中国全科医学 ›› 2023, Vol. 26 ›› Issue (32): 4031-4037.DOI: 10.12114/j.issn.1007-9572.2023.0127
所属专题: 肿瘤最新文章合辑; 骨健康最新文章合辑; 消化系统疾病最新文章合辑
收稿日期:2023-02-06
修回日期:2023-03-30
出版日期:2023-11-15
发布日期:2023-04-26
通讯作者:
曹春
基金资助:
GAO Dekang, WEI Shaohua, MA Xiaoming, DU Peng, XING Chungen, CAO Chun*( )
)
Received:2023-02-06
Revised:2023-03-30
Published:2023-11-15
Online:2023-04-26
Contact:
CAO Chun
摘要: 背景 肝癌大范围肝切除术手术风险高,围术期营养状况对术后恢复极为重要,然而目前鲜有术后骨骼肌减少(PLSMM)预测术后并发症及预后的研究。 目的 明确肝癌大范围肝切除术后患者骨骼肌指数(SMI)变化,并探讨术后PLSMM发生的危险因素以及其与术后并发症的相关性。 方法 选取2018年7月—2022年8月因肝癌在苏州大学附属第二医院普外科接受大范围肝切除术的患者97例,通过CT影像测量术前和术后第5天第三腰椎水平的骨骼肌面积。计算术后SMI变化率,PLSMM定义为SMI变化率的最低三分位数,并以此将患者分为PLSMM组和Non-PLSMM组。收集两组患者基线资料、手术相关指标及术后指标等并进行对比分析。 结果 共54例患者术后出现SMI降低;PLSMM组32例(SMI≤-3.59%),Non-PLSMM组65例(SMI>-3.59%)。PLSMM组手术时间长于Non-PLSMM组,手术失血量多于Non-PLSMM组,微血管侵犯(MVI)发生率高于Non-PLSMM组(P<0.05)。PLSMM组术后住院时间长于Non-PLSMM组,术后第5天白细胞计数(WBC)和国际标准化比值(INR)高于Non-PLSMM组,术后第5天纤维蛋白原(FIB)水平低于Non-PLSMM组,总体并发症发生率高于Non-PLSMM组(P<0.05)。多因素Logistic回归分析结果显示,MVI〔OR=2.751,95%CI(1.173,6.642)〕及手术时间>210 min〔OR=1.973,95%CI(1.286,4.936)〕是肝癌大范围肝切除术后患者发生PLSMM的危险因素(P<0.05);并且PLSMM〔OR=2.591,95%CI(1.173,6.977)〕、术前肌少症〔OR=1.798,95%CI(1.133,3.792)〕、手术时间>210 min〔OR=2.958,95%CI(0.918,9.529)〕和失血量>500 mL〔OR=1.003,95%CI(1.001,1.007)〕是肝癌大范围肝切除术后患者发生并发症的危险因素(P<0.05)。 结论 MVI和手术时间>210 min是肝癌大范围肝切除术后PLSMM发生的危险因素,同时PLSMM是术后并发症的独立预测因子,其对预后发挥负向影响作用。
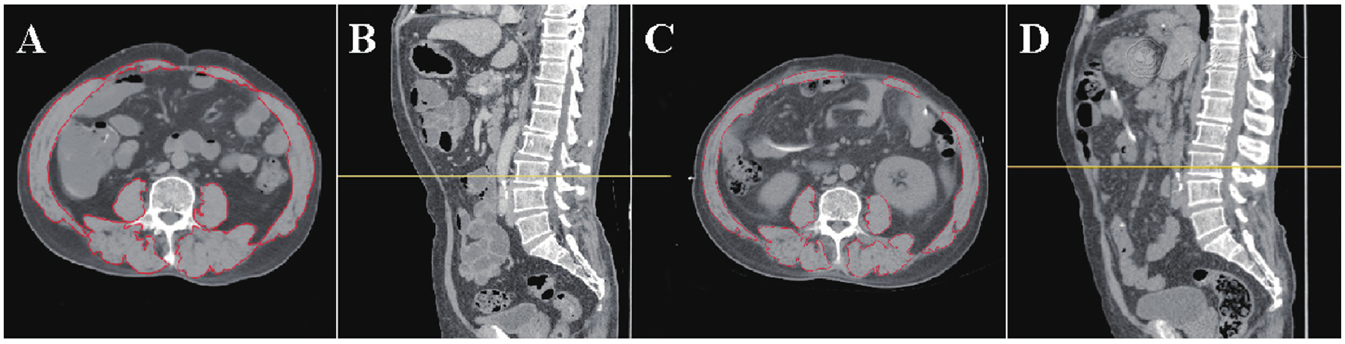
图1 CT测算第三腰椎水平骨骼肌面积注:A、C为水平位,B、D为矢状位;黄色水平线为设定的第三腰椎水平,红色线条区域内为此水平骨骼肌范围;A、B为术前骨骼肌指数(SMI)(47.98 cm2/m2),C、D为术后SMI(43.10 cm2/m2)。
Figure 1 Skeletal muscle area at the third lumbar vertebra measured with computed tomographic images
| 指标 | Non-PLSMM组(n=65) | PLSMM组(n=32) | Z(χ2)值 | P值 |
|---|---|---|---|---|
| 性别(男/女) | 34/31 | 14/18 | 0.628a | 0.428 |
| 年龄〔M(P25,P75),岁〕 | 60(52,70) | 59(50,69) | -0.303 | 0.765 |
| 体质量〔M(P25,P75),kg〕 | 60(53,70) | 58(51,63) | -1.570 | 0.117 |
| BMI〔M(P25,P75),kg/m2〕 | 22.3(20.9,24.9) | 21.7(20.2,24.2) | -1.051 | 0.295 |
| 病理诊断〔例(%)〕 | 0.056a | 0.813 | ||
| 肝细胞型肝癌 | 39(60) | 20(63) | ||
| 肝胆管细胞型肝癌 | 26(40) | 12(37) | ||
| 术前肌少症〔例(%)〕 | 34(52) | 20(63) | 0.903a | 0.342 |
| 病毒性肝炎〔例(%)〕 | 18(48) | 9(37) | 0.002a | 0.964 |
| Child-Pugh分级〔例(%)〕 | 0.252a | 0.616 | ||
| A级 | 59(91) | 30(94) | ||
| B级 | 6(9) | 2(6) | ||
| 肝硬化〔例(%)〕 | 18(28) | 10(31) | 0.132a | 0.716 |
| ICG-R15〔M(P25,P75)〕 | 9.1(6.4,11.9) | 8.0(6.7,11.3) | -0.491 | 0.626 |
| 剩余肝体积〔M(P25,P75),%〕 | 48.3(43.8,56.5) | 48.4(45.7,53.1) | -0.077 | 0.942 |
| 术前实验室检查指标 | ||||
| WBC〔M(P25,P75),×109/L〕 | 7(5.50,8.60) | 6.75(4.78,8.35) | -0.173 | 0.866 |
| HB〔M(P25,P75),g/L〕 | 118.7(105.6,130.7) | 123.4(112.2,132.4) | -0.675 | 0.502 |
| PLT〔M(P25,P75),×109/L〕 | 261.0(214.0,314.0) | 241.5(207.0,289.5) | -1.255 | 0.211 |
| NEU〔M(P25,P75),×109/L〕 | 4.20(3.10,5.10) | 3.75(3.08,4.35) | -1.013 | 0.313 |
| LYM〔M(P25,P75),×109/L〕 | 1.90(1.40,2.65) | 2.15(1.65,2.46) | -0.488 | 0.629 |
| NEU/LYM〔M(P25,P75)〕 | 2.24(1.51,2.96) | 1.81(1.43,2.29) | -1.393 | 0.165 |
| AST〔M(P25,P75),U/L〕 | 57.0(36.0,75.0) | 65.5(41.8,83.0) | -1.201 | 0.231 |
| ALT〔M(P25,P75),U/L〕 | 59(47,71) | 61(47,78) | -0.660 | 0.512 |
| LDH〔M(P25,P75),U/L〕 | 283(186,336) | 260(169,350) | <0.001 | 0.997 |
| TBIL〔M(P25,P75),μmol/L〕 | 27.1(17.3,33.8) | 29.1(23.0,36.3) | -0.913 | 0.363 |
| DBIL〔M(P25,P75),μmol/L〕 | 6.45(4.35,8.35) | 5.35(4.11,7.07) | -1.209 | 0.228 |
| ALB〔M(P25,P75),g/L〕 | 37.3(33.4,43.8) | 37.4(32.2,42.5) | -0.679 | 0.499 |
| GLB〔M(P25,P75),g/L〕 | 31.9(27.0,36.4) | 29.8(25.1,33.1) | -0.967 | 0.336 |
| ALB/GLB〔M(P25,P75)〕 | 1.25(1.01,1.46) | 1.25(1.12,1.35) | -0.192 | 0.851 |
| INR〔M(P25,P75)〕 | 1.1(0.99,1.24) | 1.09(0.95,1.22) | -0.215 | 0.833 |
| PT〔M(P25,P75),s〕 | 12.7(12.0,13.7) | 13.0(11.9,14.2) | -0.564 | 0.575 |
| APTT〔M(P25,P75),s〕 | 32.6(31.4,34.2) | 33.5(31.9,34.5) | -1.094 | 0.276 |
| FIB〔M(P25,P75),g/L〕 | 3.54(2.98,3.91) | 3.64(2.98,4.29) | -0.856 | 0.394 |
表1 Non-PLSMM组与PLSMM组术前基线资料比较
Table 1 Comparisonof preoperative characteristics between non-PLSMM and PLSMM groups
| 指标 | Non-PLSMM组(n=65) | PLSMM组(n=32) | Z(χ2)值 | P值 |
|---|---|---|---|---|
| 性别(男/女) | 34/31 | 14/18 | 0.628a | 0.428 |
| 年龄〔M(P25,P75),岁〕 | 60(52,70) | 59(50,69) | -0.303 | 0.765 |
| 体质量〔M(P25,P75),kg〕 | 60(53,70) | 58(51,63) | -1.570 | 0.117 |
| BMI〔M(P25,P75),kg/m2〕 | 22.3(20.9,24.9) | 21.7(20.2,24.2) | -1.051 | 0.295 |
| 病理诊断〔例(%)〕 | 0.056a | 0.813 | ||
| 肝细胞型肝癌 | 39(60) | 20(63) | ||
| 肝胆管细胞型肝癌 | 26(40) | 12(37) | ||
| 术前肌少症〔例(%)〕 | 34(52) | 20(63) | 0.903a | 0.342 |
| 病毒性肝炎〔例(%)〕 | 18(48) | 9(37) | 0.002a | 0.964 |
| Child-Pugh分级〔例(%)〕 | 0.252a | 0.616 | ||
| A级 | 59(91) | 30(94) | ||
| B级 | 6(9) | 2(6) | ||
| 肝硬化〔例(%)〕 | 18(28) | 10(31) | 0.132a | 0.716 |
| ICG-R15〔M(P25,P75)〕 | 9.1(6.4,11.9) | 8.0(6.7,11.3) | -0.491 | 0.626 |
| 剩余肝体积〔M(P25,P75),%〕 | 48.3(43.8,56.5) | 48.4(45.7,53.1) | -0.077 | 0.942 |
| 术前实验室检查指标 | ||||
| WBC〔M(P25,P75),×109/L〕 | 7(5.50,8.60) | 6.75(4.78,8.35) | -0.173 | 0.866 |
| HB〔M(P25,P75),g/L〕 | 118.7(105.6,130.7) | 123.4(112.2,132.4) | -0.675 | 0.502 |
| PLT〔M(P25,P75),×109/L〕 | 261.0(214.0,314.0) | 241.5(207.0,289.5) | -1.255 | 0.211 |
| NEU〔M(P25,P75),×109/L〕 | 4.20(3.10,5.10) | 3.75(3.08,4.35) | -1.013 | 0.313 |
| LYM〔M(P25,P75),×109/L〕 | 1.90(1.40,2.65) | 2.15(1.65,2.46) | -0.488 | 0.629 |
| NEU/LYM〔M(P25,P75)〕 | 2.24(1.51,2.96) | 1.81(1.43,2.29) | -1.393 | 0.165 |
| AST〔M(P25,P75),U/L〕 | 57.0(36.0,75.0) | 65.5(41.8,83.0) | -1.201 | 0.231 |
| ALT〔M(P25,P75),U/L〕 | 59(47,71) | 61(47,78) | -0.660 | 0.512 |
| LDH〔M(P25,P75),U/L〕 | 283(186,336) | 260(169,350) | <0.001 | 0.997 |
| TBIL〔M(P25,P75),μmol/L〕 | 27.1(17.3,33.8) | 29.1(23.0,36.3) | -0.913 | 0.363 |
| DBIL〔M(P25,P75),μmol/L〕 | 6.45(4.35,8.35) | 5.35(4.11,7.07) | -1.209 | 0.228 |
| ALB〔M(P25,P75),g/L〕 | 37.3(33.4,43.8) | 37.4(32.2,42.5) | -0.679 | 0.499 |
| GLB〔M(P25,P75),g/L〕 | 31.9(27.0,36.4) | 29.8(25.1,33.1) | -0.967 | 0.336 |
| ALB/GLB〔M(P25,P75)〕 | 1.25(1.01,1.46) | 1.25(1.12,1.35) | -0.192 | 0.851 |
| INR〔M(P25,P75)〕 | 1.1(0.99,1.24) | 1.09(0.95,1.22) | -0.215 | 0.833 |
| PT〔M(P25,P75),s〕 | 12.7(12.0,13.7) | 13.0(11.9,14.2) | -0.564 | 0.575 |
| APTT〔M(P25,P75),s〕 | 32.6(31.4,34.2) | 33.5(31.9,34.5) | -1.094 | 0.276 |
| FIB〔M(P25,P75),g/L〕 | 3.54(2.98,3.91) | 3.64(2.98,4.29) | -0.856 | 0.394 |
| 指标 | Non-PLSMM组(n=65) | PLSMM组(n=32) | χ2(Z)值 | P值 |
|---|---|---|---|---|
| 手术方式〔例(%)〕 | 0.672 | 0.955 | ||
| 左半肝切除术 | 23(35) | 13(41) | ||
| 右半肝切除术 | 32(49) | 14(44) | ||
| 左三叶切除术 | 6(9) | 3(9) | ||
| 左半肝+S1段切除术 | 1(2) | 1(3) | ||
| 右半肝+S1段切除术 | 3(5) | 1(3) | ||
| 手术时间〔M(P25,P75),min〕 | 180(150,220) | 212(180,290) | -2.013a | 0.047 |
| 失血量〔M(P25,P75),mL〕 | 300(200,600) | 600(200,800) | -2.297a | 0.022 |
| 输血〔例(%)〕 | 13(20) | 9(28) | 0.807 | 0.369 |
| MVI〔例(%)〕 | 12(18) | 12(38) | 4.174 | 0.041 |
表2 Non-PLSMM组与PLSMM组手术相关指标对比
Table 2 Comparisonof intraoperative characteristics between non-PLSMM and PLSMM groups
| 指标 | Non-PLSMM组(n=65) | PLSMM组(n=32) | χ2(Z)值 | P值 |
|---|---|---|---|---|
| 手术方式〔例(%)〕 | 0.672 | 0.955 | ||
| 左半肝切除术 | 23(35) | 13(41) | ||
| 右半肝切除术 | 32(49) | 14(44) | ||
| 左三叶切除术 | 6(9) | 3(9) | ||
| 左半肝+S1段切除术 | 1(2) | 1(3) | ||
| 右半肝+S1段切除术 | 3(5) | 1(3) | ||
| 手术时间〔M(P25,P75),min〕 | 180(150,220) | 212(180,290) | -2.013a | 0.047 |
| 失血量〔M(P25,P75),mL〕 | 300(200,600) | 600(200,800) | -2.297a | 0.022 |
| 输血〔例(%)〕 | 13(20) | 9(28) | 0.807 | 0.369 |
| MVI〔例(%)〕 | 12(18) | 12(38) | 4.174 | 0.041 |
| 因素 | Non-PLSMM组(n=65) | PLSMM组(n=32) | Z(χ2)值 | P值 |
|---|---|---|---|---|
| 术后住院时间〔M(P25,P75),d〕 | 11(8,13) | 13(10,16.3) | -2.297 | 0.022 |
| 术后第5天实验室检查指标 | ||||
| WBC〔M(P25,P75),×109/L〕 | 6.90(5.50,7.90) | 8.55(5.70,10.03) | -2.13 | 0.034 |
| HB〔M(P25,P75),g/L〕 | 115.5(100.5,120.8) | 107.0(96.0,121.0) | -0.649 | 0.502 |
| PLT〔M(P25,P75),×109/L〕 | 157.0(125.0,211.0) | 143.5(117.8,193.5) | -0.445 | 0.659 |
| NEU〔M(P25,P75),×109/L〕 | 5.5(3.9,6.9) | 5.6(4.1,7.4) | -0.253 | 0.803 |
| LYM〔M(P25,P75),×109/L〕 | 1.0(0.8,1.4) | 1.1(0.7,1.4) | -0.143 | 0.890 |
| NEU/LYM〔M(P25,P75)〕 | 5.60(3.75,7.86) | 5.18(3.85,6.89) | -0.065 | 0.950 |
| AST〔M(P25,P75),U/L〕 | 33(22,52) | 38(23,75) | -1.098 | 0.274 |
| ALT〔M(P25,P75),U/L〕 | 63(44,104) | 65(38,91) | -0.648 | 0.519 |
| LDH〔M(P25,P75),U/L〕 | 182(158,224) | 198(158,231) | -0.514 | 0.610 |
| TBIL〔M(P25,P75),μmol/L〕 | 23.4(12.6,33.2) | 16.0(12.7,29.3) | -1.331 | 0.184 |
| DBIL〔M(P25,P75),μmol/L〕 | 7.1(5.2,14.5) | 6.9(5.6,9.6) | -0.813 | 0.418 |
| ALB〔M(P25,P75),g/L〕 | 35.9(33.0,37.9) | 34.1(32.0,36.6) | -1.753 | 0.080 |
| GLB〔M(P25,P75),g/L〕 | 22.3(20.0,25.2) | 23.5(19.9,24.7) | -0.134 | 0.896 |
| ALB/GLB〔M(P25,P75)〕 | 1.57(1.39,1.79) | 1.55(1.36,1.67) | -0.967 | 0.340 |
| INR〔M(P25,P75)〕 | 1.18(0.98,1.46) | 1.33(1.15,1.56) | -2.068 | 0.039 |
| PT〔M(P25,P75),s〕 | 14.1(13.3,14.6) | 14.1(13.6,14.8) | -0.115 | 0.911 |
| APTT〔M(P25,P75),s〕 | 35.3(32.5,38.6) | 35.4(32.9,37.2) | -0.150 | 0.884 |
| FIB〔M(P25,P75),g/L〕 | 3.49(2.62,4.67) | 2.55(2.11,3.58) | -2.425 | 0.016 |
| 总体并发症〔例(%)〕 | 25(38) | 21(66) | 6.346a | 0.012 |
| 器官/腔隙SSI | 12(18) | 15(47) | 8.618a | 0.003 |
| 切口SSI | 2(3) | 7(22) | 9.002a | 0.003 |
| 菌血症 | 8(12) | 10(31) | 5.091a | 0.024 |
| 胆瘘(ISGLS B级) | 8(12) | 10(31) | 5.091a | 0.024 |
| 术后出血 | 3(5) | 5(16) | 3.435a | 0.064 |
| 肝衰竭(ISGLS B级) | 3(5) | 6(19) | 5.090a | 0.024 |
| 迟发性胃轻瘫 | 3(5) | 3(9) | 0.837a | 0.360 |
| 心肺事件 | 2(3) | 2(6) | 0.546a | 0.460 |
| 血栓形成事件 | 0 | 2(6) | 4.148a | 0.042 |
| 单器官衰竭 | 0 | 4(13) | 8.474a | 0.004 |
| 死亡 | 1(2) | 4(13) | 5.270a | 0.022 |
表3 Non-PLSMM组与PLSMM组术后指标及并发症发生率比较
Table 3 Comparison of postoperative characteristics and complications between non-PLSMM and PLSMM groups
| 因素 | Non-PLSMM组(n=65) | PLSMM组(n=32) | Z(χ2)值 | P值 |
|---|---|---|---|---|
| 术后住院时间〔M(P25,P75),d〕 | 11(8,13) | 13(10,16.3) | -2.297 | 0.022 |
| 术后第5天实验室检查指标 | ||||
| WBC〔M(P25,P75),×109/L〕 | 6.90(5.50,7.90) | 8.55(5.70,10.03) | -2.13 | 0.034 |
| HB〔M(P25,P75),g/L〕 | 115.5(100.5,120.8) | 107.0(96.0,121.0) | -0.649 | 0.502 |
| PLT〔M(P25,P75),×109/L〕 | 157.0(125.0,211.0) | 143.5(117.8,193.5) | -0.445 | 0.659 |
| NEU〔M(P25,P75),×109/L〕 | 5.5(3.9,6.9) | 5.6(4.1,7.4) | -0.253 | 0.803 |
| LYM〔M(P25,P75),×109/L〕 | 1.0(0.8,1.4) | 1.1(0.7,1.4) | -0.143 | 0.890 |
| NEU/LYM〔M(P25,P75)〕 | 5.60(3.75,7.86) | 5.18(3.85,6.89) | -0.065 | 0.950 |
| AST〔M(P25,P75),U/L〕 | 33(22,52) | 38(23,75) | -1.098 | 0.274 |
| ALT〔M(P25,P75),U/L〕 | 63(44,104) | 65(38,91) | -0.648 | 0.519 |
| LDH〔M(P25,P75),U/L〕 | 182(158,224) | 198(158,231) | -0.514 | 0.610 |
| TBIL〔M(P25,P75),μmol/L〕 | 23.4(12.6,33.2) | 16.0(12.7,29.3) | -1.331 | 0.184 |
| DBIL〔M(P25,P75),μmol/L〕 | 7.1(5.2,14.5) | 6.9(5.6,9.6) | -0.813 | 0.418 |
| ALB〔M(P25,P75),g/L〕 | 35.9(33.0,37.9) | 34.1(32.0,36.6) | -1.753 | 0.080 |
| GLB〔M(P25,P75),g/L〕 | 22.3(20.0,25.2) | 23.5(19.9,24.7) | -0.134 | 0.896 |
| ALB/GLB〔M(P25,P75)〕 | 1.57(1.39,1.79) | 1.55(1.36,1.67) | -0.967 | 0.340 |
| INR〔M(P25,P75)〕 | 1.18(0.98,1.46) | 1.33(1.15,1.56) | -2.068 | 0.039 |
| PT〔M(P25,P75),s〕 | 14.1(13.3,14.6) | 14.1(13.6,14.8) | -0.115 | 0.911 |
| APTT〔M(P25,P75),s〕 | 35.3(32.5,38.6) | 35.4(32.9,37.2) | -0.150 | 0.884 |
| FIB〔M(P25,P75),g/L〕 | 3.49(2.62,4.67) | 2.55(2.11,3.58) | -2.425 | 0.016 |
| 总体并发症〔例(%)〕 | 25(38) | 21(66) | 6.346a | 0.012 |
| 器官/腔隙SSI | 12(18) | 15(47) | 8.618a | 0.003 |
| 切口SSI | 2(3) | 7(22) | 9.002a | 0.003 |
| 菌血症 | 8(12) | 10(31) | 5.091a | 0.024 |
| 胆瘘(ISGLS B级) | 8(12) | 10(31) | 5.091a | 0.024 |
| 术后出血 | 3(5) | 5(16) | 3.435a | 0.064 |
| 肝衰竭(ISGLS B级) | 3(5) | 6(19) | 5.090a | 0.024 |
| 迟发性胃轻瘫 | 3(5) | 3(9) | 0.837a | 0.360 |
| 心肺事件 | 2(3) | 2(6) | 0.546a | 0.460 |
| 血栓形成事件 | 0 | 2(6) | 4.148a | 0.042 |
| 单器官衰竭 | 0 | 4(13) | 8.474a | 0.004 |
| 死亡 | 1(2) | 4(13) | 5.270a | 0.022 |
| 自变量 | 单因素分析 | 多因素分析 | ||
|---|---|---|---|---|
| OR(95%CI) | P值 | OR(95%CI) | P值 | |
| 性别(以男为参照) | ||||
| 女 | 1.410(0.602,3.304) | 0.429 | ||
| BMI(以≥18.0 kg/m2为参照) | ||||
| <18.0 kg/m2 | 0.928(0.805,1.069) | 0.328 | ||
| 术前肌少症(以无为参照) | ||||
| 有 | 1.520(0.640,3.611) | 0.342 | ||
| 病毒性肝炎(以无为参照) | ||||
| 有 | 1.022(0.398,2.623) | 0.964 | ||
| 肝硬化(以无为参照) | ||||
| 有 | 1.187(0.471,2.990) | 0.716 | ||
| ICG-R15(以≤10为参照) | ||||
| >10 | 0.961(0.832,1.111) | 0.593 | ||
| 剩余肝体积(以≥40%为参照) | ||||
| <40% | 0.992(0.937,1.050) | 0.777 | ||
| 手术时间(以≤210 min为参照) | ||||
| >210 min | 2.803(1.127,6.973) | 0.027 | 1.973(1.286,4.936) | 0.038 |
| 失血量(以≤500 mL为参照) | ||||
| >500 mL | 1.002(1.001,1.004) | 0.005 | 1.001(1.000,1.004) | 0.152 |
| 输血(以无为参照) | ||||
| 有 | 1.565(0.587,4.176) | 0.369 | ||
| MVI(以无为参照) | ||||
| 有 | 2.65(1.024,6.860) | 0.045 | 2.751(1.173,6.642) | 0.041 |
| WBC(以≤9.00×109/L为参照) | ||||
| >9.00×109/L | 1.199(1.013,1.418) | 0.034 | 1.153(0.895,1.377) | 0.143 |
| HB(以≥100.0 g/L为参照) | ||||
| <100.0 g/L | 1.005(0.979,1.032) | 0.688 | ||
| PLT(以≥125.0×109/L为参照) | ||||
| <125.0×109/L | 0.979(0.972,1.006) | 0.750 | ||
| NEU(以≤6.0×109/L为参照) | ||||
| >6.0×109/L | 1.006(0.831,1.216) | 0.954 | ||
| LYM(以≥1.1×109/L为参照) | ||||
| <1.1×109/L | 1.005(0.301,3.352) | 0.994 | ||
| AST(以≤50 U/L为参照) | ||||
| >50 U/L | 1.000(0.993,1.007) | 0.989 | ||
| ALT(以≤50 U/L为参照) | ||||
| >50 U/L | 0.995(0.987,1.004) | 0.262 | ||
| LDH(以≤245 U/L为参照) | ||||
| >245 U/L | 1.003(0.995,1.010) | 0.534 | ||
| TBIL(以≤7.0 μmol/L为参照) | ||||
| >7.0 μmol/L | 0.971(0.935,1.008) | 0.119 | ||
| DBIL(以≤15 .0μmol/L为参照) | ||||
| >15.0 μmol/L | 0.955(0.893,1.020) | 0.171 | ||
| ALB(以≥32.0 g/L为参照) | ||||
| <32.0 g/L | 0.903(0.799,1.020) | 0.100 | ||
| GLB(以≥ 25.0 g/L为参照) | ||||
| <25.0 g/L | 1.013(0.904,1.136) | 0.822 | ||
| INR(以≤1.3为参照) | ||||
| >1.3 | 5.135(1.054,25.020) | 0.043 | 4.305(0.735,22.180) | 0.089 |
| PT(以≤14.0 s为参照) | ||||
| >14.0 s | 0.992(0.667,1.477) | 0.970 | ||
| APTT(以≤45.0 s为参照) | ||||
| >45.0 s | 0.981(0.891,1.080) | 0.690 | ||
| FIB(以≥2.00 g/L为参照) | ||||
| <2.00 g/L | 0.719(0.506,1.023) | 0.067 | ||
表4 肝癌大范围肝切除术后患者发生PLSMM相关危险因素的单因素及多因素Logistic回归分析
Table 4 Univariate and multivariate Logistic analyses of risk factors associated with PLSMM after major hepatectomy for liver cancer
| 自变量 | 单因素分析 | 多因素分析 | ||
|---|---|---|---|---|
| OR(95%CI) | P值 | OR(95%CI) | P值 | |
| 性别(以男为参照) | ||||
| 女 | 1.410(0.602,3.304) | 0.429 | ||
| BMI(以≥18.0 kg/m2为参照) | ||||
| <18.0 kg/m2 | 0.928(0.805,1.069) | 0.328 | ||
| 术前肌少症(以无为参照) | ||||
| 有 | 1.520(0.640,3.611) | 0.342 | ||
| 病毒性肝炎(以无为参照) | ||||
| 有 | 1.022(0.398,2.623) | 0.964 | ||
| 肝硬化(以无为参照) | ||||
| 有 | 1.187(0.471,2.990) | 0.716 | ||
| ICG-R15(以≤10为参照) | ||||
| >10 | 0.961(0.832,1.111) | 0.593 | ||
| 剩余肝体积(以≥40%为参照) | ||||
| <40% | 0.992(0.937,1.050) | 0.777 | ||
| 手术时间(以≤210 min为参照) | ||||
| >210 min | 2.803(1.127,6.973) | 0.027 | 1.973(1.286,4.936) | 0.038 |
| 失血量(以≤500 mL为参照) | ||||
| >500 mL | 1.002(1.001,1.004) | 0.005 | 1.001(1.000,1.004) | 0.152 |
| 输血(以无为参照) | ||||
| 有 | 1.565(0.587,4.176) | 0.369 | ||
| MVI(以无为参照) | ||||
| 有 | 2.65(1.024,6.860) | 0.045 | 2.751(1.173,6.642) | 0.041 |
| WBC(以≤9.00×109/L为参照) | ||||
| >9.00×109/L | 1.199(1.013,1.418) | 0.034 | 1.153(0.895,1.377) | 0.143 |
| HB(以≥100.0 g/L为参照) | ||||
| <100.0 g/L | 1.005(0.979,1.032) | 0.688 | ||
| PLT(以≥125.0×109/L为参照) | ||||
| <125.0×109/L | 0.979(0.972,1.006) | 0.750 | ||
| NEU(以≤6.0×109/L为参照) | ||||
| >6.0×109/L | 1.006(0.831,1.216) | 0.954 | ||
| LYM(以≥1.1×109/L为参照) | ||||
| <1.1×109/L | 1.005(0.301,3.352) | 0.994 | ||
| AST(以≤50 U/L为参照) | ||||
| >50 U/L | 1.000(0.993,1.007) | 0.989 | ||
| ALT(以≤50 U/L为参照) | ||||
| >50 U/L | 0.995(0.987,1.004) | 0.262 | ||
| LDH(以≤245 U/L为参照) | ||||
| >245 U/L | 1.003(0.995,1.010) | 0.534 | ||
| TBIL(以≤7.0 μmol/L为参照) | ||||
| >7.0 μmol/L | 0.971(0.935,1.008) | 0.119 | ||
| DBIL(以≤15 .0μmol/L为参照) | ||||
| >15.0 μmol/L | 0.955(0.893,1.020) | 0.171 | ||
| ALB(以≥32.0 g/L为参照) | ||||
| <32.0 g/L | 0.903(0.799,1.020) | 0.100 | ||
| GLB(以≥ 25.0 g/L为参照) | ||||
| <25.0 g/L | 1.013(0.904,1.136) | 0.822 | ||
| INR(以≤1.3为参照) | ||||
| >1.3 | 5.135(1.054,25.020) | 0.043 | 4.305(0.735,22.180) | 0.089 |
| PT(以≤14.0 s为参照) | ||||
| >14.0 s | 0.992(0.667,1.477) | 0.970 | ||
| APTT(以≤45.0 s为参照) | ||||
| >45.0 s | 0.981(0.891,1.080) | 0.690 | ||
| FIB(以≥2.00 g/L为参照) | ||||
| <2.00 g/L | 0.719(0.506,1.023) | 0.067 | ||
| 自变量 | 单因素分析 | 多因素分析 | ||
|---|---|---|---|---|
| OR(95%CI) | P值 | OR(95%CI) | P值 | |
| 性别(以男为参照) | ||||
| 女 | 1.135(0.511,2.519) | 0.756 | ||
| BMI(以≥18.0 kg/m2为参照) | ||||
| <18.0 kg/m2 | 0.972(0.855,1.105) | 0.665 | ||
| PLSMM(以无为参照) | ||||
| 有 | 3.055(1.262,7.395) | 0.013 | 2.591(1.173,6.977) | 0.016 |
| 术前肌少症(以无为参照) | ||||
| 有 | 2.168(1.176,4.683) | 0.047 | 1.798(1.133,3.792) | 0.042 |
| 病毒性肝炎(以无为参照) | ||||
| 有 | 0.556(0.223,1.381) | 0.206 | ||
| 肝硬化(以无为参照) | ||||
| 有 | 0.772(0.319,1.870) | 0.567 | ||
| ICG-R15(以≤10为参照) | ||||
| >10 | 0.927(0.808,1.063) | 0.278 | ||
| 剩余肝体积(以≥40%为参照) | ||||
| <40% | 0.964(0.913,1.018) | 0.191 | ||
| 手术时间(以≤210 min为参照) | ||||
| >210 min | 5.359(2.214,12.970) | <0.001 | 3.439(1.206,9.809) | 0.021 |
| 失血量(以≤500 mL为参照) | ||||
| >500 mL | 1.003(1.002,1.005) | <0.001 | 1.004(1.001,1.007) | 0.027 |
| 输血(以无为参照) | ||||
| 有 | 3.041(1.110,8.334) | 0.047 | 0.259(0.036,1.846) | 0.178 |
| MVI(以无为参照) | ||||
| 有 | 2.258(0.875,5.826) | 0.092 | ||
| WBC(以≤9.00×109/L为参照) | ||||
| >9.00×109/L | 1.304(1.091,1.558) | 0.004 | 1.154(0.842,1.582) | 0.372 |
| HB(以≥100.0 g/L为参照) | ||||
| <100.0 g/L | 0.951(0.924,0.979) | 0.060 | ||
| PLT(以≥125.0×109/L为参照) | ||||
| <125.0×109/L | 1.000(0.994,1.007) | 0.857 | ||
| NEU(以≤6.0×109/L为参照) | ||||
| >6.0×109/L | 1.266(1.042,1.538) | 0.017 | 1.092(0.786,1.516) | 0.601 |
| LYM(以≥1.1×109/L为参照) | ||||
| <1.1×109/L | 1.141(0.367,3.549) | 0.820 | ||
| AST(以≤50 U/L为参照) | ||||
| >50 U/L | 1.000(0.993,1.007) | 0.929 | ||
| ALT(以≤50 U/L为参照) | ||||
| >50 U/L | 0.999(0.994,1.003) | 0.539 | ||
| LDH(以≤245 U/L为参照) | ||||
| >245 U/L | 1.005(0.997,1.013) | 0.200 | ||
| TBIL(以≤7.0 μmol/L为参照) | ||||
| >7.0 μmol/L | 1.032(0.997,1.067) | 0.073 | ||
| DBIL(以≤15.0 μmol/L为参照) | ||||
| >15.0 μmol/L | 1.091(1.021,1.166) | 0.058 | ||
| ALB(以≥32.0 g/L为参照) | ||||
| <32.0 g/L | 0.863(0.765,0.974) | 0.017 | 0.880(0.747,1.037) | 0.127 |
| GLB(以≥25.0 g/L为参照) | ||||
| <25.0 g/L | 0.993(0.892,1.106) | 0.904 | ||
| INR(以≤1.3为参照) | ||||
| >1.3 | 2.526(0.591,10.79) | 0.211 | ||
| PT(以≤14.0 s为参照) | ||||
| >14.0 s | 0.838(0.573,1.225) | 0.360 | ||
| APTT(以≤45.0 s为参照) | ||||
| >45.0 s | 0.975(0.891,1.067) | 0.579 | ||
| FIB(以≥2.00 g/L为参照) | ||||
| <2.00 g/L | 1.131(0.84,1.523) | 0.417 | ||
表5 肝癌大范围肝切除术后患者发生并发症相关危险因素的单因素及多因素Logistic回归分析
Table 5 Univariate and multivariate Logistic analyses of risk factors associated with overall postoperative complications of PLSMM after major hepatectomy for liver cancer patients
| 自变量 | 单因素分析 | 多因素分析 | ||
|---|---|---|---|---|
| OR(95%CI) | P值 | OR(95%CI) | P值 | |
| 性别(以男为参照) | ||||
| 女 | 1.135(0.511,2.519) | 0.756 | ||
| BMI(以≥18.0 kg/m2为参照) | ||||
| <18.0 kg/m2 | 0.972(0.855,1.105) | 0.665 | ||
| PLSMM(以无为参照) | ||||
| 有 | 3.055(1.262,7.395) | 0.013 | 2.591(1.173,6.977) | 0.016 |
| 术前肌少症(以无为参照) | ||||
| 有 | 2.168(1.176,4.683) | 0.047 | 1.798(1.133,3.792) | 0.042 |
| 病毒性肝炎(以无为参照) | ||||
| 有 | 0.556(0.223,1.381) | 0.206 | ||
| 肝硬化(以无为参照) | ||||
| 有 | 0.772(0.319,1.870) | 0.567 | ||
| ICG-R15(以≤10为参照) | ||||
| >10 | 0.927(0.808,1.063) | 0.278 | ||
| 剩余肝体积(以≥40%为参照) | ||||
| <40% | 0.964(0.913,1.018) | 0.191 | ||
| 手术时间(以≤210 min为参照) | ||||
| >210 min | 5.359(2.214,12.970) | <0.001 | 3.439(1.206,9.809) | 0.021 |
| 失血量(以≤500 mL为参照) | ||||
| >500 mL | 1.003(1.002,1.005) | <0.001 | 1.004(1.001,1.007) | 0.027 |
| 输血(以无为参照) | ||||
| 有 | 3.041(1.110,8.334) | 0.047 | 0.259(0.036,1.846) | 0.178 |
| MVI(以无为参照) | ||||
| 有 | 2.258(0.875,5.826) | 0.092 | ||
| WBC(以≤9.00×109/L为参照) | ||||
| >9.00×109/L | 1.304(1.091,1.558) | 0.004 | 1.154(0.842,1.582) | 0.372 |
| HB(以≥100.0 g/L为参照) | ||||
| <100.0 g/L | 0.951(0.924,0.979) | 0.060 | ||
| PLT(以≥125.0×109/L为参照) | ||||
| <125.0×109/L | 1.000(0.994,1.007) | 0.857 | ||
| NEU(以≤6.0×109/L为参照) | ||||
| >6.0×109/L | 1.266(1.042,1.538) | 0.017 | 1.092(0.786,1.516) | 0.601 |
| LYM(以≥1.1×109/L为参照) | ||||
| <1.1×109/L | 1.141(0.367,3.549) | 0.820 | ||
| AST(以≤50 U/L为参照) | ||||
| >50 U/L | 1.000(0.993,1.007) | 0.929 | ||
| ALT(以≤50 U/L为参照) | ||||
| >50 U/L | 0.999(0.994,1.003) | 0.539 | ||
| LDH(以≤245 U/L为参照) | ||||
| >245 U/L | 1.005(0.997,1.013) | 0.200 | ||
| TBIL(以≤7.0 μmol/L为参照) | ||||
| >7.0 μmol/L | 1.032(0.997,1.067) | 0.073 | ||
| DBIL(以≤15.0 μmol/L为参照) | ||||
| >15.0 μmol/L | 1.091(1.021,1.166) | 0.058 | ||
| ALB(以≥32.0 g/L为参照) | ||||
| <32.0 g/L | 0.863(0.765,0.974) | 0.017 | 0.880(0.747,1.037) | 0.127 |
| GLB(以≥25.0 g/L为参照) | ||||
| <25.0 g/L | 0.993(0.892,1.106) | 0.904 | ||
| INR(以≤1.3为参照) | ||||
| >1.3 | 2.526(0.591,10.79) | 0.211 | ||
| PT(以≤14.0 s为参照) | ||||
| >14.0 s | 0.838(0.573,1.225) | 0.360 | ||
| APTT(以≤45.0 s为参照) | ||||
| >45.0 s | 0.975(0.891,1.067) | 0.579 | ||
| FIB(以≥2.00 g/L为参照) | ||||
| <2.00 g/L | 1.131(0.84,1.523) | 0.417 | ||
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [21] |
|
| [1] | 胡洁蔓, 谭斐翔, 袁安新, 陈世宇, 唐楚蕾, 殷月姮, 巴磊, 许勤. 结直肠癌患者术后衰弱变化轨迹及影响因素研究[J]. 中国全科医学, 2025, 28(26): 3276-3282. |
| [2] | 丑欣彤, 彭瀚瑜, 马慧, 张珍, 苏先, 邱红燕. 产妇对避孕决策的偏好及其影响因素研究[J]. 中国全科医学, 2025, 28(26): 3294-3299. |
| [3] | 魏姣花, 彭慧如, 彭建业, 谭文婷, 黄金娥, 方立. MOTS-c在心房颤动患者血清中的表达及其与心房重构的相关性研究[J]. 中国全科医学, 2025, 28(26): 3271-3276. |
| [4] | 褚艺婧, 严雨格, 顾杰, 席彪, 祝墡珠, 黄蛟灵. 中国基层医务人员留用意愿影响因素分析:基于城乡差异比较[J]. 中国全科医学, 2025, 28(25): 3161-3168. |
| [5] | 余孜孜, 刘杜丽, 李熙敏, 阮春怡, 尹向阳, 蔡乐. 农村高血压患病和自我管理现状及影响因素研究[J]. 中国全科医学, 2025, 28(25): 3137-3143. |
| [6] | 范博阳, 张玉, 孙雯宁, 张慧芳, 王英杰, 张奥, 赵洋, 王海鹏. 基层医生慢性病医防融合服务行为意向及影响因素研究[J]. 中国全科医学, 2025, 28(25): 3144-3150. |
| [7] | 王汝朋, 南京, 胡奕然, 杨升华, 金泽宁. 三酰甘油-葡萄糖体质量指数对2型糖尿病合并急性心肌梗死行急诊经皮冠状动脉介入治疗术后患者慢血流/无复流的预测价值研究[J]. 中国全科医学, 2025, 28(24): 2985-2992. |
| [8] | 吴越, 王雪彤, 柯碧莲. 近视性黄斑病变低视力患者视觉相关生活质量评估及影响因素研究[J]. 中国全科医学, 2025, 28(23): 2908-2914. |
| [9] | 丁梓峻, 周南男, 罗星, 罗洁羽, 郝文娟, 张春江, 金鑫, 赵丹. 维持性血液透析患者认知障碍情况及其影响因素:一项多中心横断面研究[J]. 中国全科医学, 2025, 28(23): 2885-2893. |
| [10] | 尉晓霞, 陈诺, 王娟娟, 朱静芬. 职校生抑郁和焦虑情绪对吸烟行为的影响研究[J]. 中国全科医学, 2025, 28(22): 2826-2832. |
| [11] | 赵晓晴, 郭桐桐, 张欣怡, 李林虹, 张亚, 嵇丽红, 董志伟, 高倩倩, 蔡伟芹, 郑文贵, 井淇. 社区老年人认知障碍风险预测模型的构建与验证研究[J]. 中国全科医学, 2025, 28(22): 2776-2783. |
| [12] | 郝爱华, 曾子莹, 金爱琼, 唐玲玲, 郑梓悫, 马景泰, 赵建国, 曾韦霖, 肖建鹏, 聂辉, 杨颖. 老年高血压患者可避免住院的影响因素研究[J]. 中国全科医学, 2025, 28(19): 2370-2375. |
| [13] | 黄志杰, 麦志华, 王皓翔, 何煜明, 邓巧妍, 戴燃然, 周志衡. 老年"三高"共患情况和家庭功能的现状及影响因素研究[J]. 中国全科医学, 2025, 28(16): 2001-2010. |
| [14] | 赵璨, 申颖, 奚谦, 彭厚瑄, 覃金琼, 王璇, 郑艳萍, 覃丽, 左延莉. 广西壮族自治区乡镇卫生院多重慢病患者的住院费用及影响因素研究[J]. 中国全科医学, 2025, 28(16): 2039-2049. |
| [15] | 绳菁煜, 刘凡凡, 马梅, 田霖, 刘雨桐, 刘凤敏, 高杉, 于春泉. 冠心病患者血尿素氮与血清白蛋白比值与颈动脉斑块的相关性研究[J]. 中国全科医学, 2025, 28(15): 1831-1839. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





