中国全科医学 ›› 2023, Vol. 26 ›› Issue (17): 2147-2154.DOI: 10.12114/j.issn.1007-9572.2022.0568
所属专题: 肿瘤最新文章合辑
靳通通1, 吴王剑1, 付豪1, 何万滨1, 周逢海1,2,*( )
)
收稿日期:2022-06-15
修回日期:2022-10-12
出版日期:2023-06-15
发布日期:2022-10-31
通讯作者:
周逢海
基金资助:
JIN Tongtong1, WU Wangjian1, FU Hao1, HE Wanbin1, ZHOU Fenghai1,2,*( )
)
Received:2022-06-15
Revised:2022-10-12
Published:2023-06-15
Online:2022-10-31
Contact:
ZHOU Fenghai
摘要: 背景 前列腺癌是危害我国老年男性生命健康常见的恶性肿瘤之一,前列腺癌根治术是局限性前列腺癌治疗最主要的手段。然而,部分患者存在术后病理标本切缘阳性,而切缘阳性是术后生化复发的高风险指标,是预后不良的高风险因素。目前有关中国人群前列腺癌根治术后切缘阳性的危险因素尚无统一意见。 目的 探讨中国人群前列腺癌根治术后切缘阳性的危险因素,为防控工作提供参考。 方法 计算机检索PubMed、Embase、Cochrane Library、Web of Science、中国知网、万方数据知识服务平台、中国生物医学文献数据库和维普网,搜集有关中国人群前列腺癌根治术后切缘阳性危险因素的相关文献,检索时限均从建库至2022-03-01,使用纽卡斯尔-渥太华量表(NOS)评价队列研究质量。采用Stata 16.0统计学软件对纳入研究的数据进行Meta分析。 结果 最终纳入21篇病例对照研究,包括6 782例患者,其中切缘阳性患者2 028例。Meta分析结果显示,术前高前列腺特异抗原(PSA)〔OR=1.77,95%CI(1.18,2.65)〕、穿刺神经周围侵犯〔OR=5.83,95%CI(2.05,16.59)〕、术前高级别临床T分期〔OR=2.17,95%CI(1.06,4.42)〕、术后高级别病理T分期〔OR=4.30,95%CI(2.43,7.63)〕、高穿刺阳性针数百分比〔OR=1.83,95%CI(1.35,2.47)〕、高穿刺格里森(Gleason)评分〔OR=2.14,95%CI(1.67,2.74)〕、术后高Gleason评分〔OR= 2.33,95%CI(1.80,3.01)〕是我国人群前列腺癌根治术后切缘阳性的危险因素(P<0.05)。不同的手术方式的亚组分析显示,术前高级别临床T分期〔OR=4.57,95%CI(2.57,8.12)〕、术后高级别病理T分期〔OR=4.80,95%CI(2.20,10.48)〕,术后高Gleason评分〔OR=2.46,95%CI(1.57,3.86)〕是行腹腔镜下根治性前列腺切除术的前列腺癌患者切缘阳性的危险因素(P<0.05);术前高PSA〔OR=2.17,95%CI(1.60,2.94)〕是行机器人辅助腹腔镜根治性前列腺切除术的前列腺癌患者切缘阳性的危险因素(P<0.05)。敏感性分析结果显示,危险因素的一致性均较好,结果具有稳定性;术前PSA、术后病理T分期和术后Gleason评分的漏斗图分布不对称,存在发表偏倚;术前临床T分期漏斗图分布对称,不存在发表偏倚。 结论 PSA、穿刺神经周围侵犯、术前高级别临床T分期、术后高级别病理T分期、高穿刺阳性针数百分比、高穿刺Gleason评分、术后高Gleason评分是我国人群前列腺癌根治术后切缘阳性的危险因素,在临床工作中应尽早识别,并采取干预措施来预防肿瘤复发和进展。
| 步骤 | 检索词 |
|---|---|
| #1 | ( "Prostatectomy" [Title/Abstract] OR "Prostatectomies" [Title/Abstract] OR "suprapubic prostatectomies" [Title/Abstract] OR "suprapubic prostatectomy " [Title/Abstract] OR "retropubic prostatectomies" [Title/Abstract] OR "retropubic prostatectomy" [Title/Abstract] OR "radical prostatectomy" [Title/Abstract] OR(( "radical" [All Fields] OR "radical's" [All Fields] OR "radicals" [All Fields]) AND( "resect" [All Fields] OR "resectability" [All Fields] OR "resectable" [All Fields] OR "resectates" [All Fields] OR "resected" [All Fields] OR "resecting" [All Fields] OR "Resection" [All Fields] OR "resectional" [All Fields] OR "resectioned" [All Fields] OR "resectioning" [All Fields] OR "resections" [All Fields] OR "resective" [All Fields] OR "resects" [All Fields]) AND " prostate cancer" [Title/Abstract])) |
| #2 | ( "positive margin" [Title/Abstract] OR "positive excision margins" [Title/Abstract] OR "margins of excision" [Title/Abstract] OR "excision margin" [Title/Abstract] OR "excision margins" [Title/Abstract] OR "resection margin" [Title/Abstract] OR "resection margins" [Title/Abstract] OR "surgical margins" [Title/Abstract] OR "surgical margin" [Title/Abstract] OR "positive surgical margins" [Title/Abstract] OR "positive surgical margin" [Title/Abstract] OR "negative surgical margins" [Title/Abstract] OR "negative surgical margin" [Title/Abstract] OR "tumor free margins" [Title/Abstract] OR "tumor free margins" [Title/Abstract] OR "tumor free margin" [Title/Abstract]) |
| #3 | ( "Risk factors" [Title/Abstract] OR "social risk factors" [Title/Abstract] OR "social risk factor" [Title/Abstract] OR "health correlates" [Title/Abstract] OR "population at risk" [Title/Abstract] OR "populations at risk" [Title/Abstract] OR "risk scores" [Title/Abstract] OR "risk score" [Title/Abstract] OR "risk factor scores" [Title/Abstract] OR "risk factor score" [Title/Abstract] OR "dangerous factor" [Title/Abstract] OR "hazardous factors" [Title/Abstract] OR "risky factors" [Title/Abstract] OR "risks factors" [Title/Abstract] OR "Risk-factors" [Title/Abstract] OR "danger factors" [Title/Abstract] OR "danger factor" [Title/Abstract] OR "hazard factors" [Title/Abstract] OR "Factor" [Title/Abstract] OR "Factors" [Title/Abstract] OR " elements" [Title/Abstract] OR "element" [Title/Abstract]) |
| #4 | #1 AND #2 AND #3 |
表1 文献检索策略
Table 1 Strategy for searching studies
| 步骤 | 检索词 |
|---|---|
| #1 | ( "Prostatectomy" [Title/Abstract] OR "Prostatectomies" [Title/Abstract] OR "suprapubic prostatectomies" [Title/Abstract] OR "suprapubic prostatectomy " [Title/Abstract] OR "retropubic prostatectomies" [Title/Abstract] OR "retropubic prostatectomy" [Title/Abstract] OR "radical prostatectomy" [Title/Abstract] OR(( "radical" [All Fields] OR "radical's" [All Fields] OR "radicals" [All Fields]) AND( "resect" [All Fields] OR "resectability" [All Fields] OR "resectable" [All Fields] OR "resectates" [All Fields] OR "resected" [All Fields] OR "resecting" [All Fields] OR "Resection" [All Fields] OR "resectional" [All Fields] OR "resectioned" [All Fields] OR "resectioning" [All Fields] OR "resections" [All Fields] OR "resective" [All Fields] OR "resects" [All Fields]) AND " prostate cancer" [Title/Abstract])) |
| #2 | ( "positive margin" [Title/Abstract] OR "positive excision margins" [Title/Abstract] OR "margins of excision" [Title/Abstract] OR "excision margin" [Title/Abstract] OR "excision margins" [Title/Abstract] OR "resection margin" [Title/Abstract] OR "resection margins" [Title/Abstract] OR "surgical margins" [Title/Abstract] OR "surgical margin" [Title/Abstract] OR "positive surgical margins" [Title/Abstract] OR "positive surgical margin" [Title/Abstract] OR "negative surgical margins" [Title/Abstract] OR "negative surgical margin" [Title/Abstract] OR "tumor free margins" [Title/Abstract] OR "tumor free margins" [Title/Abstract] OR "tumor free margin" [Title/Abstract]) |
| #3 | ( "Risk factors" [Title/Abstract] OR "social risk factors" [Title/Abstract] OR "social risk factor" [Title/Abstract] OR "health correlates" [Title/Abstract] OR "population at risk" [Title/Abstract] OR "populations at risk" [Title/Abstract] OR "risk scores" [Title/Abstract] OR "risk score" [Title/Abstract] OR "risk factor scores" [Title/Abstract] OR "risk factor score" [Title/Abstract] OR "dangerous factor" [Title/Abstract] OR "hazardous factors" [Title/Abstract] OR "risky factors" [Title/Abstract] OR "risks factors" [Title/Abstract] OR "Risk-factors" [Title/Abstract] OR "danger factors" [Title/Abstract] OR "danger factor" [Title/Abstract] OR "hazard factors" [Title/Abstract] OR "Factor" [Title/Abstract] OR "Factors" [Title/Abstract] OR " elements" [Title/Abstract] OR "element" [Title/Abstract]) |
| #4 | #1 AND #2 AND #3 |
| 第一作者 | 发表年份(年) | 研究地区 | 样本量(例) | 手术方式 | 结局指标 | NOS评分(分) | |
|---|---|---|---|---|---|---|---|
| 病例组 | 对照组 | ||||||
| 张靖博[ | 2021 | 河南 | 64 | 188 | LRP | ①②⑦⑧ | 8 |
| 张平新[ | 2020 | 新疆 | 26 | 73 | LRP | ⑧ | 6 |
| 阎乙夫[ | 2011 | 北京 | 76 | 112 | LRP | ⑦⑧ | 8 |
| 陈星[ | 2021 | 福建 | 36 | 86 | LRP | ①③④⑦⑧ | 7 |
| 张争[ | 2019 | 北京 | 57 | 120 | LRP | ⑧ | 7 |
| 吴丹[ | 2020 | 江苏 | 34 | 82 | LRP | ⑧ | 6 |
| 缪志俊[ | 2021 | 江苏 | 79 | 420 | LRP | ①③⑤ | 7 |
| 王硕[ | 2021 | 北京 | 97 | 83 | — | ⑦⑧ | 8 |
| 侯惠民[ | 2018 | 北京 | 94 | 226 | — | ② | 7 |
| 范效铮[ | 2021 | 陕西 | 158 | 360 | RARP | ①⑤ | 8 |
| 屈武功[ | 2021 | 河南 | 106 | 204 | RARP | ② | 7 |
| 张春雷[ | 2018 | 上海 | 47 | 143 | RARP | ①⑧ | 7 |
| 沈诞[ | 2012 | 上海 | 258 | 1 390 | RARP | ⑤ | 7 |
| 瞿旻[ | 2017 | 上海 | 151 | 249 | RARP | ①⑤ | 8 |
| 韩涛[ | 2013 | 江苏 | 98 | 162 | LRP | ④⑥ | 6 |
| 张铁龙[ | 2015 | 上海 | 61 | 184 | ORP | ①⑦ | 6 |
| 丁攀[ | 2019 | 江西 | 118 | 114 | — | ①②④⑥ | 7 |
| 洪锴[ | 2008 | 北京 | 9 | 24 | LRP | ⑤⑦ | 7 |
| YANG[ | 2017 | 江苏 | 86 | 210 | LRP | ③④⑥ | 7 |
| WANG[ | 2021 | 北京 | 106 | 94 | — | ④⑤ | 8 |
| ZHOU[ | 2021 | 天津 | 267 | 230 | — | ①⑦ | 8 |
表2 纳入研究的基本特征及偏倚风险评价结果
Table 2 Table of basic characteristics and risk of bias in included studies
| 第一作者 | 发表年份(年) | 研究地区 | 样本量(例) | 手术方式 | 结局指标 | NOS评分(分) | |
|---|---|---|---|---|---|---|---|
| 病例组 | 对照组 | ||||||
| 张靖博[ | 2021 | 河南 | 64 | 188 | LRP | ①②⑦⑧ | 8 |
| 张平新[ | 2020 | 新疆 | 26 | 73 | LRP | ⑧ | 6 |
| 阎乙夫[ | 2011 | 北京 | 76 | 112 | LRP | ⑦⑧ | 8 |
| 陈星[ | 2021 | 福建 | 36 | 86 | LRP | ①③④⑦⑧ | 7 |
| 张争[ | 2019 | 北京 | 57 | 120 | LRP | ⑧ | 7 |
| 吴丹[ | 2020 | 江苏 | 34 | 82 | LRP | ⑧ | 6 |
| 缪志俊[ | 2021 | 江苏 | 79 | 420 | LRP | ①③⑤ | 7 |
| 王硕[ | 2021 | 北京 | 97 | 83 | — | ⑦⑧ | 8 |
| 侯惠民[ | 2018 | 北京 | 94 | 226 | — | ② | 7 |
| 范效铮[ | 2021 | 陕西 | 158 | 360 | RARP | ①⑤ | 8 |
| 屈武功[ | 2021 | 河南 | 106 | 204 | RARP | ② | 7 |
| 张春雷[ | 2018 | 上海 | 47 | 143 | RARP | ①⑧ | 7 |
| 沈诞[ | 2012 | 上海 | 258 | 1 390 | RARP | ⑤ | 7 |
| 瞿旻[ | 2017 | 上海 | 151 | 249 | RARP | ①⑤ | 8 |
| 韩涛[ | 2013 | 江苏 | 98 | 162 | LRP | ④⑥ | 6 |
| 张铁龙[ | 2015 | 上海 | 61 | 184 | ORP | ①⑦ | 6 |
| 丁攀[ | 2019 | 江西 | 118 | 114 | — | ①②④⑥ | 7 |
| 洪锴[ | 2008 | 北京 | 9 | 24 | LRP | ⑤⑦ | 7 |
| YANG[ | 2017 | 江苏 | 86 | 210 | LRP | ③④⑥ | 7 |
| WANG[ | 2021 | 北京 | 106 | 94 | — | ④⑤ | 8 |
| ZHOU[ | 2021 | 天津 | 267 | 230 | — | ①⑦ | 8 |
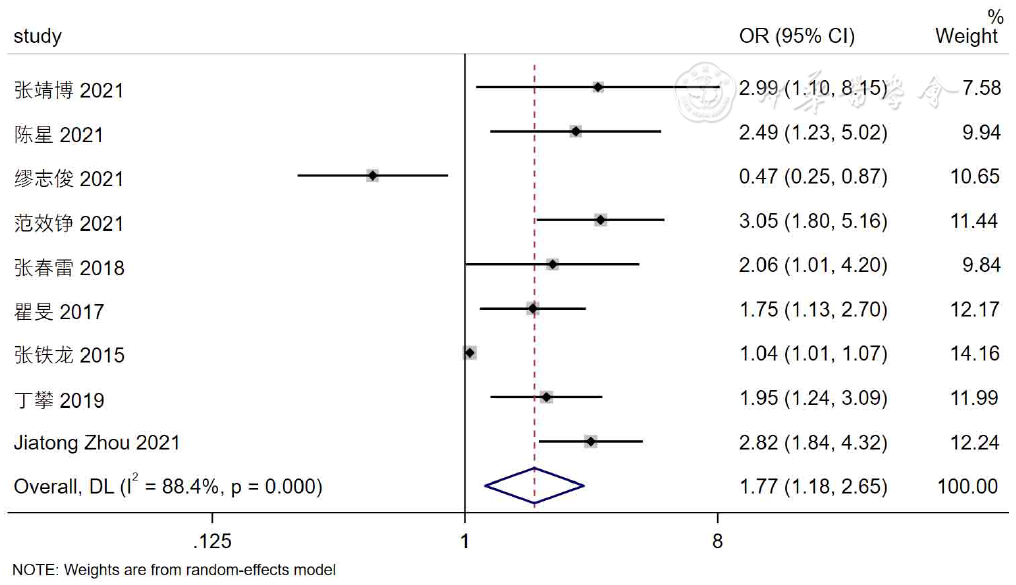
图2 术前PSA与中国人群前列腺癌根治术后PSM相关性的Meta分析
Figure 2 Meta-analysis of the correlation between pre-radical prostatectomy PSA and post-radical prostatectomy PSMs in Chinese men
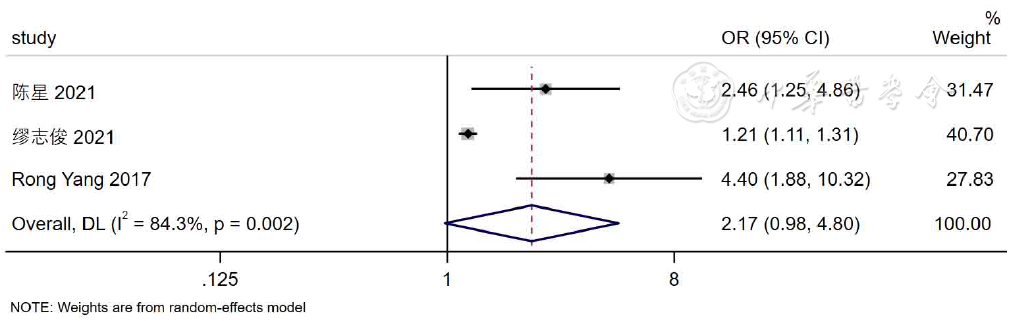
图3 穿刺阳性针数与中国人群前列腺癌根治术后PSM相关性的Meta分析
Figure 3 Meta-analysis of the correlation between number of positive puncture stitches and PSMs after radical prostatectomy in Chinese men
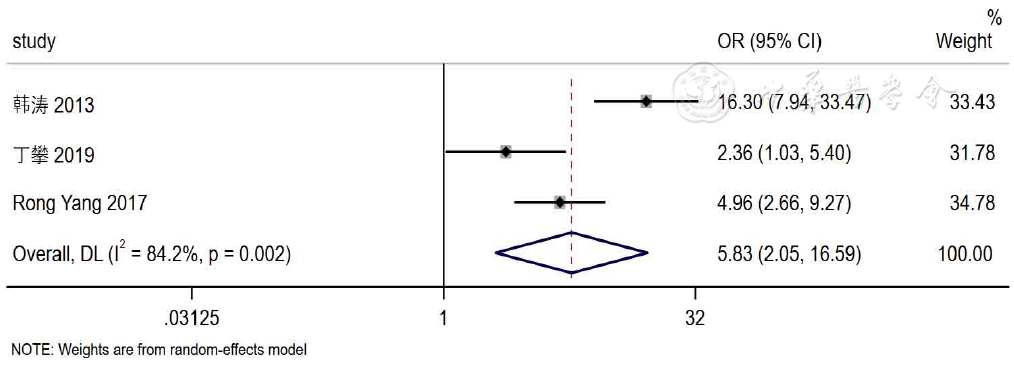
图4 穿刺神经周围侵犯与中国人群前列腺癌根治术后PSM相关性的Meta分析
Figure 4 Meta-analysis of the correlation between perineural invasion at puncture time and post-radical prostatectomy PSMs in Chinese men
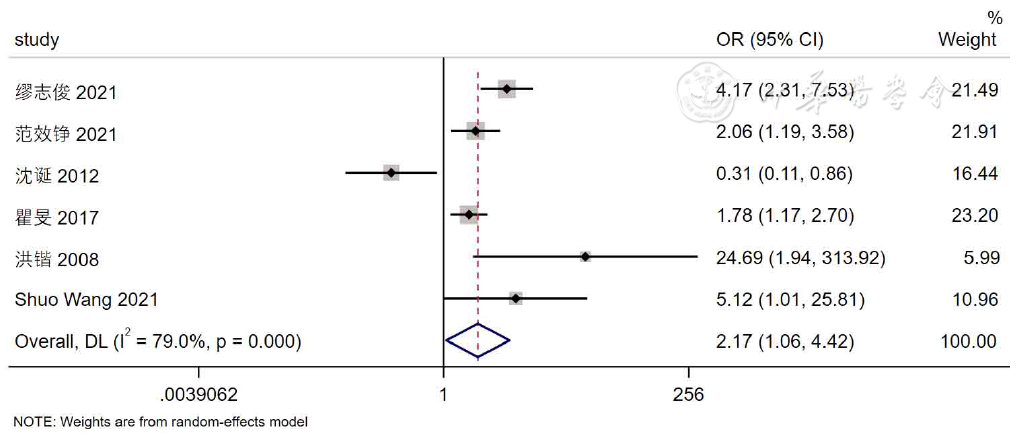
图5 术前临床T分期与中国人群前列腺癌根治术后PSM相关性的Meta分析
Figure 5 Meta-analysis of the correlation between pre-radical prostatectomy clinical T stage and post-radical prostatectomy PSMs in Chinese men
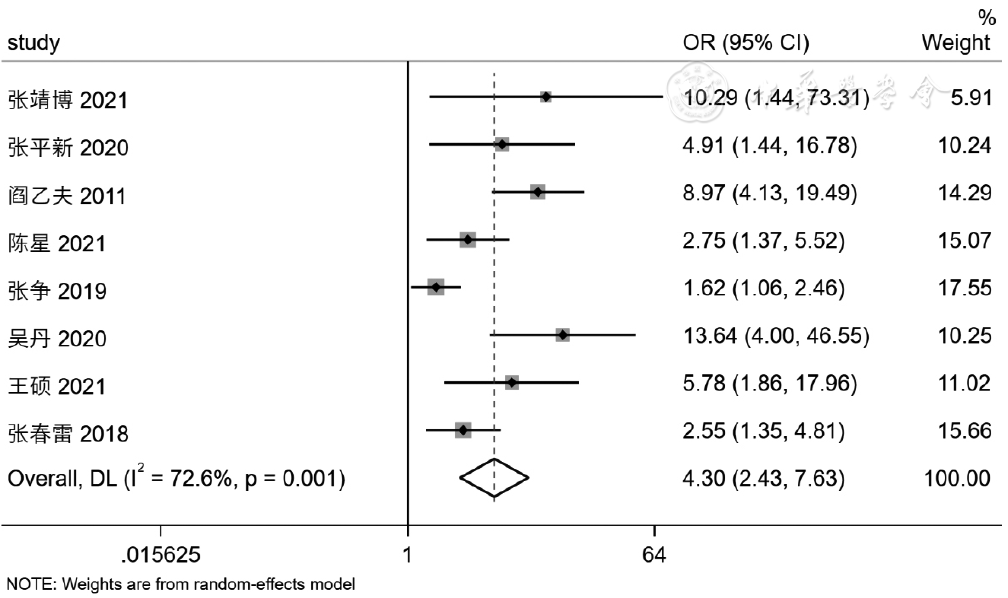
图6 术后病理T分期与中国人群前列腺癌根治术后PSM相关性的Meta分析
Figure 6 Meta-analysis of the correlation between pathological T stage and PSMs after radical prostatectomy in Chinese men
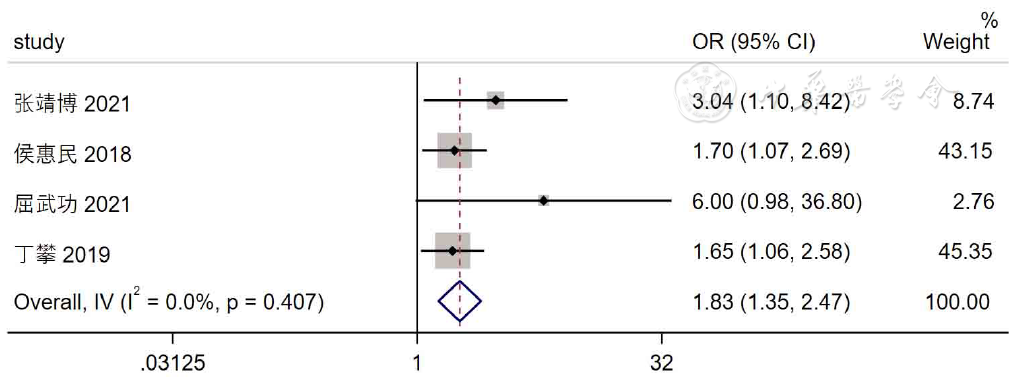
图7 穿刺阳性针数百分比与中国人群前列腺癌根治术后PSM相关性的Meta分析
Figure 7 Meta-analysis of the correlation between positive puncture stitches and PSMs after radical prostatectomy in Chinese men
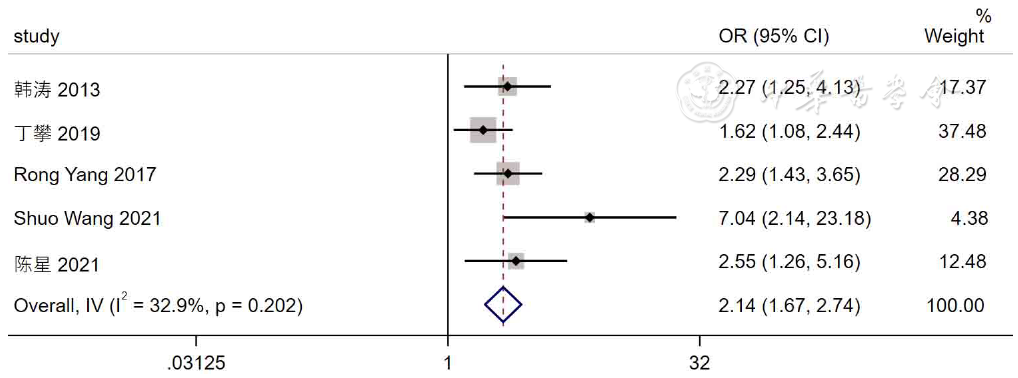
图8 穿刺Gleason评分与中国人群前列腺癌根治术后PSM相关性的Meta分析
Figure 8 Meta-analysis of the correlation between Gleason score at puncture time and PSMs after radical prostatectomy in Chinese men
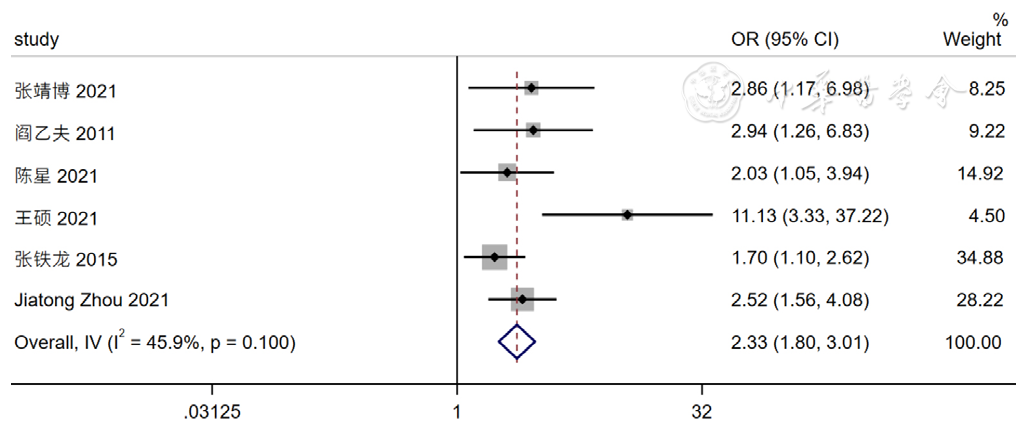
图9 术后Gleason评分与中国人群前列腺癌根治术后PSM相关性的Meta分析
Figure 9 Meta-analysis of the correlation between Gleason score and PSMs after radical prostatectomy in Chinese men
| 危险因素 | 纳入研究数(篇) | 异质性分析结果 | 效应模型 | Meta分析结果 | ||
|---|---|---|---|---|---|---|
| I2值(%) | P值 | OR(95%CI) | P值 | |||
| LRP | ||||||
| 术前PSA | 3[ | 87.7 | <0.001 | 随机效应模型 | 1.47(0.42,5.09) | 0.548 |
| 穿刺阳性针数 | 3[ | 84.3 | 0.002 | 随机效应模型 | 2.17(0.98,4.80) | 0.057 |
| 术前临床T分期 | 2[ | 43.9 | 0.182 | 固定效应模型 | 4.57(2.57,8.12) | <0.001 |
| 术后病理T分期 | 6[ | 79.2 | <0.001 | 随机效应模型 | 4.80(2.20,10.48) | <0.001 |
| 术后Gleason评分 | 3[ | 0 | 0.739 | 固定效应模型 | 2.46(1.57,3.86) | <0.001 |
| RARP | ||||||
| 术前PSA | 3[ | 22.4 | 0.275 | 固定效应模型 | 2.17(1.60,2.94) | <0.001 |
| 术前临床T分期 | 3[ | 81.6 | 0.004 | 随机效应模型 | 1.19(0.52,2.74) | 0.678 |
表3 不同危险因素的亚组分析
Table 3 Subgroup analysis of different risk factors for PSMs after radical prostatectomy
| 危险因素 | 纳入研究数(篇) | 异质性分析结果 | 效应模型 | Meta分析结果 | ||
|---|---|---|---|---|---|---|
| I2值(%) | P值 | OR(95%CI) | P值 | |||
| LRP | ||||||
| 术前PSA | 3[ | 87.7 | <0.001 | 随机效应模型 | 1.47(0.42,5.09) | 0.548 |
| 穿刺阳性针数 | 3[ | 84.3 | 0.002 | 随机效应模型 | 2.17(0.98,4.80) | 0.057 |
| 术前临床T分期 | 2[ | 43.9 | 0.182 | 固定效应模型 | 4.57(2.57,8.12) | <0.001 |
| 术后病理T分期 | 6[ | 79.2 | <0.001 | 随机效应模型 | 4.80(2.20,10.48) | <0.001 |
| 术后Gleason评分 | 3[ | 0 | 0.739 | 固定效应模型 | 2.46(1.57,3.86) | <0.001 |
| RARP | ||||||
| 术前PSA | 3[ | 22.4 | 0.275 | 固定效应模型 | 2.17(1.60,2.94) | <0.001 |
| 术前临床T分期 | 3[ | 81.6 | 0.004 | 随机效应模型 | 1.19(0.52,2.74) | 0.678 |
| 危险因素 | 随机效应模型 | 固定效应模型 | ||
|---|---|---|---|---|
| OR(95%CI) | P值 | OR(95%CI) | P值 | |
| 术前PSA | 1.77(1.18,2.65) | 0.006 | 1.05(1.02,1.08) | <0.001 |
| 穿刺阳性针数百分比 | 1.83(1.35,2.47) | <0.001 | 1.83(1.35,2.47) | <0.001 |
| 穿刺阳性针数 | 2.17(0.98,4.80) | 0.057 | 1.24(1.14,1.34) | <0.001 |
| 穿刺Gleason评分 | 2.25(1.63,3.10) | <0.001 | 2.14(1.67,2.74) | <0.001 |
| 穿刺神经周围侵犯 | 5.83(2.05,16.59) | 0.001 | 6.09(4.04,9.17) | <0.001 |
| 术前临床T分期 | 2.17(1.06,4.42) | 0.033 | 2.08(1.58,2.74) | <0.001 |
| 术后病理T分期 | 4.30(2.43,7.63) | <0.001 | 2.98(2.28,3.88) | <0.001 |
| 术后Gleason评分 | 2.55(1.75,3.72) | <0.001 | 2.33(1.80,3.01) | <0.001 |
表4 中国人群前列腺癌根治术后PSM危险因素的敏感性分析
Table 4 Sensitivity analysis of risk factors for PSMs after radical prostatectomy in Chinese men
| 危险因素 | 随机效应模型 | 固定效应模型 | ||
|---|---|---|---|---|
| OR(95%CI) | P值 | OR(95%CI) | P值 | |
| 术前PSA | 1.77(1.18,2.65) | 0.006 | 1.05(1.02,1.08) | <0.001 |
| 穿刺阳性针数百分比 | 1.83(1.35,2.47) | <0.001 | 1.83(1.35,2.47) | <0.001 |
| 穿刺阳性针数 | 2.17(0.98,4.80) | 0.057 | 1.24(1.14,1.34) | <0.001 |
| 穿刺Gleason评分 | 2.25(1.63,3.10) | <0.001 | 2.14(1.67,2.74) | <0.001 |
| 穿刺神经周围侵犯 | 5.83(2.05,16.59) | 0.001 | 6.09(4.04,9.17) | <0.001 |
| 术前临床T分期 | 2.17(1.06,4.42) | 0.033 | 2.08(1.58,2.74) | <0.001 |
| 术后病理T分期 | 4.30(2.43,7.63) | <0.001 | 2.98(2.28,3.88) | <0.001 |
| 术后Gleason评分 | 2.55(1.75,3.72) | <0.001 | 2.33(1.80,3.01) | <0.001 |
| 危险因素 | 排除文献 | 排除前 | 排除后 | ||||
|---|---|---|---|---|---|---|---|
| 模型 | OR(95%CI) | P值 | 模型 | OR(95%CI) | P值 | ||
| 术前PSA | [ | 随机效应模型 | 1.77(1.18,2.65) | 0.006 | 固定效应模型 | 2.31(1.88,2.83) | <0.001 |
| 穿刺阳性针数 | [ | 随机效应模型 | 2.17(0.98,4.80) | 0.057 | 固定效应模型 | 3.09(1.81,5.26) | <0.001 |
| 穿刺神经周围侵犯 | [ | 随机效应模型 | 5.83(2.05,16.59) | 0.001 | 固定效应模型 | 3.79(2.30,6.24) | <0.001 |
| 术前临床T分期 | [ | 随机效应模型 | 2.17(1.06,4.42) | 0.033 | 固定效应模型 | 1.95(1.41,2.71) | <0.001 |
| 术后病理T分期 | [ | 随机效应模型 | 4.30(2.43,7.63) | <0.001 | 固定效应模型 | 3.77(2.58,5.51) | <0.001 |
表5 中国人群前列腺癌根治术后PSM危险因素的排除分析
Table 5 Exclusion analysis of risk factors for PSMs after radical prostatectomy in Chinese men
| 危险因素 | 排除文献 | 排除前 | 排除后 | ||||
|---|---|---|---|---|---|---|---|
| 模型 | OR(95%CI) | P值 | 模型 | OR(95%CI) | P值 | ||
| 术前PSA | [ | 随机效应模型 | 1.77(1.18,2.65) | 0.006 | 固定效应模型 | 2.31(1.88,2.83) | <0.001 |
| 穿刺阳性针数 | [ | 随机效应模型 | 2.17(0.98,4.80) | 0.057 | 固定效应模型 | 3.09(1.81,5.26) | <0.001 |
| 穿刺神经周围侵犯 | [ | 随机效应模型 | 5.83(2.05,16.59) | 0.001 | 固定效应模型 | 3.79(2.30,6.24) | <0.001 |
| 术前临床T分期 | [ | 随机效应模型 | 2.17(1.06,4.42) | 0.033 | 固定效应模型 | 1.95(1.41,2.71) | <0.001 |
| 术后病理T分期 | [ | 随机效应模型 | 4.30(2.43,7.63) | <0.001 | 固定效应模型 | 3.77(2.58,5.51) | <0.001 |
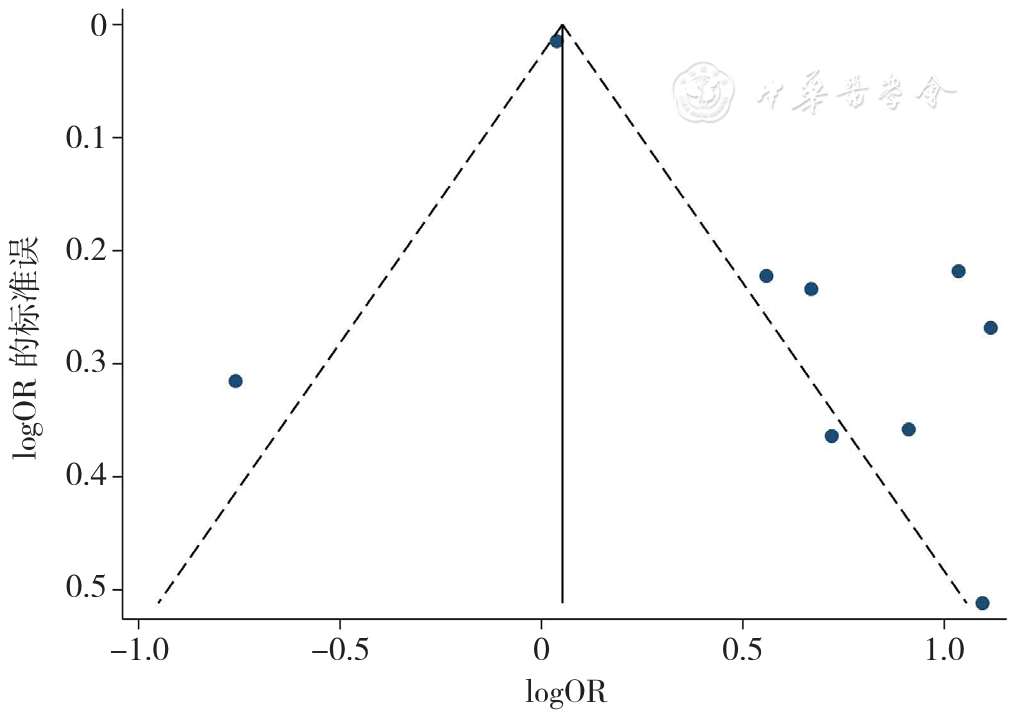
图10 术前PSA对前列腺癌根治术后PSM影响的漏斗图
Figure 10 The funnel plot assessing potential publication bias for the meta-analysis of the impact of pre-radical prostatectomy high PSA on PSMs
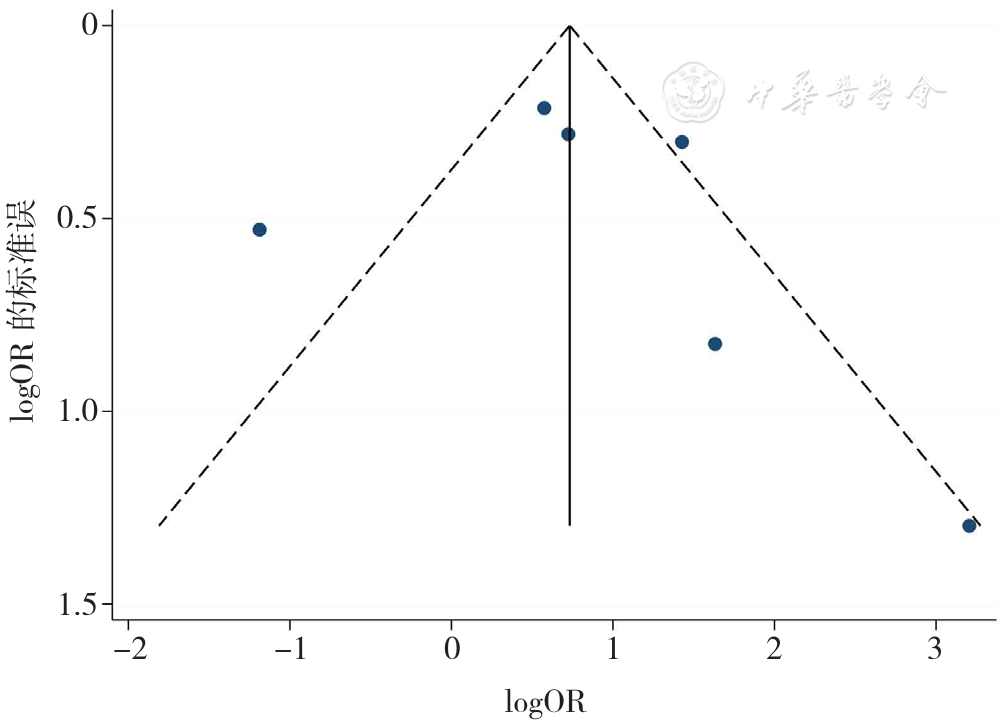
图11 术前临床T分期对前列腺癌根治术后PSM影响的漏斗图
Figure 11 The funnel plot assessing potential publication bias for the meta-analysis of the impact of pre-radical prostatectomy clinical T stage on PSMs
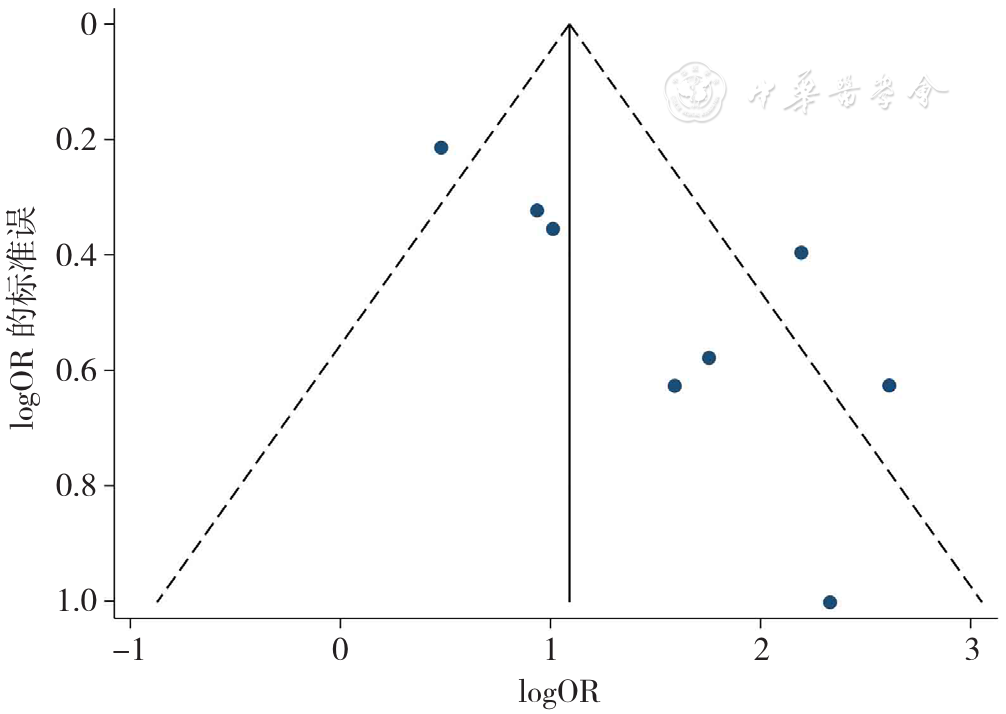
图12 术后病理T分期对前列腺癌根治术后PSM影响的漏斗图
Figure 12 The funnel plot assessing potential publication bias for the meta-analysis of the impact of post-radical prostatectomy pathological T stage on PSMs
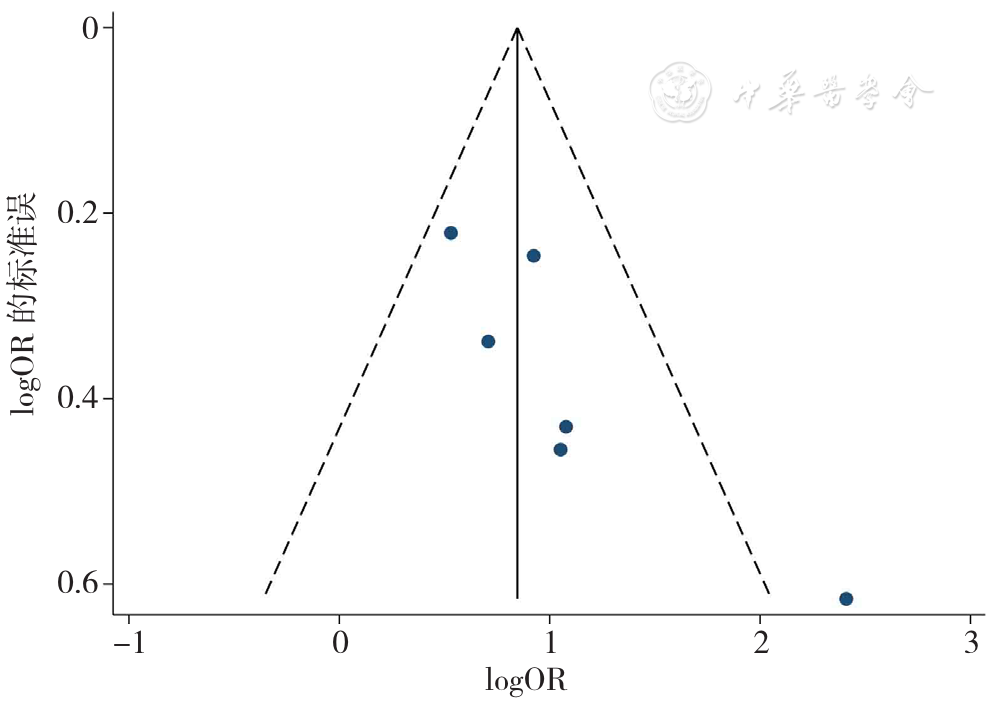
图13 术后Gleason评分对前列腺癌根治术后PSM影响的漏斗图
Figure 13 The funnel plot assessing potential publication bias for the meta-analysis of the impact of post-radical prostatectomy Gleason score on PSMs
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
张靖博. 腹膜外途径腹腔镜下根治性前列腺切除术切缘阳性的影响因素分析[J]. 中国现代医药杂志,2021,23(3):33-36. DOI:10.3969/j.issn.1672-9463.2021.03.008.
|
| [6] |
张平新,王文光,马军,等. 腹膜外途径腹腔镜下根治性前列腺切除术切缘阳性的影响因素[J]. 现代泌尿外科杂志,2020,25(3):247-251.
|
| [7] |
阎乙夫,黄毅,马潞林. 腹腔镜根治性前列腺切除术后切缘阳性的相关因素分析[J]. 临床泌尿外科杂志,2011,26(12):901-905. DOI:10.3969/j.issn.1001-1420.2011.12.006.
|
| [8] |
陈星,李炤,何裕杰. 腹腔镜前列腺癌根治术后切缘阳性的影响因素及对患者术后生化复发的影响[J]. 医学理论与实践,2021,34(21):3742-3744. DOI:10.19381/j.issn.1001-7585.2021.21.023.
|
| [9] |
张争,张克楠,洪保安,等. 腹腔镜前列腺癌根治术后切缘阳性的相关影响因素分析[J]. 中国肿瘤临床,2019,46(6):299-302. DOI:10.3969/j.issn.1000-8179.2019.06.276.
|
| [10] |
吴丹. 腹腔镜前列腺癌根治术围手术期指标影响因素分析[D]. 苏州:苏州大学,2020.
|
| [11] |
缪志俊,李鹏,徐宏博,等. 腹腔镜下前列腺癌根治术后切缘阳性的危险因素分析[J]. 现代泌尿生殖肿瘤杂志,2021,13(5):274-277.
|
| [12] |
王硕,杜鹏,曹煜东,等. 根治性前列腺切除术后前列腺尖端、基底切缘阳性的危险因素分析[J]. 中华泌尿外科杂志,2021,42(4):283-288. DOI:10.3760/cma.j.cn112330-20210106-00008.
|
| [13] |
侯惠民,江炘,刘明,等. 根治性前列腺切除术后切缘阳性的临床特征和影响因素分析[J]. 中华泌尿外科杂志,2018,39(10):740-744. DOI:10.3760/cma.j.issn.1000-6702.2018.10.004.
|
| [14] |
范效铮,权鹏鹤,张龙龙,等. 机器人辅助腹腔镜根治性前列腺切除术患者特征及切缘阳性分析[J]. 微创泌尿外科杂志,2021,10(2):105-110. DOI:10.19558/j.cnki.10-1020/r.2021.02.007.
|
| [15] |
屈武功,董彪,陶金,等. 机器人辅助腹腔镜根治性前列腺切除术后切缘阳性的影响因素分析[J]. 中华泌尿外科杂志,2021,42(4):289-293. DOI:10.3760/cma.j.cn112330-20200430-00338.
|
| [16] |
张春雷,陈锐,孔德沛,等. 机器人辅助腹腔镜根治性前列腺切除术后切缘阳性和生化复发的影响因素及相关性分析[J]. 中华泌尿外科杂志,2018,39(12):905-910. DOI:10.3760/cma.j.issn.1000-6702.2018.12.006.
|
| [17] |
沈诞. 机器人辅助腹腔镜前列腺癌根治术治疗高危前列腺癌的研究[D]. 上海:第二军医大学,2012.
|
| [18] |
瞿旻,林恒之,王海峰,等. 机器人辅助腹腔镜下根治性前列腺切除术治疗高危前列腺癌400例报告[J]. 中华泌尿外科杂志,2017,38(6):424-427. DOI:10.3760/cma.j.issn.1000-6702.2017.06.007.
|
| [19] |
韩涛. 前列腺癌穿刺活检与根治切除病理的相关性研究[D]. 南京:南京大学,2013.
|
| [20] |
张铁龙. 前列腺癌患者临床资料库的建立及数据分析[D]. 上海:上海交通大学,2015.
|
| [21] |
丁攀. 前列腺癌根治术后切缘阳性的相关因素分析及风险预测[D]. 南昌:南昌大学,2019.
|
| [22] |
洪锴,马潞林,黄毅,等. 腹腔镜下前列腺癌根治术后切缘阳性的相关因素分析[J]. 中华泌尿外科杂志,2008,29(4):271-274. DOI:10.3321/j.issn:1000-6702.2008.04.015.
|
| [23] |
|
| [24] |
|
| [25] |
|
| [26] |
闫厚煜,邢金春,张开颜,等. 前列腺癌的早期诊断研究进展[J]. 临床泌尿外科杂志,2020,35(3):242-246. DOI:10.13201/j.issn.1001-1420.2020.03.018.
|
| [27] |
|
| [28] |
|
| [29] |
赫捷,陈万青,李霓,等. 中国前列腺癌筛查与早诊早治指南(2022,北京)[J]. 中华肿瘤杂志,2022,44(1):29-53. DOI:10.3760/cma.j.cn112152-20211226-00975.
|
| [30] |
|
| [31] |
|
| [32] |
|
| [33] |
|
| [34] |
|
| [35] |
宫正,李艺,刘重远,等. 骨盆径线及其他相关参数与前列腺癌根治术后尖部切缘阳性关系的探讨[J]. 现代肿瘤医学,2018,26(24):3973-3977.
|
| [36] |
梁迎春,许宁,吴宇鹏,等. 前列腺尖部形态对腹腔镜根治性前列腺切除术后尖部切缘阳性及生化复发的影响[J]. 中华外科杂志,2019,57(3):200-205. DOI:10.3760/cma.j.issn.0529-5815.2019.03.008.
|
| [1] | 许佳兰, 阎红, 文君, 周紫彤, 王思宇. 老年癌症患者潜在不适当用药发生率的Meta分析[J]. 中国全科医学, 2025, 28(30): 3815-3822. |
| [2] | 徐百川, 王艳, 张彭, 李艺婷, 刘飞来, 谢洋. 慢性阻塞性肺疾病共病肺癌筛查工具分析[J]. 中国全科医学, 2025, 28(30): 3847-3852. |
| [3] | 邵晓颖, 邵洁, 朱焱, 邵金玲, 尚灵, 吴振莲, 赵钰, 张加才. 贵州省6~36月龄儿童铁缺乏现状及缺铁性贫血影响因素研究[J]. 中国全科医学, 2025, 28(27): 3368-3374. |
| [4] | 张天宇, 于海搏, 陈飞, 李新, 张佳佳, 詹晓凯, 申曼, 汤然, 范斯斌, 赵凤仪, 黄仲夏. POEMS综合征全身系统性治疗疗效和安全性的Meta分析[J]. 中国全科医学, 2025, 28(27): 3447-3455. |
| [5] | 全家霖, 朱琳, 苏煜, 陈泽恺, 陈梓淇, 张卓凡. 运动方式对超重或肥胖儿童青少年执行功能改善效果的网状Meta分析[J]. 中国全科医学, 2025, 28(27): 3422-3431. |
| [6] | 蒋世华, 朱政, 任盈盈, 朱垚磊, 王越, 高希彬. 中国儿童青少年近视患病率及影响因素的Meta分析[J]. 中国全科医学, 2025, 28(24): 3043-3052. |
| [7] | 李浩, 李江涛, 刘丹, 王建军. 贝利尤单抗和阿尼鲁单抗及泰它西普治疗系统性红斑狼疮疗效和安全性的网状Meta分析[J]. 中国全科医学, 2025, 28(23): 2924-2933. |
| [8] | 王笑林, 李秋月, 周彦君, 张金辉, 梁涛. 转移性结直肠癌患者呋喹替尼治疗相关心血管毒性发生率和风险的Meta分析[J]. 中国全科医学, 2025, 28(23): 2934-2940. |
| [9] | 周倩, 吴晓敏, 王宝华, 严若菡, 蔚苗, 吴静. 胃癌发生风险的列线图预测模型研究[J]. 中国全科医学, 2025, 28(23): 2870-2877. |
| [10] | 马盼盼, 王思静, 游娜, 丁大法, 鲁一兵. Danuglipron与Orforglipron治疗2型糖尿病疗效及安全性的Meta分析[J]. 中国全科医学, 2025, 28(21): 2679-2685. |
| [11] | 胡婉琴, 余深艳, 曹学华, 向凤, 贾钰. 中国儿童性早熟影响因素的Meta分析[J]. 中国全科医学, 2025, 28(21): 2661-2671. |
| [12] | 阿迪力·吐尔孙, 程刚. 非奈利酮治疗2型糖尿病肾病有效性和安全性的Meta分析[J]. 中国全科医学, 2025, 28(21): 2686-2691. |
| [13] | 郭盛滕, 张芬芬, 万迪, 于冬梅, 王庆华. 重症急性胰腺炎并发急性肺损伤危险因素的Meta分析[J]. 中国全科医学, 2025, 28(20): 2546-2554. |
| [14] | 王碧晴, 张萍, 杨红霞, 王倩, 鞠春晓, 赵俊男, 梅俊, 张颖, 徐凤芹. 中国老年高血压患者轻度认知障碍患病率及发展趋势的Meta分析[J]. 中国全科医学, 2025, 28(17): 2186-2192. |
| [15] | 樊宇, 李蓉, 龚双英, 杨小娟, 李蕊. 中国产妇配偶产后抑郁发生率的Meta分析[J]. 中国全科医学, 2025, 28(17): 2179-2185. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





