中国全科医学 ›› 2022, Vol. 25 ›› Issue (18): 2207-2214.DOI: 10.12114/j.issn.1007-9572.2022.02.021
所属专题: 内分泌代谢性疾病最新文章合辑; 骨健康最新文章合辑; 骨质疏松最新文章合辑
收稿日期:2021-10-29
修回日期:2022-01-12
出版日期:2022-06-20
发布日期:2022-02-24
通讯作者:
吴文迅
基金资助:
Huifang NI, Jun LI, Yuan DING, Qun FU, Wenxun WU*( )
)
Received:2021-10-29
Revised:2022-01-12
Published:2022-06-20
Online:2022-02-24
Contact:
Wenxun WU
About author:摘要: 背景 糖尿病患者并发骨质疏松症(OP)的风险较大,尤其是绝经后2型糖尿病(T2DM)患者,慢性炎症在其中起着重要作用。 目的 探讨中性粒细胞/淋巴细胞比值(NLR)和单核细胞/高密度脂蛋白胆固醇比值(MHR)对绝经后T2DM患者发生OP的预测价值。 方法 选取2018年1月至2020年1月于郑州大学第一附属医院内分泌及代谢性疾病科住院的216例绝经后T2DM患者,收集患者的临床资料。采集患者空腹静脉血,测定血常规、血脂等生化指标,计算得到NLR和MHR;采用双能X线吸收法(DXA)测定患者腰椎L1~4、左股骨颈及左髋骨密度(BMD)。根据BMD结果,将患者分为骨量正常组51例、骨量减少组78例、OP组87例,另外根据NLR四分位数(A1~A4组)和MHR四分位数(B1~B4组)将患者分为4组,每组54例。采用Spearman秩相关分析探讨NLR和MHR与各部位BMD的相关性,多因素Logistic回归分析探讨绝经后T2DM患者发生OP的影响因素,受试者工作特征(ROC)曲线评价NLR、MHR及两者联合预测绝经后T2DM患者发生OP的价值。 结果 骨量减少组NLR、MHR均高于骨量正常组(P<0.05),OP组NLR、MHR均高于骨量正常组和骨量减少组(P<0.05)。A3组L1~4 、左股骨颈、左髋BMD均低于A1组(P<0.05);A4组左股骨颈BMD低于A1组,L1~4 、左髋BMD低于A1组和A2组(P<0.05)。B2、B3组L1~4 、左股骨颈、左髋BMD均低于B1组(P<0.05);B4组L1~4 BMD低于B1组、B2组和B3组,左股骨颈、左髋BMD均低于B1组和B2组(P<0.05)。Spearman秩相关分析结果显示,NLR、MHR均分别与L1~4 、左股骨颈、左髋BMD呈负相关(P<0.001)。多因素Logistic回归分析结果显示,绝经年限长〔OR=1.092,95%CI(1.005,1.186)〕、NLR水平升高〔OR=2.341,95%CI(1.453,3.770)〕和MHR水平升高〔OR=329.250,95%CI(21.421,5 060.810)〕是绝经后T2DM患者发生OP的独立危险因素(P<0.05),体质指数(BMI)升高〔OR=0.806,95%CI(0.718,0.903)〕是绝经后T2DM患者发生OP的独立保护因素(P<0.05)。ROC曲线分析结果显示,NLR、MHR及两者联合预测绝经后T2DM患者发生OP的ROC曲线下面积分别为0.722、0.709、0.787,灵敏度分别为65.5%、52.9%、81.6%,特异度分别为72.1%、79.8%、67.4%;两者联合预测绝经后T2DM患者发生OP的ROC曲线下面积分别高于NLR、MHR(Z=2.418,P<0.05;Z=2.893,P<0.05)。 结论 NLR和MHR均可单独作为绝经后T2DM患者发生OP的预测指标,且两者联合检测时预测效能及灵敏度更高。
| 组别 | 例数 | 年龄(岁) | 绝经年限(年) | 糖尿病病程(年) | BMI(kg/m2) | NEU(×109/L) | LYM(×109/L) |
|---|---|---|---|---|---|---|---|
| 骨量正常组 | 51 | 57.0(56.0,61.0) | 7.0(5.0,9.0) | 9.0(2.0,10.0) | 24.8(23.4,27.1) | 3.27(3.00,3.78) | 1.60(1.30,2.03) |
| 骨量减少组 | 78 | 58.5(55.0,65.2) | 11.0(4.0,16.2)a | 8.0(3.8,15.0) | 24.5(22.5,26.7) | 3.27(2.68,3.98) | 1.61(1.27,1.93) |
| OP组 | 87 | 66.0(57.0,71.0)ab | 17.0(10.0,22.0)ab | 9.6(5.0,15.0) | 23.2(21.2,25.7)ab | 3.68(2.96,4.17) | 1.51(1.16,2.00) |
| H值 | 17.850 | 29.760 | 4.188 | 10.580 | 4.755 | 3.083 | |
| P值 | <0.001 | <0.001 | 0.123 | 0.005 | 0.093 | 0.214 | |
| 组别 | MON(×109/L) | NLR | HbA1c(%) | FBG(mmol/L) | TG(mmol/L) | TC(mmol/L) | |
| 骨量正常组 | 0.35(0.30,0.44) | 1.93(1.43,2.08) | 8.4(7.0,10.1) | 7.97(6.72,9.23) | 1.28(0.94,1.64) | 4.09(3.76,5.02) | |
| 骨量减少组 | 0.36(0.29,0.43) | 2.04(1.67,2.48)a | 7.6(6.9,9.7) | 7.93(6.52,9.12) | 1.29(0.93,1.93) | 4.60(3.88,5.12) | |
| OP组 | 0.41(0.32,0.51)ab | 2.43(2.02,3.11)ab | 7.8(7.0,9.7) | 8.61(7.54,9.53)ab | 1.51(1.12,2.01) | 4.55(3.93,5.09) | |
| H值 | 8.814 | 35.120 | 0.708 | 7.333 | 2.708 | 2.338 | |
| P值 | 0.012 | <0.001 | 0.702 | 0.026 | 0.258 | 0.311 | |
| 组别 | HDL-C(mmol/L) | LDL-C(mmol/L) | MHR | L1~4 BMD(g/cm2) | 左股骨颈BMD(g/cm2) | 左髋BMD(g/cm2) | |
| 骨量正常组 | 1.12(1.00,1.30) | 2.39(1.59,3.33) | 0.25(0.20,0.31) | 1.08(0.97,1.16) | 0.83(0.80,0.90) | 0.96(0.92,1.02) | |
| 骨量减少组 | 1.13(1.00,1.37) | 2.63(1.92,3.46) | 0.31(0.24,0.39)a | 0.88(0.83,0.92)a | 0.67(0.65,0.72)a | 0.80(0.76,0.85)a | |
| OP组 | 1.08(0.95,1.30) | 2.72(1.95,3.33) | 0.38(0.28,0.49)ab | 0.72(0.67,0.77)ab | 0.60(0.51,0.66)ab | 0.71(0.63,0.76)ab | |
| H值 | 1.432 | 2.000 | 38.030 | 157.600 | 120.500 | 126.100 | |
| P值 | 0.489 | 0.368 | <0.001 | <0.001 | <0.001 | <0.001 |
表1 骨量正常组、骨量减少组、OP组临床资料比较〔M(P25,P75)〕
Table 1 Comparison of clinical data across postmenopausal T2DM patients with different BMD levels
| 组别 | 例数 | 年龄(岁) | 绝经年限(年) | 糖尿病病程(年) | BMI(kg/m2) | NEU(×109/L) | LYM(×109/L) |
|---|---|---|---|---|---|---|---|
| 骨量正常组 | 51 | 57.0(56.0,61.0) | 7.0(5.0,9.0) | 9.0(2.0,10.0) | 24.8(23.4,27.1) | 3.27(3.00,3.78) | 1.60(1.30,2.03) |
| 骨量减少组 | 78 | 58.5(55.0,65.2) | 11.0(4.0,16.2)a | 8.0(3.8,15.0) | 24.5(22.5,26.7) | 3.27(2.68,3.98) | 1.61(1.27,1.93) |
| OP组 | 87 | 66.0(57.0,71.0)ab | 17.0(10.0,22.0)ab | 9.6(5.0,15.0) | 23.2(21.2,25.7)ab | 3.68(2.96,4.17) | 1.51(1.16,2.00) |
| H值 | 17.850 | 29.760 | 4.188 | 10.580 | 4.755 | 3.083 | |
| P值 | <0.001 | <0.001 | 0.123 | 0.005 | 0.093 | 0.214 | |
| 组别 | MON(×109/L) | NLR | HbA1c(%) | FBG(mmol/L) | TG(mmol/L) | TC(mmol/L) | |
| 骨量正常组 | 0.35(0.30,0.44) | 1.93(1.43,2.08) | 8.4(7.0,10.1) | 7.97(6.72,9.23) | 1.28(0.94,1.64) | 4.09(3.76,5.02) | |
| 骨量减少组 | 0.36(0.29,0.43) | 2.04(1.67,2.48)a | 7.6(6.9,9.7) | 7.93(6.52,9.12) | 1.29(0.93,1.93) | 4.60(3.88,5.12) | |
| OP组 | 0.41(0.32,0.51)ab | 2.43(2.02,3.11)ab | 7.8(7.0,9.7) | 8.61(7.54,9.53)ab | 1.51(1.12,2.01) | 4.55(3.93,5.09) | |
| H值 | 8.814 | 35.120 | 0.708 | 7.333 | 2.708 | 2.338 | |
| P值 | 0.012 | <0.001 | 0.702 | 0.026 | 0.258 | 0.311 | |
| 组别 | HDL-C(mmol/L) | LDL-C(mmol/L) | MHR | L1~4 BMD(g/cm2) | 左股骨颈BMD(g/cm2) | 左髋BMD(g/cm2) | |
| 骨量正常组 | 1.12(1.00,1.30) | 2.39(1.59,3.33) | 0.25(0.20,0.31) | 1.08(0.97,1.16) | 0.83(0.80,0.90) | 0.96(0.92,1.02) | |
| 骨量减少组 | 1.13(1.00,1.37) | 2.63(1.92,3.46) | 0.31(0.24,0.39)a | 0.88(0.83,0.92)a | 0.67(0.65,0.72)a | 0.80(0.76,0.85)a | |
| OP组 | 1.08(0.95,1.30) | 2.72(1.95,3.33) | 0.38(0.28,0.49)ab | 0.72(0.67,0.77)ab | 0.60(0.51,0.66)ab | 0.71(0.63,0.76)ab | |
| H值 | 1.432 | 2.000 | 38.030 | 157.600 | 120.500 | 126.100 | |
| P值 | 0.489 | 0.368 | <0.001 | <0.001 | <0.001 | <0.001 |
| 组别 | 例数 | 年龄(岁) | 绝经年限(年) | 糖尿病病程(年) | BMI(kg/m2) | NEU(×109/L) | LYM(×109/L) |
|---|---|---|---|---|---|---|---|
| A1组 | 54 | 58.0(55.0,64.2) | 8.5(4.0,16.2) | 9.0(3.0,12.0) | 24.2(22.8,27.2) | 3.04(2.42,3.30) | 1.88(1.51,2.08) |
| A2组 | 54 | 58.5(56.0,66.2) | 9.0(6.75,15.2) | 7.0(2.0,11.2) | 24.2(21.8,25.9) | 3.33(2.68,3.88)a | 1.66(1.39,2.02) |
| A3组 | 54 | 62.0(56.0,69.0) | 14.0(6.0,20.0)a | 10.0(5.0,15.0) | 24.1(22.6,26.4) | 3.50(2.77,4.29)a | 1.56(1.19,1.96)a |
| A4组 | 54 | 64.0(57.0,69.0) | 15.0(6.8,21.2)ab | 9.3(3.0,15.2) | 24.0(22.0,26.8) | 3.96(3.54,4.84)abc | 1.25(1.13,1.52)abc |
| H值 | 6.793 | 9.228 | 4.342 | 1.137 | 51.740 | 35.340 | |
| P值 | 0.079 | 0.026 | 0.227 | 0.768 | <0.001 | <0.001 | |
| 组别 | MON(×109/L) | NLR | HbA1c(%) | FBG(mmol/L) | TG(mmol/L) | TC(mmol/L) | |
| A1组 | 0.34(0.30,0.41) | 1.56(1.36,1.67) | 7.85(6.60,9.53) | 7.28(6.37,8.54) | 1.19(0.83,1.56) | 4.20(3.73,5.13) | |
| A2组 | 0.39(0.31,0.47) | 1.98(1.91,2.04)a | 7.60(7.08,10.10) | 8.06(7.09,9.21)a | 1.47(0.95,1.94) | 4.60(4.01,5.03) | |
| A3组 | 0.36(0.31,0.47) | 2.30(2.18,2.46)ab | 7.95(7.20,9.23) | 8.80(7.98,9.79)ab | 1.56(1.21,1.92)a | 4.51(3.80,5.09) | |
| A4组 | 0.40(0.32,0.51) | 3.27(2.90,3.79)abc | 8.20(6.88,10.20) | 8.34(7.28,9.51)a | 1.41(1.01,1.95)a | 4.40(3.75,5.13) | |
| H值 | 6.683 | 201.514 | 1.716 | 18.906 | 8.887 | 0.485 | |
| P值 | 0.083 | <0.001 | 0.633 | <0.001 | 0.031 | 0.922 | |
| 组别 | HDL-C(mmol/L) | LDL-C(mmol/L) | MHR | L1~4 BMD(g/cm2) | 左股骨颈BMD(g/cm2) | 左髋BMD(g/cm2) | |
| A1组 | 1.13(0.96,1.30) | 2.41(1.79,3.40) | 0.29(0.23,0.35) | 0.92(0.85,0.98) | 0.74(0.65,0.81) | 0.84(0.78,0.92) | |
| A2组 | 1.09(1.00,1.28) | 2.73(2.13,3.33) | 0.31(0.21,0.41) | 0.88(0.76,1.00) | 0.67(0.60,0.81) | 0.81(0.73,0.93) | |
| A3组 | 1.08(0.96,1.29) | 2.79(2.00,3.42) | 0.32(0.25,0.42) | 0.80(0.72,0.95)a | 0.67(0.59,0.73)a | 0.76(0.70,0.85)a | |
| A4组 | 1.13(0.94,1.42) | 2.45(1.91,3.22) | 0.35(0.27,0.47)a | 0.80(0.71,0.89)ab | 0.65(0.59,0.70)a | 0.75(0.70,0.83)ab | |
| H值 | 0.505 | 1.601 | 8.553 | 19.105 | 12.322 | 13.842 | |
| P值 | 0.918 | 0.659 | 0.036 | <0.001 | 0.006 | 0.003 |
表2 根据NLR四分位数分组的各组临床资料比较〔M(P25,P75)〕
Table 2 Comparison of clinical data across NLR quartile groups of postmenopausal T2DM patients
| 组别 | 例数 | 年龄(岁) | 绝经年限(年) | 糖尿病病程(年) | BMI(kg/m2) | NEU(×109/L) | LYM(×109/L) |
|---|---|---|---|---|---|---|---|
| A1组 | 54 | 58.0(55.0,64.2) | 8.5(4.0,16.2) | 9.0(3.0,12.0) | 24.2(22.8,27.2) | 3.04(2.42,3.30) | 1.88(1.51,2.08) |
| A2组 | 54 | 58.5(56.0,66.2) | 9.0(6.75,15.2) | 7.0(2.0,11.2) | 24.2(21.8,25.9) | 3.33(2.68,3.88)a | 1.66(1.39,2.02) |
| A3组 | 54 | 62.0(56.0,69.0) | 14.0(6.0,20.0)a | 10.0(5.0,15.0) | 24.1(22.6,26.4) | 3.50(2.77,4.29)a | 1.56(1.19,1.96)a |
| A4组 | 54 | 64.0(57.0,69.0) | 15.0(6.8,21.2)ab | 9.3(3.0,15.2) | 24.0(22.0,26.8) | 3.96(3.54,4.84)abc | 1.25(1.13,1.52)abc |
| H值 | 6.793 | 9.228 | 4.342 | 1.137 | 51.740 | 35.340 | |
| P值 | 0.079 | 0.026 | 0.227 | 0.768 | <0.001 | <0.001 | |
| 组别 | MON(×109/L) | NLR | HbA1c(%) | FBG(mmol/L) | TG(mmol/L) | TC(mmol/L) | |
| A1组 | 0.34(0.30,0.41) | 1.56(1.36,1.67) | 7.85(6.60,9.53) | 7.28(6.37,8.54) | 1.19(0.83,1.56) | 4.20(3.73,5.13) | |
| A2组 | 0.39(0.31,0.47) | 1.98(1.91,2.04)a | 7.60(7.08,10.10) | 8.06(7.09,9.21)a | 1.47(0.95,1.94) | 4.60(4.01,5.03) | |
| A3组 | 0.36(0.31,0.47) | 2.30(2.18,2.46)ab | 7.95(7.20,9.23) | 8.80(7.98,9.79)ab | 1.56(1.21,1.92)a | 4.51(3.80,5.09) | |
| A4组 | 0.40(0.32,0.51) | 3.27(2.90,3.79)abc | 8.20(6.88,10.20) | 8.34(7.28,9.51)a | 1.41(1.01,1.95)a | 4.40(3.75,5.13) | |
| H值 | 6.683 | 201.514 | 1.716 | 18.906 | 8.887 | 0.485 | |
| P值 | 0.083 | <0.001 | 0.633 | <0.001 | 0.031 | 0.922 | |
| 组别 | HDL-C(mmol/L) | LDL-C(mmol/L) | MHR | L1~4 BMD(g/cm2) | 左股骨颈BMD(g/cm2) | 左髋BMD(g/cm2) | |
| A1组 | 1.13(0.96,1.30) | 2.41(1.79,3.40) | 0.29(0.23,0.35) | 0.92(0.85,0.98) | 0.74(0.65,0.81) | 0.84(0.78,0.92) | |
| A2组 | 1.09(1.00,1.28) | 2.73(2.13,3.33) | 0.31(0.21,0.41) | 0.88(0.76,1.00) | 0.67(0.60,0.81) | 0.81(0.73,0.93) | |
| A3组 | 1.08(0.96,1.29) | 2.79(2.00,3.42) | 0.32(0.25,0.42) | 0.80(0.72,0.95)a | 0.67(0.59,0.73)a | 0.76(0.70,0.85)a | |
| A4组 | 1.13(0.94,1.42) | 2.45(1.91,3.22) | 0.35(0.27,0.47)a | 0.80(0.71,0.89)ab | 0.65(0.59,0.70)a | 0.75(0.70,0.83)ab | |
| H值 | 0.505 | 1.601 | 8.553 | 19.105 | 12.322 | 13.842 | |
| P值 | 0.918 | 0.659 | 0.036 | <0.001 | 0.006 | 0.003 |
| 组别 | 例数 | 年龄(岁) | 绝经年限(年) | 糖尿病病程(年) | BMI(kg/m2) | NEU(×109/L) | LYM(×109/L) |
|---|---|---|---|---|---|---|---|
| B1组 | 54 | 59.5(54.0,67.0) | 9.5(3.0,15.5) | 8.0(3.0,11.2) | 24.0(22.0,27.4) | 3.12(2.71,3.53) | 1.51(1.18,1.85) |
| B2组 | 54 | 59.5(56.0,67.2) | 9.0(6.0,19.2) | 10.0(6.0,15.0) | 24.1(22.9,26.1) | 3.18(2.51,3.75) | 1.41(1.17,1.81) |
| B3组 | 54 | 59.0(56.0,68.0) | 12.0(6.0,19.2) | 6.0(2.0,12.0)b | 23.6(21.6,26.0) | 3.44(2.94,3.85)ab | 1.56(1.27,2.02) |
| B4组 | 54 | 62.0(56.8,69.2) | 14.0(7.8,22.8) | 10.0(5.8,16.2)ac | 24.4(21.9,26.2) | 4.09(3.51,4.47)abc | 1.88(1.39,2.06)ab |
| H值 | 3.273 | 7.674 | 11.474 | 2.424 | 32.436 | 13.118 | |
| P值 | 0.351 | 0.053 | 0.009 | 0.489 | <0.001 | 0.004 | |
| 组别 | MON(×109/L) | NLR | HbA1c(%) | FBG(mmol/L) | TG(mmol/L) | TC(mmol/L) | |
| B1组 | 0.34(0.26,0.41) | 2.01(1.64,2.25) | 7.65(6.53,10.10) | 8.14(7.10,9.72) | 1.27(0.94,1.65) | 4.62(3.81,5.12) | |
| B2组 | 0.32(0.29,0.36) | 2.06(1.63,2.66) | 7.80(6.80,9.53) | 8.04(6.70,9.26) | 1.26(0.96,1.66) | 4.63(3.88,5.13) | |
| B3组 | 0.38(0.31,0.44)ab | 2.21(1.95,2.74)a | 7.75(7.00,9.25) | 8.34(7.04,9.56) | 1.34(0.84,1.88) | 4.75(3.87,5.16) | |
| B4组 | 0.51(0.44,0.57)abc | 2.24(1.93,3.10)a | 8.30(7.25,10.20) | 8.25(7.30,9.29) | 1.67(1.23,2.21)abc | 4.16(3.61,4.69)abc | |
| H值 | 83.859 | 8.636 | 4.410 | 0.962 | 10.846 | 10.146 | |
| P值 | <0.001 | 0.035 | 0.220 | 0.810 | 0.013 | 0.017 | |
| 组别 | HDL-C(mmol/L) | LDL-C(mmol/L) | MHR | L1~4 BMD(g/cm2) | 左股骨颈BMD(g/cm2) | 左髋BMD(g/cm2) | |
| B1组 | 1.31(1.07,1.60) | 2.59(1.80,3.33) | 0.20(0.17,0.23) | 0.94(0.82,1.08) | 0.76(0.67,0.84) | 0.86(0.77,0.97) | |
| B2组 | 1.13(1.04,1.30)a | 2.72(1.98,3.51) | 0.28(0.27,0.29)a | 0.86(0.74,0.98)a | 0.67(0.62,0.80)a | 0.80(0.72,0.92)a | |
| B3组 | 1.13(0.97,1.28)a | 2.85(2.15,3.62) | 0.35(0.32,0.38)ab | 0.83(0.75,0.94)a | 0.67(0.59,0.76)a | 0.79(0.70,0.85)a | |
| B4组 | 0.96(0.83,1.07)abc | 2.15(1.68,2.94)bc | 0.51(0.46,0.60)abc | 0.77(0.70,0.87)abc | 0.64(0.59,0.68)ab | 0.75(0.70,0.81)ab | |
| H值 | 55.039 | 11.596 | 201.132 | 24.979 | 24.781 | 18.683 | |
| P值 | <0.001 | 0.009 | <0.001 | <0.001 | <0.001 | <0.001 |
表3 根据MHR四分位数分组的各组临床资料比较〔M(P25,P75)〕
Table 3 Comparison of clinical data across MHR quartile groups of postmenopausal T2DM patients
| 组别 | 例数 | 年龄(岁) | 绝经年限(年) | 糖尿病病程(年) | BMI(kg/m2) | NEU(×109/L) | LYM(×109/L) |
|---|---|---|---|---|---|---|---|
| B1组 | 54 | 59.5(54.0,67.0) | 9.5(3.0,15.5) | 8.0(3.0,11.2) | 24.0(22.0,27.4) | 3.12(2.71,3.53) | 1.51(1.18,1.85) |
| B2组 | 54 | 59.5(56.0,67.2) | 9.0(6.0,19.2) | 10.0(6.0,15.0) | 24.1(22.9,26.1) | 3.18(2.51,3.75) | 1.41(1.17,1.81) |
| B3组 | 54 | 59.0(56.0,68.0) | 12.0(6.0,19.2) | 6.0(2.0,12.0)b | 23.6(21.6,26.0) | 3.44(2.94,3.85)ab | 1.56(1.27,2.02) |
| B4组 | 54 | 62.0(56.8,69.2) | 14.0(7.8,22.8) | 10.0(5.8,16.2)ac | 24.4(21.9,26.2) | 4.09(3.51,4.47)abc | 1.88(1.39,2.06)ab |
| H值 | 3.273 | 7.674 | 11.474 | 2.424 | 32.436 | 13.118 | |
| P值 | 0.351 | 0.053 | 0.009 | 0.489 | <0.001 | 0.004 | |
| 组别 | MON(×109/L) | NLR | HbA1c(%) | FBG(mmol/L) | TG(mmol/L) | TC(mmol/L) | |
| B1组 | 0.34(0.26,0.41) | 2.01(1.64,2.25) | 7.65(6.53,10.10) | 8.14(7.10,9.72) | 1.27(0.94,1.65) | 4.62(3.81,5.12) | |
| B2组 | 0.32(0.29,0.36) | 2.06(1.63,2.66) | 7.80(6.80,9.53) | 8.04(6.70,9.26) | 1.26(0.96,1.66) | 4.63(3.88,5.13) | |
| B3组 | 0.38(0.31,0.44)ab | 2.21(1.95,2.74)a | 7.75(7.00,9.25) | 8.34(7.04,9.56) | 1.34(0.84,1.88) | 4.75(3.87,5.16) | |
| B4组 | 0.51(0.44,0.57)abc | 2.24(1.93,3.10)a | 8.30(7.25,10.20) | 8.25(7.30,9.29) | 1.67(1.23,2.21)abc | 4.16(3.61,4.69)abc | |
| H值 | 83.859 | 8.636 | 4.410 | 0.962 | 10.846 | 10.146 | |
| P值 | <0.001 | 0.035 | 0.220 | 0.810 | 0.013 | 0.017 | |
| 组别 | HDL-C(mmol/L) | LDL-C(mmol/L) | MHR | L1~4 BMD(g/cm2) | 左股骨颈BMD(g/cm2) | 左髋BMD(g/cm2) | |
| B1组 | 1.31(1.07,1.60) | 2.59(1.80,3.33) | 0.20(0.17,0.23) | 0.94(0.82,1.08) | 0.76(0.67,0.84) | 0.86(0.77,0.97) | |
| B2组 | 1.13(1.04,1.30)a | 2.72(1.98,3.51) | 0.28(0.27,0.29)a | 0.86(0.74,0.98)a | 0.67(0.62,0.80)a | 0.80(0.72,0.92)a | |
| B3组 | 1.13(0.97,1.28)a | 2.85(2.15,3.62) | 0.35(0.32,0.38)ab | 0.83(0.75,0.94)a | 0.67(0.59,0.76)a | 0.79(0.70,0.85)a | |
| B4组 | 0.96(0.83,1.07)abc | 2.15(1.68,2.94)bc | 0.51(0.46,0.60)abc | 0.77(0.70,0.87)abc | 0.64(0.59,0.68)ab | 0.75(0.70,0.81)ab | |
| H值 | 55.039 | 11.596 | 201.132 | 24.979 | 24.781 | 18.683 | |
| P值 | <0.001 | 0.009 | <0.001 | <0.001 | <0.001 | <0.001 |
| 项目 | L1~4 BMD | 左股骨颈BMD | 左髋BMD | |||
|---|---|---|---|---|---|---|
| rs值 | P值 | rs值 | P值 | rs值 | P值 | |
| 年龄 | -0.239 | <0.001 | -0.24 | <0.001 | -0.295 | <0.001 |
| 绝经年限 | -0.329 | <0.001 | -0.279 | <0.001 | -0.306 | <0.001 |
| BMI | 0.254 | <0.001 | 0.275 | <0.001 | 0.295 | <0.001 |
| MON | -0.082 | 0.116 | -0.044 | 0.261 | 0.008 | 0.453 |
| NLR | -0.317 | <0.001 | -0.269 | <0.001 | -0.272 | <0.001 |
| FBG | -0.142 | 0.018 | -0.156 | 0.011 | -0.121 | 0.038 |
| MHR | -0.316 | <0.001 | -0.311 | <0.001 | -0.271 | <0.001 |
表4 NLR和MHR与各部位BMD的相关性分析
Table 4 Correlation analysis of NLR and MHR with BMD at lumbar spine L1-4,left femoral neck and left hip in postmenopausal T2DM patients
| 项目 | L1~4 BMD | 左股骨颈BMD | 左髋BMD | |||
|---|---|---|---|---|---|---|
| rs值 | P值 | rs值 | P值 | rs值 | P值 | |
| 年龄 | -0.239 | <0.001 | -0.24 | <0.001 | -0.295 | <0.001 |
| 绝经年限 | -0.329 | <0.001 | -0.279 | <0.001 | -0.306 | <0.001 |
| BMI | 0.254 | <0.001 | 0.275 | <0.001 | 0.295 | <0.001 |
| MON | -0.082 | 0.116 | -0.044 | 0.261 | 0.008 | 0.453 |
| NLR | -0.317 | <0.001 | -0.269 | <0.001 | -0.272 | <0.001 |
| FBG | -0.142 | 0.018 | -0.156 | 0.011 | -0.121 | 0.038 |
| MHR | -0.316 | <0.001 | -0.311 | <0.001 | -0.271 | <0.001 |
| 变量 | B | SE | Wald χ2值 | P值 | OR值 | 95%CI |
|---|---|---|---|---|---|---|
| 年龄 | -0.005 | 0.045 | 0.013 | 0.908 | 0.995 | (0.911,1.086) |
| 绝经年限 | 0.088 | 0.042 | 4.313 | 0.038 | 1.092 | (1.005,1.186) |
| BMI | -0.216 | 0.058 | 13.686 | <0.001 | 0.806 | (0.718,0.903) |
| NLR | 0.850 | 0.243 | 12.224 | <0.001 | 2.341 | (1.453,3.770) |
| FBG | 0.069 | 0.079 | 0.776 | 0.378 | 1.072 | (0.919,1.251) |
| MHR | 5.797 | 1.394 | 17.289 | <0.001 | 329.250 | (21.421,5 060.810) |
| 常量 | -0.607 | 2.963 | 0.042 | 0.838 | 0.545 | — |
表5 绝经后T2DM患者发生OP影响因素的多因素Logistic回归分析
Table 5 Multivariate Logistic regression analysis of influencing factors for osteoporosis in postmenopausal T2DM patients
| 变量 | B | SE | Wald χ2值 | P值 | OR值 | 95%CI |
|---|---|---|---|---|---|---|
| 年龄 | -0.005 | 0.045 | 0.013 | 0.908 | 0.995 | (0.911,1.086) |
| 绝经年限 | 0.088 | 0.042 | 4.313 | 0.038 | 1.092 | (1.005,1.186) |
| BMI | -0.216 | 0.058 | 13.686 | <0.001 | 0.806 | (0.718,0.903) |
| NLR | 0.850 | 0.243 | 12.224 | <0.001 | 2.341 | (1.453,3.770) |
| FBG | 0.069 | 0.079 | 0.776 | 0.378 | 1.072 | (0.919,1.251) |
| MHR | 5.797 | 1.394 | 17.289 | <0.001 | 329.250 | (21.421,5 060.810) |
| 常量 | -0.607 | 2.963 | 0.042 | 0.838 | 0.545 | — |
| 指标 | AUC | 95%CI | 截断值 | P值 | 灵敏度(%) | 特异度(%) | 约登指数 |
|---|---|---|---|---|---|---|---|
| NLR | 0.722 | (0.656,0.789) | 2.202 | <0.001 | 65.5 | 72.1 | 0.376 |
| MHR | 0.709 | (0.640,0.777) | 0.368 | <0.001 | 52.9 | 79.8 | 0.327 |
| 两者联合 | 0.787 | (0.727,0.847) | — | <0.001 | 81.6 | 67.4 | 0.491 |
表6 NLR、MHR及两者联合对绝经后T2DM患者发生OP的预测价值分析
Table 6 Value of NLR,MHR and their combination in predicting osteoporosis in postmenopausal T2DM patients
| 指标 | AUC | 95%CI | 截断值 | P值 | 灵敏度(%) | 特异度(%) | 约登指数 |
|---|---|---|---|---|---|---|---|
| NLR | 0.722 | (0.656,0.789) | 2.202 | <0.001 | 65.5 | 72.1 | 0.376 |
| MHR | 0.709 | (0.640,0.777) | 0.368 | <0.001 | 52.9 | 79.8 | 0.327 |
| 两者联合 | 0.787 | (0.727,0.847) | — | <0.001 | 81.6 | 67.4 | 0.491 |
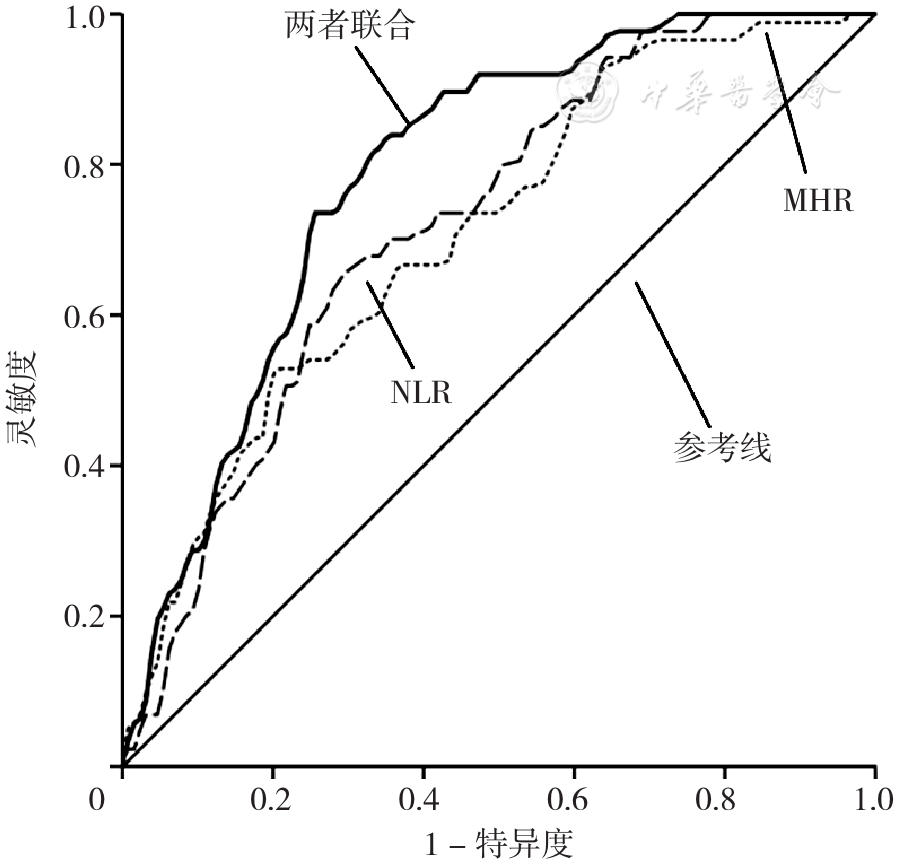
图1 NLR、MHR及两者联合预测绝经后T2DM患者发生OP的ROC曲线注:NLR=中性粒细胞/淋巴细胞比值,MHR=单核细胞/高密度脂蛋白胆固醇比值
Figure 1 ROC curve of NLR,MHR and their combination in predicting osteoporosis in postmenopausal T2DM patients
| [1] |
中华医学会骨质疏松和骨矿盐疾病分会. 原发性骨质疏松症诊疗指南(2017)[J]. 中国骨质疏松杂志,2019,25(3):281-309. DOI:10.3969/j.issn.1006-7108.2019.03.001.
|
| [2] |
周高晋,邓力军,王莲朋,等. 绝经后2型糖尿病女性骨代谢与脂代谢间的差异性[J]. 中国临床研究,2020,33(11):1463-1467. DOI:10.13429/j.cnki.cjcr.2020.11.004.
|
| [3] |
|
| [4] |
|
| [5] |
朱光,陆雨纯,沃眉宏,等. 老年2型糖尿病患者单核细胞/高密度脂蛋白胆固醇比值与骨质疏松相关性研究[J]. 中国骨质疏松杂志,2020,26(11):1572-1576. DOI:10.3969/j.issn.1006-7108.2020.11.003.
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
徐园园,卢学超,解其华,等. 绝经后2型糖尿病患者外周血中性粒细胞/淋巴细胞比值与骨密度的关系[J]. 中国骨质疏松杂志,2018,24(11):1464-1467. DOI:10.3969/j.issn.1006-7108.2018.11.014.
|
| [12] |
敖小凤.中性粒细胞与淋巴细胞绝对值比值和糖尿病肾病合并肾功能损伤的相关性研究[J]. 中国慢性病预防与控制,2017,25(9):708-711. DOI:10.16386/j.cjpccd.issn.1004-6194.2017.09.020.
|
| [13] |
浮苗,施林军,方莉萍,等. 单核/淋巴细胞比率与绝经后骨质疏松症的相关性研究[J]. 浙江医学,2020,42(21):2292-2295. DOI:10.12056/j.issn.1006-2785.2020.42.21.2020-261.
|
| [14] |
|
| [15] |
杜丹,付佳,杨曦,等. 老年女性NLR、PLR与BMD相关性分析[J]. 西南国防医药,2020,30(5):450-453.
|
| [16] |
|
| [17] |
|
| [18] |
吕丽,姜璐,陈诗鸿,等. 210例绝经后2型糖尿病发生骨质疏松的相关因素[J]. 山东大学学报:医学版,2021,59(7):19-25,31. DOI:10.6040/j.issn.1671-7554.0.2021.0633.
|
| [19] |
郭华平,郁嫣嫣,陈文华,等. 绝经后骨质疏松症发病相关危险因素分析及预防措施探讨[J]. 中国康复医学杂志,2011,26(5):424-428. DOI:10.3969/j.issn.1001-1242.2011.05.007.
|
| [20] |
修双玲,穆志静,孙丽娜,等. 老年2型糖尿病代谢综合征患者骨质疏松危险因素研究[J]. 首都医科大学学报,2020,41(1):108-112. DOI:10.3969/j.issn.1006-7795.2020.01.021.
|
| [21] |
包少瑜,孙兢,张智海. 绝经女性骨质疏松和代谢综合征各组分之间的相关性研究[J]. 中国骨质疏松杂志,2021,27(4):576-579. DOI:10.3969/j.issn.1006-7108.2021.04.019.
|
| [22] |
|
| [23] |
孙建然,祝捷,赵兵,等. 2型糖尿病患者晚期糖基化终末代谢产物与骨代谢的相关性[J]. 中国骨质疏松杂志,2021,27(5):635-640. DOI:10.3969/j.issn.1006-7108.2021.05.003.
|
| [1] | 张可兴, 张博, 吴琼, 朱珊珊, 王迪, 张春男. 基于代谢组学四妙勇安汤治疗糖尿病足的作用机制研究[J]. 中国全科医学, 2025, 28(30): 3796-3805. |
| [2] | 卢冬磊, 杨风英, 冯展鹏, 曹立全, 谭思洁. 同期训练可改善伴有超重或肥胖2型糖尿病患者的健康效应:一项Meta分析[J]. 中国全科医学, 2025, 28(27): 3410-3421. |
| [3] | 张睿敏, 董哲毅, 李爽, 王倩, 陈香美. 基于肾活检病理诊断的糖尿病肾病中医相关因素研究[J]. 中国全科医学, 2025, 28(26): 3307-3313. |
| [4] | 张宇诺, 李瑞斌, 王玮. 血清Nesfatin-1和Ghrelin水平与糖脂代谢及2型糖尿病的关系研究[J]. 中国全科医学, 2025, 28(26): 3264-3270. |
| [5] | 唐尚锋, 黄阳珍, 郑妍惜, 潘阳阳, 熊忠宝, 卿华, 宋佳, 魏艺琳, 董衡, 王春盈, 陈蔓维, 张康康. 糖尿病基层医防融合服务规范[J]. 中国全科医学, 2025, 28(25): 3096-3103. |
| [6] | 王汝朋, 南京, 胡奕然, 杨升华, 金泽宁. 三酰甘油-葡萄糖体质量指数对2型糖尿病合并急性心肌梗死行急诊经皮冠状动脉介入治疗术后患者慢血流/无复流的预测价值研究[J]. 中国全科医学, 2025, 28(24): 2985-2992. |
| [7] | 杨晨, 陈瞳, 张利方, 张洪旭, 李鹏飞, 张雪娟. 达格列净对老年乳腺癌幸存者射血分数保留的心力衰竭合并2型糖尿病患者的预后影响研究[J]. 中国全科医学, 2025, 28(24): 3053-3058. |
| [8] | 刘月影, 王雪丽, 刘雨秋, 魏立民. 空腹C肽与糖尿病病程比值与2型糖尿病发生代谢相关脂肪性肝病的相关性研究[J]. 中国全科医学, 2025, 28(23): 2852-2860. |
| [9] | 白雪, 陈倩倩, 李婕. 慢病管理创新实践:糖肝全-专管理新模式[J]. 中国全科医学, 2025, 28(23): 2841-2845. |
| [10] | 王鹏, 仇丽霞, 许姗姗, 张洋, 张晶, 杜晓菲. 代谢相关脂肪性肝病与2型糖尿病共同管理研究进展[J]. 中国全科医学, 2025, 28(23): 2846-2851. |
| [11] | 陈琳凤, 王晨霞, 贺金鹏. 糖尿病共同照护模式下门诊规律随访和院外APP活跃度对2型糖尿病患者代谢指标的影响研究[J]. 中国全科医学, 2025, 28(22): 2762-2768. |
| [12] | 王爽, 吴树法, 令垚, 谭茜蔚, 曹汝岱, 曾慧婷, 孔丹莉, 丁元林, 于海兵. 基于代谢组学探究非脂质代谢物在肥胖与糖尿病视网膜病变间的中介作用:孟德尔随机化研究[J]. 中国全科医学, 2025, 28(21): 2625-2634. |
| [13] | 唐笑睿, 徐晶晶, 顾子君, 王清玉, 林征, 朱秋瑞, 雷阳. 糖尿病自我护理指数量表的汉化及信效度检验[J]. 中国全科医学, 2025, 28(21): 2643-2651. |
| [14] | 王颖, 颜轶隽, 刘蕾, 胡毓敏, 张扬, 刘凯, 姜博仁. 抗阻力运动联合营养干预对老年2型糖尿病合并肌少症患者血糖稳定性影响的临床研究[J]. 中国全科医学, 2025, 28(21): 2604-2610. |
| [15] | 阿迪力·吐尔孙, 程刚. 非奈利酮治疗2型糖尿病肾病有效性和安全性的Meta分析[J]. 中国全科医学, 2025, 28(21): 2686-2691. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





