 | 电针 | 耳穴压豆 | 刮痧 | 揿针 | 推拿 | |
|---|---|---|---|---|---|---|---|
| 艾灸 | — | — | — | — | — | — | |
| 电针 | -1.81(-5.57,1.93) | — | — | — | — | — | |
| 耳穴压豆 | -1.97(-6.10,2.17) | -0.17(-4.05,3.76) | — | — | — | — | |
| 刮痧 | -1.58(-5.11,2.00) | 0.23(-3.10,3.62) | 0.40(-3.38,4.18) | — | — | — | |
| 揿针 | -2.13(-6.25,1.97) | -0.32(-4.19,3.55) | -0.14(-4.43,4.10) | -0.55(-4.32,3.16) | — | — | |
| 推拿 | -3.79(-7.92,0.33) | -1.97(-5.95,2.00) | -1.80(-6.18,2.53) | -2.21(-5.97,1.53) | -1.66(-5.96,2.66) | — | |
| 温针 | -5.85(-11.07,-0.62)a | -4.04(-9.04,0.97) | -3.87(-9.24,1.47) | -4.27(-9.28,0.70) | -3.72(-9.04,1.61) | -2.06(-7.51,3.38) | |
| 蜂针 | -1.68(-6.91,3.53) | 0.13(-4.95,5.22) | 0.30(-5.07,5.65) | -0.10(-5.03,4.77) | 0.45(-4.92,5.80) | 2.10(-3.23,7.45) | |
| 穴位埋线 | -3.20(-7.42,1.02) | -1.39(-5.29,2.56) | -1.22(-5.58,3.12) | -1.62(-5.56,2.28) | -1.07(-5.37,3.26) | 0.59(-3.87,5.07) | |
| 针刺 | -2.42(-5.33,0.49) | -0.61(-3.07,1.86) | -0.44(-3.54,2.65) | -0.85(-3.33,1.60) | -0.30(-3.35,2.77) | 1.36(-1.89,4.61) | |
| 镇静安眠西药 | -4.62(-7.44,-1.81)a | -2.82(-5.36,-0.25)a | -2.65(-5.75,0.44) | -3.05(-5.24,-0.89)a | -2.50(-5.54,0.57) | -0.84(-3.87,2.19) | |
| 安慰剂针刺 | -5.28(-9.05,-1.53)a | -3.48(-5.66,-1.31)a | -3.31(-7.24,0.60) | -3.71(-7.15,-0.33)a | -3.16(-7.06,0.74) | -1.50(-5.53,2.49) | |
| 空白对照 | -9.30(-14.55,-4.06)a | -7.50(-12.50,-2.45)a | -7.33(-12.69,-1.97)a | -7.72(-12.76,-2.70)a | -7.17(-12.49,-1.84)a | -5.51(-10.98,-0.07)a | |
| 干预措施 | 温针 | 蜂针 | 穴位埋线 | 针刺 | 镇静安眠西药 | 安慰剂针刺 | 空白对照 |
| 艾灸 | — | — | — | — | — | — | — |
| 电针 | — | — | — | — | — | — | — |
| 耳穴压豆 | — | — | — | — | — | — | — |
| 刮痧 | — | — | — | — | — | — | — |
| 揿针 | — | — | — | — | — | — | — |
| 推拿 | — | — | — | — | — | — | — |
| 温针 | — | — | — | — | — | — | — |
| 蜂针 | 4.17(-2.11,10.47) | — | — | — | — | — | — |
| 穴位埋线 | 2.65 (-2.68,7.96) | -1.51(-6.98,3.96) | — | — | — | — | — |
| 针刺 | 3.43(-0.93,7.77) | -0.75(-5.28,3.82) | 0.77(-2.27,3.83) | — | — | — | — |
| 镇静安眠西药 | 1.22(-3.29,5.74) | -2.95(-7.33,1.45) | -1.43(-4.70,1.83) | -2.20(-3.35,-1.05)a | — | — | — |
| 安慰剂针刺 | 0.56(-4.45,5.57) | -3.61(-8.74,1.48) | -2.09(-6.03,1.81) | -2.87(-5.35,-0.40)a | -0.66(-3.30,1.95) | — | — |
| 空白对照 | -3.46(-9.58,2.72) | -7.63(-13.88,-1.31)a | -6.11(-11.44,-0.77)a | -6.88(-11.24,-2.50)a | -4.68(-9.20,-0.14)a | -4.01(-9.04,1.04) | — |
表3 基于PSQI评分改善情况的网状Meta分析结果〔MD(95%CI)〕
Table 3 Results of network meta-analysis based on improvement in PSQI score
| 干预措施 | 艾灸 | 电针 | 耳穴压豆 | 刮痧 | 揿针 | 推拿 | |
|---|---|---|---|---|---|---|---|
| 艾灸 | — | — | — | — | — | — | |
| 电针 | -1.81(-5.57,1.93) | — | — | — | — | — | |
| 耳穴压豆 | -1.97(-6.10,2.17) | -0.17(-4.05,3.76) | — | — | — | — | |
| 刮痧 | -1.58(-5.11,2.00) | 0.23(-3.10,3.62) | 0.40(-3.38,4.18) | — | — | — | |
| 揿针 | -2.13(-6.25,1.97) | -0.32(-4.19,3.55) | -0.14(-4.43,4.10) | -0.55(-4.32,3.16) | — | — | |
| 推拿 | -3.79(-7.92,0.33) | -1.97(-5.95,2.00) | -1.80(-6.18,2.53) | -2.21(-5.97,1.53) | -1.66(-5.96,2.66) | — | |
| 温针 | -5.85(-11.07,-0.62)a | -4.04(-9.04,0.97) | -3.87(-9.24,1.47) | -4.27(-9.28,0.70) | -3.72(-9.04,1.61) | -2.06(-7.51,3.38) | |
| 蜂针 | -1.68(-6.91,3.53) | 0.13(-4.95,5.22) | 0.30(-5.07,5.65) | -0.10(-5.03,4.77) | 0.45(-4.92,5.80) | 2.10(-3.23,7.45) | |
| 穴位埋线 | -3.20(-7.42,1.02) | -1.39(-5.29,2.56) | -1.22(-5.58,3.12) | -1.62(-5.56,2.28) | -1.07(-5.37,3.26) | 0.59(-3.87,5.07) | |
| 针刺 | -2.42(-5.33,0.49) | -0.61(-3.07,1.86) | -0.44(-3.54,2.65) | -0.85(-3.33,1.60) | -0.30(-3.35,2.77) | 1.36(-1.89,4.61) | |
| 镇静安眠西药 | -4.62(-7.44,-1.81)a | -2.82(-5.36,-0.25)a | -2.65(-5.75,0.44) | -3.05(-5.24,-0.89)a | -2.50(-5.54,0.57) | -0.84(-3.87,2.19) | |
| 安慰剂针刺 | -5.28(-9.05,-1.53)a | -3.48(-5.66,-1.31)a | -3.31(-7.24,0.60) | -3.71(-7.15,-0.33)a | -3.16(-7.06,0.74) | -1.50(-5.53,2.49) | |
| 空白对照 | -9.30(-14.55,-4.06)a | -7.50(-12.50,-2.45)a | -7.33(-12.69,-1.97)a | -7.72(-12.76,-2.70)a | -7.17(-12.49,-1.84)a | -5.51(-10.98,-0.07)a | |
| 干预措施 | 温针 | 蜂针 | 穴位埋线 | 针刺 | 镇静安眠西药 | 安慰剂针刺 | 空白对照 |
| 艾灸 | — | — | — | — | — | — | — |
| 电针 | — | — | — | — | — | — | — |
| 耳穴压豆 | — | — | — | — | — | — | — |
| 刮痧 | — | — | — | — | — | — | — |
| 揿针 | — | — | — | — | — | — | — |
| 推拿 | — | — | — | — | — | — | — |
| 温针 | — | — | — | — | — | — | — |
| 蜂针 | 4.17(-2.11,10.47) | — | — | — | — | — | — |
| 穴位埋线 | 2.65 (-2.68,7.96) | -1.51(-6.98,3.96) | — | — | — | — | — |
| 针刺 | 3.43(-0.93,7.77) | -0.75(-5.28,3.82) | 0.77(-2.27,3.83) | — | — | — | — |
| 镇静安眠西药 | 1.22(-3.29,5.74) | -2.95(-7.33,1.45) | -1.43(-4.70,1.83) | -2.20(-3.35,-1.05)a | — | — | — |
| 安慰剂针刺 | 0.56(-4.45,5.57) | -3.61(-8.74,1.48) | -2.09(-6.03,1.81) | -2.87(-5.35,-0.40)a | -0.66(-3.30,1.95) | — | — |
| 空白对照 | -3.46(-9.58,2.72) | -7.63(-13.88,-1.31)a | -6.11(-11.44,-0.77)a | -6.88(-11.24,-2.50)a | -4.68(-9.20,-0.14)a | -4.01(-9.04,1.04) | — |
| 干预措施 | 电针 | 刮痧 | 温针 | 针刺 | 镇静安眠西药 | 安慰剂针刺 | 空白对照 |
|---|---|---|---|---|---|---|---|
| 电针 | — | — | — | — | — | — | — |
| 刮痧 | 3.65(-26.57,34.01) | — | — | — | — | — | — |
| 温针 | -2.45(-21.71,16.41) | -6.10(-33.97,21.19) | — | — | — | — | — |
| 针刺 | 0.22(-18.63,19.23) | -3.41(-26.92,20.05) | 2.68(-11.55,17.51) | — | — | — | — |
| 镇静安眠西药 | -3.12(-25.47,19.33) | -6.78(-27.15,13.53) | -0.68(-19.07,18.36) | -3.37(-15.13,8.42) | — | — | — |
| 安慰剂针刺 | -16.66(-36.88,3.58) | -20.30(-56.79,15.89) | -14.20(-41.87,13.66) | -16.86(-44.80,10.73) | -13.51(-43.82,16.54) | — | — |
| 空白对照 | -5.90(-33.79,22.16) | -9.53(-40.68,21.52) | -3.45(-28.29,22.04) | -6.15(-26.70,14.43) | -2.78(-26.41,20.87) | 10.75(-23.80,45.51) | — |
表4 基于Kupperman评分改善情况的网状Meta分析结果〔MD(95%CI)〕
Table 4 Results of network meta-analysis based on improvement in Kupperman score
| 干预措施 | 电针 | 刮痧 | 温针 | 针刺 | 镇静安眠西药 | 安慰剂针刺 | 空白对照 |
|---|---|---|---|---|---|---|---|
| 电针 | — | — | — | — | — | — | — |
| 刮痧 | 3.65(-26.57,34.01) | — | — | — | — | — | — |
| 温针 | -2.45(-21.71,16.41) | -6.10(-33.97,21.19) | — | — | — | — | — |
| 针刺 | 0.22(-18.63,19.23) | -3.41(-26.92,20.05) | 2.68(-11.55,17.51) | — | — | — | — |
| 镇静安眠西药 | -3.12(-25.47,19.33) | -6.78(-27.15,13.53) | -0.68(-19.07,18.36) | -3.37(-15.13,8.42) | — | — | — |
| 安慰剂针刺 | -16.66(-36.88,3.58) | -20.30(-56.79,15.89) | -14.20(-41.87,13.66) | -16.86(-44.80,10.73) | -13.51(-43.82,16.54) | — | — |
| 空白对照 | -5.90(-33.79,22.16) | -9.53(-40.68,21.52) | -3.45(-28.29,22.04) | -6.15(-26.70,14.43) | -2.78(-26.41,20.87) | 10.75(-23.80,45.51) | — |
| 干预措施 | 刮痧 | 穴位埋线 | 针刺 | 镇静安眠西药 | 安慰剂针刺 |
|---|---|---|---|---|---|
| 刮痧 | — | — | — | — | — |
| 穴位埋线 | 10.97(-38.38,57.83) | — | — | — | — |
| 针刺 | -2.41(-39.90,33.01) | -13.32(-44.75,17.95) | — | — | — |
| 镇静安眠西药 | 5.91(-28.57,39.64) | -5.08(-38.19,29.69) | 8.24(-3.93,21.93) | — | — |
| 安慰剂针刺 | -4.35(-54.44,43.15) | -15.31(-60.50,29.52) | -1.98(-34.45,30.21) | -10.25(-46.12,23.54) | — |
表5 基于E2水平改善情况的网状Meta分析结果〔MD(95%CI)〕
Table 5 Results of network meta-analysis based on improvement in E2 level
| 干预措施 | 刮痧 | 穴位埋线 | 针刺 | 镇静安眠西药 | 安慰剂针刺 |
|---|---|---|---|---|---|
| 刮痧 | — | — | — | — | — |
| 穴位埋线 | 10.97(-38.38,57.83) | — | — | — | — |
| 针刺 | -2.41(-39.90,33.01) | -13.32(-44.75,17.95) | — | — | — |
| 镇静安眠西药 | 5.91(-28.57,39.64) | -5.08(-38.19,29.69) | 8.24(-3.93,21.93) | — | — |
| 安慰剂针刺 | -4.35(-54.44,43.15) | -15.31(-60.50,29.52) | -1.98(-34.45,30.21) | -10.25(-46.12,23.54) | — |
| 作者 | 干预措施 | 不良反应 | 处理措施/缓解情况 |
|---|---|---|---|
| 李佳[ | 艾灸vs镇静安眠西药 | T:无。C:出现嗜睡、头晕 | 自行缓解 |
| 陈秀玲等[ | 电针vs镇静安眠西药 | T:无。C:晨起后出现精神疲倦、乏力、头晕等不适 | 自行缓解 |
| LI等[ | 电针vs安慰剂针刺 | T:1例患者出现出血,1例患者出现疼痛。C:1例患者出现疼痛 | 未予以处理 |
| 师维[ | 电针vs针刺 | T:1例患者出现不良反应。C:2例患者出现不良反应 | 简单处理后恢复 |
| 于心同等[ | 电针vs安慰剂针刺 | 个别患者出现轻微出血、疼痛 | 用消毒棉球进行按压止血,调整针刺深度 |
| 王子岳[ | 刮痧vs镇静安眠西药 | T:2例患者出现皮肤破损。C:1例患者出现恶心,1例患者出现腹泻 | T:用碘伏消毒。C:按揉腹部,给予止泻药 |
| 李清玲[ | 揿针vs针刺 | 个别患者针刺穴位处出现局部疼痛和局部小血肿 | 未提及 |
| 崔威等[ | 无痛蜂针疗法vs镇静安眠西药 | T:2例患者出现发热。C:无 | 1例患者自愈,1例患者通过自行服用解热镇痛药退热 |
| 秦媛媛[ | 针刺vs镇静安眠西药 | T:3例患者出现局部轻微皮下血肿。C:2例患者出现日间嗜睡,3例患者出现疲乏,2例患者出现头晕 | T:皮下血肿自行缓解。C:对于日间嗜睡患者,减少药量后,患者症状缓解;对于疲乏/头晕患者,未予以处理 |
| FU等[ | 针刺vs安慰剂针刺 | T:无。C:4例患者出现失眠症状加重 | 未提及 |
表6 非药物干预在改善围绝经期失眠症状中的安全性分析
Table 6 Safety analysis of non-pharmacological interventions in improving perimenopausal insomnia symptoms
| 作者 | 干预措施 | 不良反应 | 处理措施/缓解情况 |
|---|---|---|---|
| 李佳[ | 艾灸vs镇静安眠西药 | T:无。C:出现嗜睡、头晕 | 自行缓解 |
| 陈秀玲等[ | 电针vs镇静安眠西药 | T:无。C:晨起后出现精神疲倦、乏力、头晕等不适 | 自行缓解 |
| LI等[ | 电针vs安慰剂针刺 | T:1例患者出现出血,1例患者出现疼痛。C:1例患者出现疼痛 | 未予以处理 |
| 师维[ | 电针vs针刺 | T:1例患者出现不良反应。C:2例患者出现不良反应 | 简单处理后恢复 |
| 于心同等[ | 电针vs安慰剂针刺 | 个别患者出现轻微出血、疼痛 | 用消毒棉球进行按压止血,调整针刺深度 |
| 王子岳[ | 刮痧vs镇静安眠西药 | T:2例患者出现皮肤破损。C:1例患者出现恶心,1例患者出现腹泻 | T:用碘伏消毒。C:按揉腹部,给予止泻药 |
| 李清玲[ | 揿针vs针刺 | 个别患者针刺穴位处出现局部疼痛和局部小血肿 | 未提及 |
| 崔威等[ | 无痛蜂针疗法vs镇静安眠西药 | T:2例患者出现发热。C:无 | 1例患者自愈,1例患者通过自行服用解热镇痛药退热 |
| 秦媛媛[ | 针刺vs镇静安眠西药 | T:3例患者出现局部轻微皮下血肿。C:2例患者出现日间嗜睡,3例患者出现疲乏,2例患者出现头晕 | T:皮下血肿自行缓解。C:对于日间嗜睡患者,减少药量后,患者症状缓解;对于疲乏/头晕患者,未予以处理 |
| FU等[ | 针刺vs安慰剂针刺 | T:无。C:4例患者出现失眠症状加重 | 未提及 |
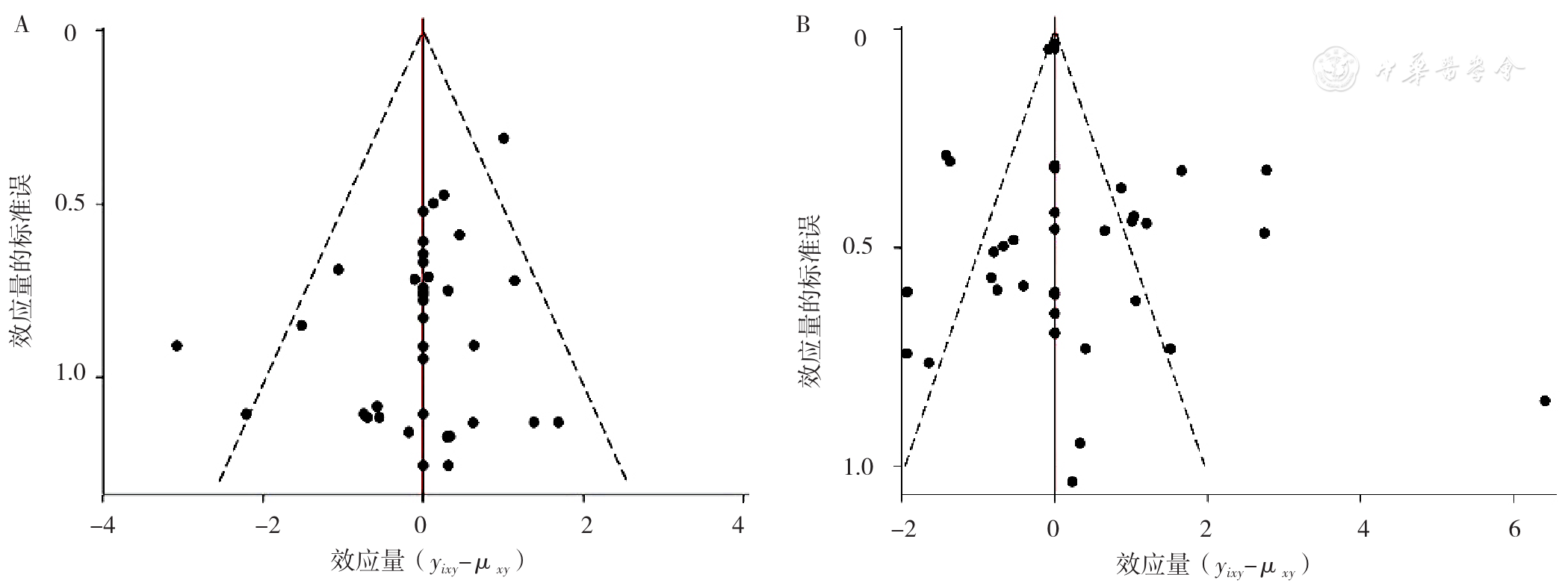
图5 基于围绝经期失眠症状改善总有效率和PSQI评分改善情况的漏斗图注:A表示基于围绝经期失眠症状改善总有效率的漏斗图,B表示基于PSQI评分改善情况的漏斗图。
Figure 5 Funnel plot based on total response rate in improving perimenopausal insomnia symptoms and PSQI score
| [1] |
谢幸,孔北华,段涛. 妇产科学[M]. 北京:人民卫生出版社,2018:353-356.
|
| [2] |
彭晓明,丁晓华. 围绝经期失眠症的治疗新进展[J]. 西部中医药,2018,31(2):141-145.
|
| [3] |
|
| [4] |
蒋东丽,江钢辉,蒋东君. 针灸治疗围绝经期失眠疗效的Meta分析及试验序贯分析[J]. 护理研究,2021,35(14):2481-2488.
|
| [5] |
罗彩凤,魏清琳,王正婷,等. 中医综合疗法治疗围绝经期失眠症[J]. 中医药临床杂志,2020,32(10):1986-1990.
|
| [6] |
|
| [7] |
蒋玲洁,岳伟岗,王盛均,等. 非药物干预比较改善ICU患者睡眠质量效果的网状Meta分析[J]. 中国循证医学杂志,2020,20(4):403-411.
|
| [8] |
马宝璋. 中医妇科学[M]. 北京:中国中医药出版社,2004:119-120.
|
| [9] |
中华医学会精神科分会. 中国精神疾病分类方案与诊断标准(CCMD-3)[M]. 3版. 济南:山东科学技术出版社,2001:118-119.
|
| [10] |
中华人民共和国卫生部. 中药新药临床研究指导原则[M]. 北京:中华人民共和国卫生部,1993:186.
|
| [11] |
The Cochrane Collbration. Cochrane handbook for systematic reviews of interventions,version 5.1.0[EB/OL]. [2022-05-07].
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
刘航,胡秀武,邓陈英. 长蛇灸治疗肝郁气滞型更年期失眠临床观察[J]. 中国中医药现代远程教育,2022,20(6):113-115.
|
| [16] |
李佳. 雷火灸治疗围绝经期妇女失眠症的临床研究[D]. 广州:广州中医药大学,2012.
|
| [17] |
陈秀玲,徐凯,秦小红. 电针治疗女性围绝经期失眠症疗效观察[J]. 上海针灸杂志,2011,30(6):366-367.
|
| [18] |
柯庆宗. 郁三针配合定神针治疗更年期睡眠障碍的临床研究[D]. 广州:广州中医药大学,2015.
|
| [19] |
王婉娣. 阴阳调衡透刺针法电针与安慰电针治疗围绝经期失眠的临床观察[D]. 上海:上海中医药大学,2015.
|
| [20] |
|
| [21] |
师维. 电针治疗围绝经期睡眠障碍的临床随机对照研究[D]. 成都:成都中医药大学,2017.
|
| [22] |
于心同,牟艳艳,孙栩秋,等. 电针对肝肾阴虚型围绝经期失眠患者睡眠和生活质量的影响[J]. 中医药信息,2022,39(3):69-73.
|
| [23] |
贾美君,黄丽华,艾叶盛. 耳穴压珠治疗更年期失眠的临床疗效[J]. 世界睡眠医学杂志,2018,5(4):458-461.
|
| [24] |
杨松柏,梅志刚,蔡三金,等. 三种不同针刺方法对女性更年期失眠症的疗效比较:随机对照研究[EB/OL]. (2013-09-09)[2022-05-07].
|
| [25] |
陈丽兰,陈阿兰,廖惠玲,等. 全息刮痧疗法干预女性围绝经期失眠的临床研究[J]. 中医外治杂志,2021,30(1):6-7.
|
| [26] |
彭德忠,王红艳,申渝泉,等. 基于子午流注理论的刮痧疗法治疗围绝经期女性失眠的临床研究[J]. 时珍国医国药,2014,25(9):2186-2187.
|
| [27] |
王子岳. 子午流注纳支刮痧法治疗痰湿体质围绝经期失眠的临床观察[D]. 成都:成都中医药大学,2015.
|
| [28] |
杨娟. 刮痧治疗更年期综合征失眠症状的临床应用[J]. 健康大视野,2020,27(18):69.
|
| [29] |
施兰来,杨毅华,黄荷贤,等. 火龙罐疗法对心肾不交型围绝经期患者睡眠障碍的影响[J]. 护理学杂志,2021,36(12):56-59.
|
| [30] |
陈阳,赵锐,章小娟,等. 揿针治疗围绝经期妇女心肾不交型失眠的疗效观察[J]. 健康女性,2021,13(47):12.
|
| [31] |
李清玲. 新型揿针治疗围绝经期失眠的临床研究[J]. 四川中医,2017,35(6):202-204.
|
| [32] |
高亮. 背腧穴擦法治疗更年期失眠临床观察[J]. 浙江中西医结合杂志,2016,26(5):458-460.
|
| [33] |
王艺晴. 点按推拿四步疗法对缓解围绝经期心肾不交型失眠的临床观察研究[D]. 贵阳:贵阳中医学院,2018.
|
| [34] |
王甜. 温针灸治疗围绝经期心肾不交型失眠的临床研究[D]. 武汉:湖北中医药大学,2018.
|
| [35] |
崔威,王淑平,成永明,等. 岭南无痛蜂针疗法治疗更年期睡眠障碍的临床研究[J]. 实用医学杂志,2017,33(10):1700-1703.
|
| [36] |
韩慧,刘洋. 针刺跷脉与穴位埋线治疗围绝经期失眠的疗效对比研究[J]. 针灸临床杂志,2020,36(2):14-18.
|
| [37] |
李霞,何志勇. 星状神经节为主埋线治疗围绝经期失眠症的疗效[J]. 东方药膳,2019,25(23):101.
|
| [38] |
刘志霞,畅红梅,龚旺梅. 穴位埋线法治疗围绝经期失眠症40例疗效观察[J]. 新中医,2014,46(10):177-179.
|
| [39] |
俞鑫佳,王松根. 穴位埋线治疗女性更年期失眠疗效观察[J]. 上海针灸杂志,2015,34(4):323-325.
|
| [40] |
王苑,黎丽娴,冯欣欣. 音乐疗法对31例围绝经期女性睡眠障碍的影响[J]. 按摩与康复医学,2020,11(2):50-51.
|
| [41] |
|
| [42] |
郭琴. 调任通督针刺法治疗对围绝经期失眠患者睡眠质量、神经内分泌水平的影响[J]. 中国医学创新,2021,18(27):82-85.
|
| [43] |
黄文雄,余秀梅,曾小红. 腹针联合头针治疗围绝经期失眠疗效及其机制探讨[J]. 天津中医药,2021,38(10):1294-1298.
|
| [44] |
李泓,袁斓,周仕轶,等. 不同针刺方法治疗围绝经期肝郁化火失眠症的疗效观察[J]. 成都中医药大学学报,2016,39(3):34-37.
|
| [45] |
李欧静,王凡. 针刺五脏俞加膈俞配神门穴治疗女性更年期失眠临床研究[J]. 中国针灸,2018,38(5):469-472.
|
| [46] |
李亚男. 针刺下三皇治疗更年期失眠120例疗效观察[J]. 中国实用医药,2014,9(19):244-246.
|
| [47] |
林文馨,尹平,徐世芬. 调任通督针刺法对围绝经期失眠的临床疗效评价[J]. 上海针灸杂志,2017,36(8):900-904.
|
| [48] |
秦媛媛. 基于从肝论治失眠理论针刺治疗围绝经期失眠肝亢肾虚证的临床研究[D]. 成都:成都中医药大学,2018.
|
| [49] |
王延玉. 针灸治疗更年期失眠28例[J]. 中国保健营养,2017,27(33):386.
|
| [50] |
向华平. 针刺五脏俞加膈俞配神门穴治疗女性更年期失眠临床分析[J]. 养生保健指南,2020,19(6):246.
|
| [51] |
杨继若,许会英,白晶梅,等. 头针体针并用治疗围绝经期失眠症81例[J]. 西部中医药,2017,30(2):4-6.
|
| [52] |
杨玉婷. 房式十三针治疗围绝经期失眠症的临床疗效[J]. 深圳中西医结合杂志,2021,31(7):71-72.
|
| [53] |
张婉容,郭华,谭少华,等. 针刺与艾灸引气归元穴组治疗围绝经期失眠症的随机对照研究[J]. 针刺研究,2019,44(5):358-362.
|
| [54] |
张巍,皮燕,陈婷,等. 从肝论治针刺治疗围绝经期失眠的临床观察[J]. 四川中医,2017,35(9):152-155.
|
| [55] |
|
| [56] |
纪峰. 交通心肾针刺法治疗更年期失眠症临床观察[J]. 上海针灸杂志,2008,27(12):21-22.
|
| [57] |
卢晨,杨秀娟,胡洁. 疏肝理脾与调理督脉取穴针刺治疗围绝经期失眠症疗效对比[J]. 中国针灸,2014,34(8):759-762.
|
| [58] |
孙枚,张继芳. 交通心肾针法治疗更年期失眠症的效果评价[J]. 中国农村卫生,2016,4(6):89-90.
|
| [59] |
高凤霞,张晓颖,陈飞. 北京市平谷区医院医护人员围绝经期相关情况及认知调查[J]. 生殖医学杂志,2016,25(5):458-462.
|
| [60] |
盛祝梅,黄坚,马林,等. 杭州地区围绝经期综合征患病状况分析调查[J]. 中国现代医生,2018,56(36):121-124.
|
| [61] |
朱晓璐,李萍,孙东梅,等. 上海徐汇区中年妇女围绝经期症状调查[J]. 中国妇幼健康研究,2016,27(1):38-41.
|
| [62] |
|
| [63] |
黄旭博,周艳艳,周俊英,等. 围绝经期女性失眠的治疗研究进展[J]. 中国民间疗法,2022,30(2):119-123.
|
| [64] |
董小庆,黄琴峰,谢晨,等. 艾灸治疗失眠的临床应用规律分析[J]. 世界科学技术-中医药现代化,2019,21(8):1615-1621.
|
| [65] |
文幸,米建平. 艾灸背俞穴联合电针治疗围绝经期睡眠障碍临床观察[J]. 新中医,2013,45(5):129-131.
|
| [66] |
王洪彬,李晓泓,莫捷,等. 灸法与治未病[J]. 中华中医药杂志,2012,27(9):2264-2266.
|
| [67] |
陈晓琴,李瑛,秦尔奇,等. 针刺配合重灸涌泉穴治疗围绝经期失眠40例临床观察[J]. 国医论坛,2019,34(6):37-39.
|
| [68] |
张明明,高希言,李潇,等. 针刺背俞穴结合透灸法治疗安眠药物依赖性失眠23例[J]. 中国针灸,2019,39(3):251-252.
|
| [69] |
|
| [70] |
孟方,段培蓓,胡倩,等. 刮痧疗法用于围绝经期失眠患者的效果观察[J]. 护理学杂志,2016,31(12):49-52.
|
| [71] |
郑娟,朱燕,李瑾. 调肾安神刮痧对围绝经期失眠病人负性情绪及血清E2、FSH、5-HT的影响[J]. 全科护理,2021,19(30):4256-4259.
|
| [72] |
|
| [73] |
闫雪丽,于远东,杨丹丹. 针刺结合香附汤加减治疗围绝经期失眠肝郁气滞证的临床研究[J]. 中国中药杂志,2020,45(6):1460-1464.
|
| [74] |
杨文佳. 从雌激素及其受体研究针刺治疗围绝经期失眠的临床疗效及神经内分泌机制[D]. 上海:上海中医药大学,2017.
|
| [1] | 张红石, 曲子涵, 孙雪峰, 王宇峰, 丛德毓, 张野. 基于蛋白质组学技术分析腹部推拿对失眠大鼠下丘脑的影响研究[J]. 中国全科医学, 2025, 28(27): 3399-3409. |
| [2] | 全家霖, 朱琳, 苏煜, 陈泽恺, 陈梓淇, 张卓凡. 运动方式对超重或肥胖儿童青少年执行功能改善效果的网状Meta分析[J]. 中国全科医学, 2025, 28(27): 3422-3431. |
| [3] | 聂丹宁, 史曙生, 陶昱如. 本体感觉神经肌肉促进技术联合螺旋稳定肌肉链训练治疗青少年特发性脊柱侧弯的临床效果研究[J]. 中国全科医学, 2025, 28(24): 3032-3042. |
| [4] | 李浩, 李江涛, 刘丹, 王建军. 贝利尤单抗和阿尼鲁单抗及泰它西普治疗系统性红斑狼疮疗效和安全性的网状Meta分析[J]. 中国全科医学, 2025, 28(23): 2924-2933. |
| [5] | 文敏, 周永玲, 刘静静, 蒋苛晴, 刘娟, 朱晓丹. 基于移动医疗APP的认知补偿训练对稳定期精神分裂症患者的干预效果与机制研究[J]. 中国全科医学, 2025, 28(22): 2819-2825. |
| [6] | 杨涵单, 乔雯, 何姝, 陈易, 童云梅. 接纳承诺疗法联合舍曲林对抑郁症青少年抑郁情绪、自杀意念及睡眠质量的影响研究[J]. 中国全科医学, 2025, 28(22): 2813-2818. |
| [7] | 王颖, 颜轶隽, 刘蕾, 胡毓敏, 张扬, 刘凯, 姜博仁. 抗阻力运动联合营养干预对老年2型糖尿病合并肌少症患者血糖稳定性影响的临床研究[J]. 中国全科医学, 2025, 28(21): 2604-2610. |
| [8] | 马盼盼, 王思静, 游娜, 丁大法, 鲁一兵. Danuglipron与Orforglipron治疗2型糖尿病疗效及安全性的Meta分析[J]. 中国全科医学, 2025, 28(21): 2679-2685. |
| [9] | 何芸, 范焕芳, 马盼, 许绍青, 杨柳, 金明哲, 张明蕊, 陈佳琪. 不同针灸治疗方式干预乳腺癌术后上肢淋巴水肿效果的网状Meta分析[J]. 中国全科医学, 2025, 28(14): 1788-1794. |
| [10] | 朱胜杰, 刁华琼, 杭晓屹, 孙文军. 不同中成药注射液治疗后循环缺血性眩晕效果的网状Meta分析[J]. 中国全科医学, 2025, 28(14): 1795-1808. |
| [11] | 郭鑫, 周明娟, 范斐婷, 肖晶旻, 池逸和, 吴蕾, 林琳, 陈远彬. 天灸散穴位贴敷治疗支气管哮喘前期的随机对照研究[J]. 中国全科医学, 2025, 28(11): 1367-1375. |
| [12] | 迟洵, 刘思思, 陈巧, 胡玥, 王伟仙. 不同营养筛查工具对肝硬化患者营养筛查适用性的网状Meta分析[J]. 中国全科医学, 2025, 28(11): 1395-1402. |
| [13] | 李晓泽, 孙国强, 沈蔷, 宋妍, 王虎峰. 社区中老年慢性病患者个体化健康教育干预效果:一项整群随机对照试验[J]. 中国全科医学, 2025, 28(11): 1320-1328. |
| [14] | 中国医师协会睡眠医学专业委员会, 中国医师协会神经内科医师分会睡眠学组. 中国成人失眠共病阻塞性睡眠呼吸暂停诊治指南(2024版)[J]. 中国全科医学, 2025, 28(11): 1289-1303. |
| [15] | 余悦敏, 莫非非, 李乐思, 潘集阳. 中国青少年失眠的评估工具和影响因素:一项范围综述[J]. 中国全科医学, 2025, 28(10): 1213-1219. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





