中国全科医学 ›› 2022, Vol. 25 ›› Issue (12): 1441-1448.DOI: 10.12114/j.issn.1007-9572.2021.02.137
所属专题: 安全用药最新文章合集
收稿日期:2021-11-12
修回日期:2021-12-15
出版日期:2022-03-03
发布日期:2022-03-21
通讯作者:
祝延红
基金资助:
Qian ZOU1, Miaomiao GENG2, Yanhong ZHU1,3,*( )
)
Received:2021-11-12
Revised:2021-12-15
Published:2022-03-03
Online:2022-03-21
Contact:
Yanhong ZHU
About author:摘要: 背景 既往研究证明多重耐药菌会在重症监护病房(ICU)患者之间交叉传播,患者获得多重耐药菌感染将影响其现有疾病的治疗效果;且临床上对多重耐药菌的检测速度较为缓慢。在此背景下,多重耐药菌感染预测研究应运而生。 目的 基于循证理论构建ICU患者多重耐药菌感染风险预测模型,并回顾性收集真实临床数据对模型进行验证。 方法 采用Meta分析的方法构建模型,即计算机检索PubMed、EMBase、the Cochrane Library、中国知网、万方数据知识服务平台、中文科技期刊数据库和中华医学期刊全文数据库2012年1月至2020年6月发表的有关ICU患者多重耐药菌感染的文献,提取可分析的危险因素,采用Stata/SE 12.0软件对纳入文献的数据进行Meta分析,确定ICU患者多重耐药菌感染的危险因素,并对各个危险因素的合并效应值进行β值转换构建ICU患者多重耐药菌感染风险预测模型。选取上海市第一人民医院2018年1月至2021年6月入住ICU的成年患者3 908例,收集患者的临床资料,构建预测模型,绘制预测模型预测患者多重耐药菌感染的受试者工作特征(ROC)曲线,从而进行预测模型外部验证。 结果 共纳入31篇文献,确定17个危险因素。通过换算公式得到预测模型Logit(P)=-2.476 3+0.086X1〔性别(男)〕+0.191X2(住院史)+0.392X3(从外院转入)+1.723X4(ICU住院天数)+0.315X5(其他感染)+0.385X6(慢性阻塞性肺疾病)+0.131X7(糖尿病)+0.536X8(肾脏疾病)+0.285X9(肾衰竭)+0.565X10(透析)+0.148X11(机械通气)+0.742X12(中央静脉导管)+0.336X13(导尿管)+3.483X14(抗菌药物使用种类)+0.174X15(抗菌药物使用史)+0.975X16(使用碳青霉烯类药物)+1.151X17(使用氨基糖苷类药物)。将3 908例患者数据代入预测模型中进行外部验证,结果显示,灵敏度为64.36%,特异度为80.39%,约登指数为0.447 4,ROC曲线下面积为0.724。 结论 基于循证理论构建包含17个危险因素的ICU患者多重耐药菌感染风险预测模型,该模型预判效果较好,证明基于循证理论构建风险预测模型具有较好的外推性、科学性和实用性,该方案可推广适用于其他疾病的预测研究中。
| 相关资料 | 感染组(n=303) | 未感染组(n=3 605) | |
|---|---|---|---|
| 基本情况 | |||
| 性别(男/女) | 221/82 | 2 103/1 502 | |
| 住院史〔n(%)〕 | 43(14.19) | 682(18.92) | |
| 从外院转入〔n(%)〕 | 124(40.92) | 1 105(30.65) | |
| ICU住院天数〔M(QR),d〕 | 30.5(38.5) | 12.5(12.5) | |
| 合并症 | |||
| 其他感染〔n(%)〕 | 118(38.94) | 1 037(28.77) | |
| COPD〔n(%)〕 | 13(4.29) | 87(2.41) | |
| 糖尿病〔n(%)〕 | 53(17.49) | 682(18.92) | |
| 肾脏疾病〔n(%)〕 | 67(22.11) | 489(13.56) | |
| 肾衰竭〔n(%)〕 | 15(4.95) | 74(2.05) | |
| 侵入性操作 | |||
| 透析〔n(%)〕 | 7(2.31) | 32(0.89) | |
| 机械通气〔n(%)〕 | 230(75.91) | 1 071(29.71) | |
| 中央静脉导管〔n(%)〕 | 227(74.92) | 1 433(39.75) | |
| 导尿管〔n(%)〕 | 273(90.10) | 2 693(72.93) | |
| 抗菌药物使用情况 | |||
| 抗菌药物使用种类〔M(QR),种〕 | 6(4) | 3(3) | |
| 抗菌药物使用史〔n(%)〕 | 299(98.68) | 3 188(88.43) | |
| 使用碳青霉烯类药物〔n(%)〕 | 57(18.81) | 339(9.40) | |
| 使用氨基糖苷类药物〔n(%)〕 | 46(15.18) | 117(3.25) | |
表1 感染组与未感染组相关资料
Table 1 Information of ICU patients with and without multi-drug resistant bacteria infections
| 相关资料 | 感染组(n=303) | 未感染组(n=3 605) | |
|---|---|---|---|
| 基本情况 | |||
| 性别(男/女) | 221/82 | 2 103/1 502 | |
| 住院史〔n(%)〕 | 43(14.19) | 682(18.92) | |
| 从外院转入〔n(%)〕 | 124(40.92) | 1 105(30.65) | |
| ICU住院天数〔M(QR),d〕 | 30.5(38.5) | 12.5(12.5) | |
| 合并症 | |||
| 其他感染〔n(%)〕 | 118(38.94) | 1 037(28.77) | |
| COPD〔n(%)〕 | 13(4.29) | 87(2.41) | |
| 糖尿病〔n(%)〕 | 53(17.49) | 682(18.92) | |
| 肾脏疾病〔n(%)〕 | 67(22.11) | 489(13.56) | |
| 肾衰竭〔n(%)〕 | 15(4.95) | 74(2.05) | |
| 侵入性操作 | |||
| 透析〔n(%)〕 | 7(2.31) | 32(0.89) | |
| 机械通气〔n(%)〕 | 230(75.91) | 1 071(29.71) | |
| 中央静脉导管〔n(%)〕 | 227(74.92) | 1 433(39.75) | |
| 导尿管〔n(%)〕 | 273(90.10) | 2 693(72.93) | |
| 抗菌药物使用情况 | |||
| 抗菌药物使用种类〔M(QR),种〕 | 6(4) | 3(3) | |
| 抗菌药物使用史〔n(%)〕 | 299(98.68) | 3 188(88.43) | |
| 使用碳青霉烯类药物〔n(%)〕 | 57(18.81) | 339(9.40) | |
| 使用氨基糖苷类药物〔n(%)〕 | 46(15.18) | 117(3.25) | |
| 第一作者 | 发表时间(年) | 研究类型 | 病例数/总例数 | 质量评价 |
|---|---|---|---|---|
| KIM[ | 2012 | 病例对照研究 | 106/311 | 8分 |
| BATISTÃO[ | 2012 | 病例对照研究 | 21/164 | 8分 |
| OLIVGERIS[ | 2012 | 病例对照研究 | 52/405 | 7分 |
| ROUTSI[ | 2013 | 病例对照研究 | 83/733 | 7分 |
| VASUDEVAN[ | 2014 | 队列研究 | 76/1 474 | 5分 |
| KOFTERIDIS[ | 2014 | 病例对照研究 | 83/244 | 6分 |
| MARCHENAY[ | 2015 | 队列研究 | 23/347 | 5分 |
| MCMASTER[ | 2015 | 队列研究 | 58/232 | 5分 |
| KAO[ | 2015 | 队列研究 | 237/1 266 | 6分 |
| 叶慧芬[ | 2015 | 病例对照研究 | 90/180 | 7分 |
| YANG[ | 2016 | 病例对照研究 | 370/1 110 | 7分 |
| HETEM[ | 2016 | 临床试验 | 223/8 196 | 低偏倚 |
| AMBERPET[ | 2016 | 队列研究 | 83/302 | 6分 |
| REPESSÉ[ | 2017 | 队列研究 | 9/221 | 7分 |
| MASSE[ | 2017 | 队列研究 | 204/593 | 5分 |
| 周芳[ | 2017 | 病例对照研究 | 106/246 | 8分 |
| BLANCO[ | 2018 | 队列研究 | 261/4 818 | 5分 |
| SONG[ | 2018 | 队列研究 | 89/444 | 5分 |
| 白攀峰[ | 2018 | 病例对照研究 | 264/593 | 7分 |
| 王莉[ | 2018 | 病例对照研究 | 40/80 | 6分 |
| 吴庆英[ | 2018 | 病例对照研究 | 23/100 | 6分 |
| 姚林伶[ | 2018 | 病例对照研究 | 72/144 | 5分 |
| KIDDEE[ | 2019 | 队列研究 | 134/215 | 7分 |
| VANDRESEN[ | 2019 | 病例对照研究 | 86/785 | 7分 |
| RUIZ[ | 2019 | 队列研究 | 308/1 725 | 5分 |
| KANG[ | 2019 | 病例对照研究 | 21/810 | 7分 |
| DANTAS[ | 2019 | 病例对照研究 | 343/1 372 | 6分 |
| COPPRY[ | 2019 | 病例对照研究 | 59/201 | 7分 |
| SALOMÃO[ | 2020 | 病例对照研究 | 103/304 | 6分 |
| 丁梦媛[ | 2020 | 病例对照研究 | 58/116 | 6分 |
| 陈娟婷[ | 2020 | 病例对照研究 | 89/725 | 6分 |
表2 纳入文献的基本特征及质量评价得分
Table 2 Basic characteristics and quality of included studies regarding multi-drug resistant bacterial infections in ICU patients
| 第一作者 | 发表时间(年) | 研究类型 | 病例数/总例数 | 质量评价 |
|---|---|---|---|---|
| KIM[ | 2012 | 病例对照研究 | 106/311 | 8分 |
| BATISTÃO[ | 2012 | 病例对照研究 | 21/164 | 8分 |
| OLIVGERIS[ | 2012 | 病例对照研究 | 52/405 | 7分 |
| ROUTSI[ | 2013 | 病例对照研究 | 83/733 | 7分 |
| VASUDEVAN[ | 2014 | 队列研究 | 76/1 474 | 5分 |
| KOFTERIDIS[ | 2014 | 病例对照研究 | 83/244 | 6分 |
| MARCHENAY[ | 2015 | 队列研究 | 23/347 | 5分 |
| MCMASTER[ | 2015 | 队列研究 | 58/232 | 5分 |
| KAO[ | 2015 | 队列研究 | 237/1 266 | 6分 |
| 叶慧芬[ | 2015 | 病例对照研究 | 90/180 | 7分 |
| YANG[ | 2016 | 病例对照研究 | 370/1 110 | 7分 |
| HETEM[ | 2016 | 临床试验 | 223/8 196 | 低偏倚 |
| AMBERPET[ | 2016 | 队列研究 | 83/302 | 6分 |
| REPESSÉ[ | 2017 | 队列研究 | 9/221 | 7分 |
| MASSE[ | 2017 | 队列研究 | 204/593 | 5分 |
| 周芳[ | 2017 | 病例对照研究 | 106/246 | 8分 |
| BLANCO[ | 2018 | 队列研究 | 261/4 818 | 5分 |
| SONG[ | 2018 | 队列研究 | 89/444 | 5分 |
| 白攀峰[ | 2018 | 病例对照研究 | 264/593 | 7分 |
| 王莉[ | 2018 | 病例对照研究 | 40/80 | 6分 |
| 吴庆英[ | 2018 | 病例对照研究 | 23/100 | 6分 |
| 姚林伶[ | 2018 | 病例对照研究 | 72/144 | 5分 |
| KIDDEE[ | 2019 | 队列研究 | 134/215 | 7分 |
| VANDRESEN[ | 2019 | 病例对照研究 | 86/785 | 7分 |
| RUIZ[ | 2019 | 队列研究 | 308/1 725 | 5分 |
| KANG[ | 2019 | 病例对照研究 | 21/810 | 7分 |
| DANTAS[ | 2019 | 病例对照研究 | 343/1 372 | 6分 |
| COPPRY[ | 2019 | 病例对照研究 | 59/201 | 7分 |
| SALOMÃO[ | 2020 | 病例对照研究 | 103/304 | 6分 |
| 丁梦媛[ | 2020 | 病例对照研究 | 58/116 | 6分 |
| 陈娟婷[ | 2020 | 病例对照研究 | 89/725 | 6分 |
| 危险因素 | 文献数量(篇) | 异质性检验 | 效应模型 | Z值 | OR/SMD (95%CI) | P值 | ||
|---|---|---|---|---|---|---|---|---|
| I2值(%) | P值 | |||||||
| 基本情况 | ||||||||
| X1〔性别(男)〕 | 28[ | 0 | 0.717 | 固定效应模型 | 2.79 | 1.09(1.03,1.16) | 0.005 | |
| X2(住院史) | 14[ | 0 | 0.782 | 固定效应模型 | 3.66 | 1.21(1.09,1.33) | <0.001 | |
| X3(从外院转入) | 7[ | 36.6 | 0.149 | 固定效应模型 | 4.22 | 1.48(1.24,1.78) | <0.001 | |
| X4(ICU住院天数) | 11[ | 94.2 | <0.001 | 随机效应模型 | 5.13 | 0.95(0.59,1.31)a | <0.001 | |
| 合并症 | ||||||||
| X5(其他感染) | 6[ | 0 | 0.677 | 固定效应模型 | 4.54 | 1.37(1.20,1.57) | <0.001 | |
| X6(COPD) | 11[ | 69.6 | <0.001 | 随机效应模型 | 2.37 | 1.47(1.07,2.01) | 0.018 | |
| X7(糖尿病) | 22[ | 0 | 0.593 | 固定效应模型 | 2.34 | 1.14(1.02,1.27) | 0.019 | |
| X8(肾脏疾病) | 8[ | 59.1 | 0.017 | 随机效应模型 | 1.98 | 1.71(1.00,2.91) | 0.048 | |
| X9(肾衰竭) | 6[ | 0.2 | 0.415 | 固定效应模型 | 2.45 | 1.33(1.06,1.68) | 0.014 | |
| 侵入性操作 | ||||||||
| X10(透析) | 5[ | 0 | 0.571 | 固定效应模型 | 3.40 | 1.76(1.27,2.44) | 0.001 | |
| X11(机械通气) | 11[ | 0 | 0.566 | 固定效应模型 | 2.41 | 1.16(1.03,1.32) | 0.016 | |
| X12(中央静脉导管) | 10[ | 92.2 | <0.001 | 随机效应模型 | 3.82 | 2.10(1.43,3.06) | <0.001 | |
| X13(导尿管) | 14[ | 77.9 | <0.001 | 随机效应模型 | 3.43 | 1.40(1.15,1.69) | <0.001 | |
| 抗菌药物使用情况 | ||||||||
| X14(抗菌药物使用种类) | 7[ | 98.0 | <0.001 | 随机效应模型 | 4.08 | 1.92(1.00,2.84)a | <0.001 | |
| X15(抗菌药物使用史) | 7[ | 23.7 | 0.248 | 固定效应模型 | 2.38 | 1.19(1.03,1.37) | 0.017 | |
| X16(使用碳青霉烯类药物) | 13[ | 79.6 | <0.001 | 随机效应模型 | 5.04 | 2.65(1.81,3.87) | <0.001 | |
| X17(使用氨基糖苷类药物) | 5[ | 83.9 | <0.001 | 随机效应模型 | 2.59 | 3.16(1.32,7.57) | <0.001 | |
表3 ICU患者多重耐药菌感染危险因素的Meta分析结果
Table 3 Meta-analysis of risk factors of multi-drug resistant bacterial infections in ICU patients
| 危险因素 | 文献数量(篇) | 异质性检验 | 效应模型 | Z值 | OR/SMD (95%CI) | P值 | ||
|---|---|---|---|---|---|---|---|---|
| I2值(%) | P值 | |||||||
| 基本情况 | ||||||||
| X1〔性别(男)〕 | 28[ | 0 | 0.717 | 固定效应模型 | 2.79 | 1.09(1.03,1.16) | 0.005 | |
| X2(住院史) | 14[ | 0 | 0.782 | 固定效应模型 | 3.66 | 1.21(1.09,1.33) | <0.001 | |
| X3(从外院转入) | 7[ | 36.6 | 0.149 | 固定效应模型 | 4.22 | 1.48(1.24,1.78) | <0.001 | |
| X4(ICU住院天数) | 11[ | 94.2 | <0.001 | 随机效应模型 | 5.13 | 0.95(0.59,1.31)a | <0.001 | |
| 合并症 | ||||||||
| X5(其他感染) | 6[ | 0 | 0.677 | 固定效应模型 | 4.54 | 1.37(1.20,1.57) | <0.001 | |
| X6(COPD) | 11[ | 69.6 | <0.001 | 随机效应模型 | 2.37 | 1.47(1.07,2.01) | 0.018 | |
| X7(糖尿病) | 22[ | 0 | 0.593 | 固定效应模型 | 2.34 | 1.14(1.02,1.27) | 0.019 | |
| X8(肾脏疾病) | 8[ | 59.1 | 0.017 | 随机效应模型 | 1.98 | 1.71(1.00,2.91) | 0.048 | |
| X9(肾衰竭) | 6[ | 0.2 | 0.415 | 固定效应模型 | 2.45 | 1.33(1.06,1.68) | 0.014 | |
| 侵入性操作 | ||||||||
| X10(透析) | 5[ | 0 | 0.571 | 固定效应模型 | 3.40 | 1.76(1.27,2.44) | 0.001 | |
| X11(机械通气) | 11[ | 0 | 0.566 | 固定效应模型 | 2.41 | 1.16(1.03,1.32) | 0.016 | |
| X12(中央静脉导管) | 10[ | 92.2 | <0.001 | 随机效应模型 | 3.82 | 2.10(1.43,3.06) | <0.001 | |
| X13(导尿管) | 14[ | 77.9 | <0.001 | 随机效应模型 | 3.43 | 1.40(1.15,1.69) | <0.001 | |
| 抗菌药物使用情况 | ||||||||
| X14(抗菌药物使用种类) | 7[ | 98.0 | <0.001 | 随机效应模型 | 4.08 | 1.92(1.00,2.84)a | <0.001 | |
| X15(抗菌药物使用史) | 7[ | 23.7 | 0.248 | 固定效应模型 | 2.38 | 1.19(1.03,1.37) | 0.017 | |
| X16(使用碳青霉烯类药物) | 13[ | 79.6 | <0.001 | 随机效应模型 | 5.04 | 2.65(1.81,3.87) | <0.001 | |
| X17(使用氨基糖苷类药物) | 5[ | 83.9 | <0.001 | 随机效应模型 | 2.59 | 3.16(1.32,7.57) | <0.001 | |
| 危险因素 | Begg's检验 | Egger's检验 |
|---|---|---|
| 性别(男) | 0.752 | 0.141 |
| 住院史 | 0.702 | 0.868 |
| ICU住院天数 | 0.312 | 0.998 |
| COPD | 0.891 | 0.349 |
| 糖尿病 | 0.382 | 0.321 |
| 机械通气 | 0.586 | 0.636 |
| 中央静脉导管 | 0.531 | 0.772 |
| 导尿管 | 0.956 | 0.237 |
| 使用碳青霉烯类药物 | 0.714 | 0.961 |
表4 ICU患者多重耐药菌感染危险因素文献发表偏倚的分析结果
Table 4 Publication bias assessment of studies regarding risk factors of multi-drug resistant bacterial infections in ICU patients
| 危险因素 | Begg's检验 | Egger's检验 |
|---|---|---|
| 性别(男) | 0.752 | 0.141 |
| 住院史 | 0.702 | 0.868 |
| ICU住院天数 | 0.312 | 0.998 |
| COPD | 0.891 | 0.349 |
| 糖尿病 | 0.382 | 0.321 |
| 机械通气 | 0.586 | 0.636 |
| 中央静脉导管 | 0.531 | 0.772 |
| 导尿管 | 0.956 | 0.237 |
| 使用碳青霉烯类药物 | 0.714 | 0.961 |
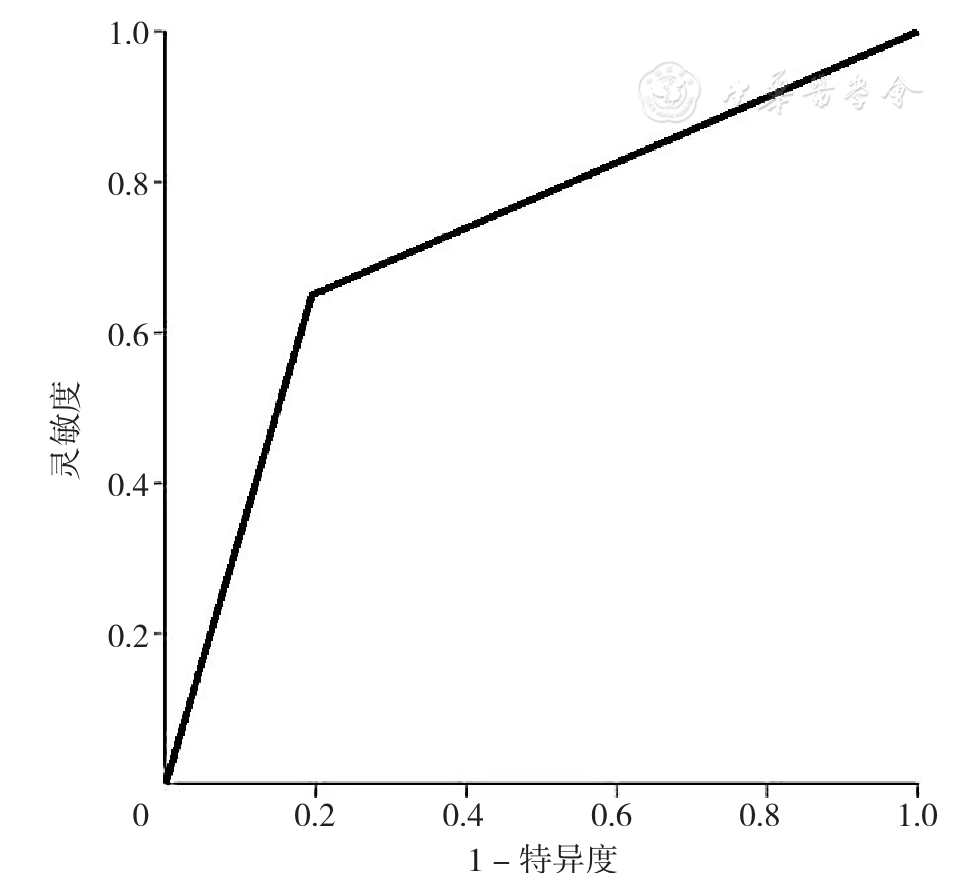
图2 ICU患者多重耐药菌感染风险预测模型预测效果的ROC曲线
Figure 2 ROC analysis of the prediction model for estimating the risk of multi-drug resistant bacterial infections in ICU patients
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
卫生部办公厅关于印发《多重耐药菌医院感染预防与控制技术指南(试行)》的通知[J]. 中华人民共和国国家卫生与计划生育委员会公报,2011,9(2):59-61.
|
| [9] |
李洋,何文英,王忠. 基于Meta分析腹腔镜胆囊切除术中转开腹风险预测模型的构建[J]. 中国全科医学,2018,21(23):2849-2855. DOI:10.3969/j.issn.1007-9572.2018.00.127.
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [21] |
|
| [22] |
|
| [23] |
|
| [24] |
|
| [25] |
|
| [26] |
|
| [27] |
|
| [28] |
|
| [29] |
|
| [30] |
|
| [31] |
|
| [32] |
|
| [33] |
白攀峰,胡尚琼,吴晓英,等. ICU患者多重耐药菌定植或感染的危险因素分析[J]. 世界最新医学信息文摘,2018,18(9):4-5,8. DOI:10.19613/j.cnki.1671-3141.2018.09.002.
|
| [34] |
陈娟婷,陈法聪. 某院重症监护病房患者多重耐药菌感染的危险因素分析及预防对策[J]. 抗感染药学,2020,17(3):376-378. DOI:10.13493/j.issn.1672-7878.2020.03-022.
|
| [35] |
丁梦媛,李文进,耿苗苗,等. 综合重症监护病房患者多重耐药菌医院感染风险评估模型构建[J]. 中国卫生资源,2020,23(4):384-387,399. DOI:10.13688/j.cnki.chr.2020.20326.
|
| [36] |
王莉,张桂侠,卢晓娥. 某院重症医学科患者多重耐药鲍曼不动杆菌医院感染危险因素分析[J]. 中国消毒学杂志,2018,35(6):478-480. DOI:10.11726/j.issn.1001-7658.2018.06.027.
|
| [37] |
吴庆英,马自东. ICU病房多重耐药菌感染相关危险因素及预防控制管理[J]. 兵团医学,2018(2):14-16. DOI:10.3969/j.issn.1672-4356.2018.02.007.
|
| [38] |
姚林伶,罗朝军,冯广贵. 鲍曼不动杆菌院内感染的危险因素和耐药性分析[J]. 中国实用医药,2018,13(22):192-194. DOI:10.14163/j.cnki.11-5547/r.2018.22.111.
|
| [39] |
叶慧芬,曾俊韶,覃文周,等. 重症监护病房患者MRSA定植情况及影响因素研究[J]. 中国消毒学杂志,2015,32(1):24-26.
|
| [40] |
周芳,董亚琳. ICU多重耐药菌医院感染的危险因素分析[J]. 中国药房,2017,28(14):1916-1920. DOI:10.6039/j.issn.1001-0408.2017.14.12.
|
| [41] |
温剑艺,覃铁和,王首红,等. ICU老年患者多重耐药菌主动筛查情况及危险因素分析[J]. 中国药房,2018,29(2):199-203. DOI:10.6039/j.issn.1001-0408.2018.02.14.
|
| [42] |
杨晋如,谈宜斌,邬闻文,等. 重症医学科不同置管患者多重耐药菌感染的生存分析[J]. 中国感染与化疗杂志,2021,21(3):297-302. DOI:10.16718/j.1009-7708.2021.03.010.
|
| [43] |
李巍,史哲新,王兴丽,等. 替加环素对血液病患者化疗后多重耐药菌感染的疗效探讨[J]. 中国全科医学,2020,23(S2):168-170.
|
| [44] |
王敏芳,干铁儿,丁黎敏,等. 多重耐药菌感染综合防控措施的闭环管理及其效果评价[J]. 中华医院感染学杂志,2021,31(18):2850-2854. DOI:10.11816/cn.ni.2021-211206.
|
| [45] |
|
| [46] |
项彦斌,周燕,杜建成,等. 重症患者多重耐药菌感染的影响因素及预测模型分析[J]. 重庆医学,2020,49(23):3966-3970. DOI:10.3969/j.issn.1671-8348.2020.23.024.
|
| [1] | 王喆, 董志浩, 郑好, 孔文程, 张玉宽, 张秋月, 韩晶. 针刺干预偏头痛优势方案构建研究:基于熵权TOPSIS法[J]. 中国全科医学, 2023, 26(34): 4336-4342. |
| [2] | 王越, 陈晴, 刘鲁蓉. 中国老年人抑郁检出率及影响因素的Meta分析[J]. 中国全科医学, 2023, 26(34): 4329-4335. |
| [3] | 梁譞, 那飞扬, 秦梦瑶, 杨辉, 郭丽, 郭琪, 任蕾, 陈德, 刘东海, 张蓉芳. 儿童支气管哮喘合并阻塞性睡眠呼吸暂停低通气综合征的临床特征及影响因素研究[J]. 中国全科医学, 2023, 26(33): 4225-4230. |
| [4] | 张继方, 陈芳, 唐佳雯, 李红亮. 肿瘤出芽及肿瘤浸润淋巴细胞对食管鳞状细胞癌淋巴结转移的预测价值研究[J]. 中国全科医学, 2023, 26(32): 4038-4042. |
| [5] | 蹇秋枫, 徐荣华, 姚倩, 周媛媛. 中国老年脑卒中患者认知障碍患病率和影响因素的Meta分析[J]. 中国全科医学, 2023, 26(32): 4070-4079. |
| [6] | 贾钰, 周紫彤, 曹学华, 胡婉琴, 向凤, 熊浪宇, 王晓霞. 中国40~65岁女性围绝经期综合征发生率的Meta分析[J]. 中国全科医学, 2023, 26(32): 4080-4088. |
| [7] | 李纪新, 邱林杰, 任燕, 王文茹, 李美洁, 张晋. 膳食炎症指数与超重和肥胖及腹型肥胖关系的Meta分析[J]. 中国全科医学, 2023, 26(32): 4089-4097. |
| [8] | 张娟, 李海芬, 李小曼, 姚苗, 马惠珍, 马强. 糖尿病足溃疡复发风险预测模型的构建:基于Logistic回归和支持向量机及BP神经网络模型[J]. 中国全科医学, 2023, 26(32): 4013-4019. |
| [9] | 何静漪, 王芳, 税晓玲, 李玲, 梁倩. 非药物干预改善围绝经期失眠症状疗效的网状Meta分析[J]. 中国全科医学, 2023, 26(31): 3963-3974. |
| [10] | 朱琳, 郭闫葵, 高琛, 陈学志, 王法帅. 单纯西药、中成药及其联合治疗卒中后失眠疗效的网状Meta分析[J]. 中国全科医学, 2023, 26(30): 3823-3832. |
| [11] | 张懂理, 沈冲, 张卫川, 陈海滨, 赵建军. 程序性死亡因子1/程序性死亡因子1配体抑制剂治疗肾细胞癌有效性及安全性的Meta分析[J]. 中国全科医学, 2023, 26(30): 3815-3822. |
| [12] | 何莉, 张逸凡, 沈雪纯, 孙燕, 赵洋. 中国大陆地区居民慢性病共病的流行趋势:一项Meta分析[J]. 中国全科医学, 2023, 26(29): 3599-3607. |
| [13] | 王珍, 申国旗, 李亚南, 朱英华, 仇航, 郑迪, 徐通达, 李文华. 急性心肌梗死患者行经皮冠状动脉介入治疗术后发生对比剂急性肾损伤风险预测模型的建立与验证研究[J]. 中国全科医学, 2023, 26(29): 3650-3656. |
| [14] | 胡婧伊, 洪景, 郭晓冬, 张晓红, 莫宁, 周小翠, 余钦, 周敏华, 孙艳, 倪柳, 石晓丽, 苏小青, 李玉倩. 社区参与安宁疗护对临终期肿瘤患者干预效果的Meta分析[J]. 中国全科医学, 2023, 26(28): 3573-3584. |
| [15] | 白一彤, 林连捷, 裴冬梅. 代谢相关性脂肪性肝病严重程度与甲状腺结节的相关性研究[J]. 中国全科医学, 2023, 26(27): 3392-3396. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





