中国全科医学 ›› 2022, Vol. 25 ›› Issue (27): 3414-3421.DOI: 10.12114/j.issn.1007-9572.2022.0317
所属专题: 睡眠问题专题研究
杜莉1, 熊小花1, 段芳芳2, 任雪3, 羊春菊1, 关义婷1, 王配配1,*( )
)
收稿日期:2022-06-07
修回日期:2022-06-24
出版日期:2022-09-20
发布日期:2022-07-14
通讯作者:
王配配
基金资助:
Li DU1, Xiaohua XIONG1, Fangfang DUAN2, Xue REN3, Chunju YANG1, Yiting GUAN1, Peipei WANG1,*( )
)
Received:2022-06-07
Revised:2022-06-24
Published:2022-09-20
Online:2022-07-14
Contact:
Peipei WANG
About author:摘要: 背景 阻塞性睡眠呼吸暂停低通气综合征(OSAHS)是一种常见的慢性睡眠呼吸障碍,无创正压通气(NPPV)是该疾病的首选治疗方式,但治疗依从性差影响了该疗法的临床应用与推广。 目的 探究OSAHS患者对NPPV治疗的接受情况及影响因素。 方法 选取2019年12月至2021年12月就诊于三亚中心医院(海南省第三人民医院)睡眠医学科且符合NPPV治疗指征的OSAHS患者(年龄≥18岁)为研究对象。根据NPPV滴定接受与否将患者分为接受滴定组和拒绝滴定组,比较两组患者人口学资料及临床资料;根据NPPV治疗接受与否将患者分为接受治疗组与拒绝治疗组,比较两组人口学资料及临床资料。采用多因素Logistic回归分析探讨患者对NPPV压力滴定接受、NPPV治疗接受的影响因素。 结果 共纳入402例符合条件的OSAHS患者。327例患者拒绝NPPV治疗,其中245例(74.9%)在确诊后未进行压力滴定就直接拒绝NPPV治疗,拒绝最常见的原因是对疾病及其风险认知不足,认为无治疗必要性;82例(25.1%)在进行压力滴定后拒绝NPPV治疗,拒绝最常见的原因是认为长期NPPV治疗不方便。仅75例(75/402,18.7%)接受了NPPV治疗。接受滴定组和拒绝滴定组人口学资料、临床资料比较,差异均无统计学意义(P>0.05)。多因素Logistic回归分析显示,人口学资料、临床资料不影响患者对压力滴定的接受情况(P>0.05)。单因素分析显示,与拒绝治疗组相比,接受治疗组中年人(45~59岁)占比高(49.3% vs 33.3%)、老年人(年龄≥60岁)占比低(12.0% vs 32.1%)、伴夜间憋醒比例高(38.7% vs 26.3%)、重度OSAHS患者占比高(64.0% vs 47.4%)、夜间平均血氧饱和度(SPO2)及最低SPO2均更低、SPO2低于90%的时间(T90)更长(P<0.05)。多因素Logistic回归分析显示,年龄、T90是患者NPPV治疗接受情况的影响因素(P<0.05)。控制其他因素后发现,年龄〔OR=0.39,95%CI(0.16,0.93),P<0.05〕、T90〔OR=1.14,95%CI(1.01,1.29),P<0.05〕仍是患者NPPV治疗接受情况的影响因素。 结论 OSAHS患者的NPPV治疗接受情况不佳,年龄、T90是其影响因素。未来在诊疗过程中应加强对患者,尤其是超过60岁患者的教育及认知行为干预,以提高NPPV接受情况。同时应注重全流程管理,增强NPPV治疗依从性。
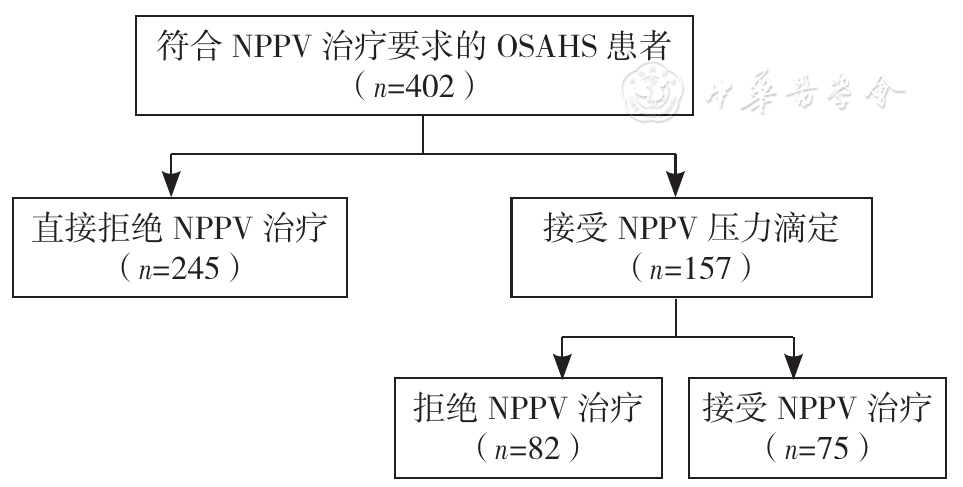
图1 OSAHS患者的NPPV治疗参与流程图注:NPPV=无创正压通气,OSAHS=阻塞性睡眠呼吸暂停低通气综合征
Figure 1 Flow diagram of the enrollment of OSAHS patients with indications for NPPV accepting or rejecting NPPV
| 项目 | 接受滴定组(n=157) | 拒绝滴定组(n=245) | 检验统计量值 | P值 | |
|---|---|---|---|---|---|
| 年龄〔n(%)〕 | -0.61c | 0.542 | |||
| 青年组(18~44岁) | 55(35.0) | 87(35.5) | |||
| 中年组(45~59岁) | 63(40.1) | 83(33.9) | |||
| 老年组(≥60岁) | 39(24.9) | 75(30.6) | |||
| 性别〔n(%)〕 | 0.54a | 0.463 | |||
| 男 | 118(75.2) | 176(71.8) | |||
| 女 | 39(24.8) | 69(28.2) | |||
| 民族〔n(%)〕 | 0.15b | 0.697 | |||
| 汉族 | 155(98.7) | 244(99.6) | |||
| 少数民族 | 2(1.3) | 1(0.4) | |||
| 文化程度〔n(%)〕 | 4.37a | 0.113 | |||
| 小学及以下 | 54(34.4) | 62(25.3) | |||
| 初中-高中 | 62(39.5) | 102(41.6) | |||
| 大学及以上 | 41(26.1) | 81(33.1) | |||
| 合并症〔n(%)〕 | 27(17.2) | 43(17.6) | 0.01a | 0.927 | |
| 夜间失眠易醒〔n(%)〕 | 66(42.0) | 112(45.7) | 0.52a | 0.469 | |
| 夜间憋醒〔n(%)〕 | 49(31.2) | 66(26.9) | 0.86a | 0.355 | |
| 日间嗜睡〔n(%)〕 | 77(49.0) | 108(44.1) | 0.95a | 0.330 | |
| 颈围〔M(P25,P75),㎝〕 | 40.0(37.0,42.0) | 39.0(37.0,41.0) | -0.94c | 0.347 | |
| 腹围〔M(P25,P75),㎝〕 | 95.0(88.5,102.0) | 94.0(89.0,101.0) | -0.22c | 0.825 | |
| 臀围〔M(P25,P75),㎝〕 | 101.0(97.0,105.5) | 97.0(97.0,105.0) | -0.42c | 0.674 | |
| BMI〔M(P25,P75),kg/m2〕 | 26.2(23.2,28.9) | 25.8(23.8,29.2) | -0.25c | 0.807 | |
| ESS〔M(P25,P75),分〕 | 9.0(5.0,12.0) | 7.0(4.0,12.0) | -1.64c | 0.101 | |
| OSAHS严重程度〔n(%)〕 | -1.09c | 0.278 | |||
| 轻度 | 23(14.6) | 35(14.3) | |||
| 中度 | 48(30.6) | 93(38.0) | |||
| 重度 | 86(54.8) | 117(47.7) | |||
| 平均SPO2〔M(P25,P75),%〕 | 94.0(92.5,95.2) | 93.9(92.4,95.2) | -0.16c | 0.873 | |
| LSPO2〔M(P25,P75),%〕 | 80.0(70.0,85.0) | 81.0(73.0,85.0) | -1.25c | 0.211 | |
| T90〔M(P25,P75),/30min〕 | 0.6(0.1,2.0) | 0.4(0.1,1.9) | -0.97c | 0.332 | |
表1 NPPV接受滴定组与拒绝滴定组人口学特征及临床资料比较
Table 1 Comparison of demographic and clinical characteristics between acceptors and rejecters of NPPV titration
| 项目 | 接受滴定组(n=157) | 拒绝滴定组(n=245) | 检验统计量值 | P值 | |
|---|---|---|---|---|---|
| 年龄〔n(%)〕 | -0.61c | 0.542 | |||
| 青年组(18~44岁) | 55(35.0) | 87(35.5) | |||
| 中年组(45~59岁) | 63(40.1) | 83(33.9) | |||
| 老年组(≥60岁) | 39(24.9) | 75(30.6) | |||
| 性别〔n(%)〕 | 0.54a | 0.463 | |||
| 男 | 118(75.2) | 176(71.8) | |||
| 女 | 39(24.8) | 69(28.2) | |||
| 民族〔n(%)〕 | 0.15b | 0.697 | |||
| 汉族 | 155(98.7) | 244(99.6) | |||
| 少数民族 | 2(1.3) | 1(0.4) | |||
| 文化程度〔n(%)〕 | 4.37a | 0.113 | |||
| 小学及以下 | 54(34.4) | 62(25.3) | |||
| 初中-高中 | 62(39.5) | 102(41.6) | |||
| 大学及以上 | 41(26.1) | 81(33.1) | |||
| 合并症〔n(%)〕 | 27(17.2) | 43(17.6) | 0.01a | 0.927 | |
| 夜间失眠易醒〔n(%)〕 | 66(42.0) | 112(45.7) | 0.52a | 0.469 | |
| 夜间憋醒〔n(%)〕 | 49(31.2) | 66(26.9) | 0.86a | 0.355 | |
| 日间嗜睡〔n(%)〕 | 77(49.0) | 108(44.1) | 0.95a | 0.330 | |
| 颈围〔M(P25,P75),㎝〕 | 40.0(37.0,42.0) | 39.0(37.0,41.0) | -0.94c | 0.347 | |
| 腹围〔M(P25,P75),㎝〕 | 95.0(88.5,102.0) | 94.0(89.0,101.0) | -0.22c | 0.825 | |
| 臀围〔M(P25,P75),㎝〕 | 101.0(97.0,105.5) | 97.0(97.0,105.0) | -0.42c | 0.674 | |
| BMI〔M(P25,P75),kg/m2〕 | 26.2(23.2,28.9) | 25.8(23.8,29.2) | -0.25c | 0.807 | |
| ESS〔M(P25,P75),分〕 | 9.0(5.0,12.0) | 7.0(4.0,12.0) | -1.64c | 0.101 | |
| OSAHS严重程度〔n(%)〕 | -1.09c | 0.278 | |||
| 轻度 | 23(14.6) | 35(14.3) | |||
| 中度 | 48(30.6) | 93(38.0) | |||
| 重度 | 86(54.8) | 117(47.7) | |||
| 平均SPO2〔M(P25,P75),%〕 | 94.0(92.5,95.2) | 93.9(92.4,95.2) | -0.16c | 0.873 | |
| LSPO2〔M(P25,P75),%〕 | 80.0(70.0,85.0) | 81.0(73.0,85.0) | -1.25c | 0.211 | |
| T90〔M(P25,P75),/30min〕 | 0.6(0.1,2.0) | 0.4(0.1,1.9) | -0.97c | 0.332 | |
| 影响因素 | β | SE | Wald χ2值 | OR(95%CI) | P值 | |
|---|---|---|---|---|---|---|
| 常数项 | 0.762 | 1.228 | 0.385 | 2.142 | 0.535 | |
| 年龄〔以青年组(18~44岁)为参照〕 | ||||||
| 中年组(45~59岁) | 0.200 | 0.263 | 0.580 | 1.222(0.729,2.047) | 0.446 | |
| 老年组(≥60岁) | -0.210 | 0.296 | 0.502 | 0.811(0.454,1.448) | 0.479 | |
| 性别(以男性为参照) | ||||||
| 女性 | -0.038 | 0.274 | 0.020 | 0.962(0.562,1.648) | 0.889 | |
| 合并症(以否为参照) | ||||||
| 是 | 0.021 | 0.285 | 0.005 | 1.021(0.584,1.785) | 0.942 | |
| 夜间失眠易醒(以否为参照) | ||||||
| 是 | -0.163 | 0.230 | 0.505 | 0.849(0.542,1.332) | 0.477 | |
| 夜间憋醒(以否为参照) | ||||||
| 是 | -0.005 | 0.247 | 0.000 | 0.995(0.613,1.614) | 0.983 | |
| 日间嗜睡(以否为参照) | ||||||
| 是 | 0.054 | 0.230 | 0.054 | 1.055(0.672,1.658) | 0.816 | |
| 颈围 | -0.009 | 0.031 | 0.093 | 0.991(0.933,1.052) | 0.761 | |
| BMI | -0.039 | 0.032 | 1.505 | 0.962(0.904,1.023) | 0.220 | |
| ESS | 0.030 | 0.024 | 1.590 | 1.031(0.983,1.080) | 0.207 | |
| OSAHS严重程度(以轻度为参照) | ||||||
| 中度 | -0.301 | 0.336 | 0.801 | 0.740(0.383,1.431) | 0.371 | |
| 重度 | -0.077 | 0.345 | 0.050 | 0.926(0.471,1.819) | 0.823 | |
| T90 | 0.067 | 0.053 | 1.606 | 1.070(0.964,1.187) | 0.205 | |
表2 NPPV滴定接受情况影响因素的多因素Logistic回归分析
Table 2 Multivariate Logistic regression analysis of factors associated with NPPV titration acceptance
| 影响因素 | β | SE | Wald χ2值 | OR(95%CI) | P值 | |
|---|---|---|---|---|---|---|
| 常数项 | 0.762 | 1.228 | 0.385 | 2.142 | 0.535 | |
| 年龄〔以青年组(18~44岁)为参照〕 | ||||||
| 中年组(45~59岁) | 0.200 | 0.263 | 0.580 | 1.222(0.729,2.047) | 0.446 | |
| 老年组(≥60岁) | -0.210 | 0.296 | 0.502 | 0.811(0.454,1.448) | 0.479 | |
| 性别(以男性为参照) | ||||||
| 女性 | -0.038 | 0.274 | 0.020 | 0.962(0.562,1.648) | 0.889 | |
| 合并症(以否为参照) | ||||||
| 是 | 0.021 | 0.285 | 0.005 | 1.021(0.584,1.785) | 0.942 | |
| 夜间失眠易醒(以否为参照) | ||||||
| 是 | -0.163 | 0.230 | 0.505 | 0.849(0.542,1.332) | 0.477 | |
| 夜间憋醒(以否为参照) | ||||||
| 是 | -0.005 | 0.247 | 0.000 | 0.995(0.613,1.614) | 0.983 | |
| 日间嗜睡(以否为参照) | ||||||
| 是 | 0.054 | 0.230 | 0.054 | 1.055(0.672,1.658) | 0.816 | |
| 颈围 | -0.009 | 0.031 | 0.093 | 0.991(0.933,1.052) | 0.761 | |
| BMI | -0.039 | 0.032 | 1.505 | 0.962(0.904,1.023) | 0.220 | |
| ESS | 0.030 | 0.024 | 1.590 | 1.031(0.983,1.080) | 0.207 | |
| OSAHS严重程度(以轻度为参照) | ||||||
| 中度 | -0.301 | 0.336 | 0.801 | 0.740(0.383,1.431) | 0.371 | |
| 重度 | -0.077 | 0.345 | 0.050 | 0.926(0.471,1.819) | 0.823 | |
| T90 | 0.067 | 0.053 | 1.606 | 1.070(0.964,1.187) | 0.205 | |
| 项目 | 接受治疗组(n=75) | 拒绝治疗组(n=327) | 检验统计量值 | P值 | |
|---|---|---|---|---|---|
| 年龄〔n(%)〕 | -2.29c | 0.022 | |||
| 青年组(18~44岁) | 29(38.7) | 113(34.6) | |||
| 中年组(45~59岁) | 37(49.3) | 109(33.3) | |||
| 老年组(≥60岁) | 9(12.0) | 105(32.1) | |||
| 性别〔n(%)〕 | 0.83a | 0.363 | |||
| 男 | 58(77.3) | 236(72.2) | |||
| 女 | 17(22.7) | 91(27.8) | |||
| 民族〔n(%)〕 | 1.96b | 0.162 | |||
| 汉族 | 73(97.3) | 326(99.7) | |||
| 少数民族 | 2(2.7) | 1(0.3) | |||
| 文化程度〔n(%)〕 | 3.56a | 0.169 | |||
| 小学及以下 | 15(20.0) | 101(30.9) | |||
| 初中-高中 | 35(46.7) | 129(39.4) | |||
| 大学及以上 | 25(33.3) | 97(29.7) | |||
| 合并症〔n(%)〕 | 11(14.7) | 59(18.0) | 0.48a | 0.487 | |
| 夜间失眠易醒〔n(%)〕 | 30(40.0) | 148(45.3) | 0.68a | 0.408 | |
| 夜间憋醒〔n(%)〕 | 29(38.7) | 86(26.3) | 4.57a | 0.033 | |
| 日间嗜睡〔n(%)〕 | 38(50.7) | 147(45.0) | 0.80a | 0.371 | |
| 颈围〔M(P25,P75),㎝〕 | 40.0(37.0,42.0) | 39.0(37.0,41.0) | -0.97c | 0.330 | |
| 腹围〔M(P25,P75),㎝〕 | 97.0(89.0,103.0) | 94.0(89.0,101.0) | -1.23c | 0.210 | |
| 臀围〔M(P25,P75),㎝〕 | 101.0(98.0,106.0) | 101.0(97.0,105.0) | -0.62c | 0.538 | |
| BMI〔M(P25,P75),kg/m2〕 | 26.6(24.0,29.3) | 25.8(23.6,29.0) | -1.01c | 0.313 | |
| ESS〔M(P25,P75),分〕 | 10.0(6.0,12.0) | 8.0(5.0,12.0) | -1.56c | 0.119 | |
| OSAHS严重程度〔n(%)〕 | -2.57c | 0.010 | |||
| 轻度 | 7(9.3) | 51(15.6) | |||
| 中度 | 20(26.7) | 121(37.0) | |||
| 重度 | 48(64.0) | 155(47.4) | |||
| 平均SPO2〔M(P25,P75),%〕 | 93.3(91.9,94.9) | 94.1(92.6,95.3) | -2.10c | 0.035 | |
| LSPO2〔M(P25,P75),%〕 | 78.0(67.0,84.0) | 81.0(73.0,85.0) | -2.53c | 0.011 | |
| T90〔M(P25,P75),/30 min〕 | 0.9(0.2,2.6) | 0.4(0.1,1.8) | -2.68c | 0.007 | |
表3 NPPV接受治疗组与拒绝治疗组人口学特征及临床资料比较
Table 3 Comparison of demographic and clinical characteristics between acceptors and rejecters of NPPV
| 项目 | 接受治疗组(n=75) | 拒绝治疗组(n=327) | 检验统计量值 | P值 | |
|---|---|---|---|---|---|
| 年龄〔n(%)〕 | -2.29c | 0.022 | |||
| 青年组(18~44岁) | 29(38.7) | 113(34.6) | |||
| 中年组(45~59岁) | 37(49.3) | 109(33.3) | |||
| 老年组(≥60岁) | 9(12.0) | 105(32.1) | |||
| 性别〔n(%)〕 | 0.83a | 0.363 | |||
| 男 | 58(77.3) | 236(72.2) | |||
| 女 | 17(22.7) | 91(27.8) | |||
| 民族〔n(%)〕 | 1.96b | 0.162 | |||
| 汉族 | 73(97.3) | 326(99.7) | |||
| 少数民族 | 2(2.7) | 1(0.3) | |||
| 文化程度〔n(%)〕 | 3.56a | 0.169 | |||
| 小学及以下 | 15(20.0) | 101(30.9) | |||
| 初中-高中 | 35(46.7) | 129(39.4) | |||
| 大学及以上 | 25(33.3) | 97(29.7) | |||
| 合并症〔n(%)〕 | 11(14.7) | 59(18.0) | 0.48a | 0.487 | |
| 夜间失眠易醒〔n(%)〕 | 30(40.0) | 148(45.3) | 0.68a | 0.408 | |
| 夜间憋醒〔n(%)〕 | 29(38.7) | 86(26.3) | 4.57a | 0.033 | |
| 日间嗜睡〔n(%)〕 | 38(50.7) | 147(45.0) | 0.80a | 0.371 | |
| 颈围〔M(P25,P75),㎝〕 | 40.0(37.0,42.0) | 39.0(37.0,41.0) | -0.97c | 0.330 | |
| 腹围〔M(P25,P75),㎝〕 | 97.0(89.0,103.0) | 94.0(89.0,101.0) | -1.23c | 0.210 | |
| 臀围〔M(P25,P75),㎝〕 | 101.0(98.0,106.0) | 101.0(97.0,105.0) | -0.62c | 0.538 | |
| BMI〔M(P25,P75),kg/m2〕 | 26.6(24.0,29.3) | 25.8(23.6,29.0) | -1.01c | 0.313 | |
| ESS〔M(P25,P75),分〕 | 10.0(6.0,12.0) | 8.0(5.0,12.0) | -1.56c | 0.119 | |
| OSAHS严重程度〔n(%)〕 | -2.57c | 0.010 | |||
| 轻度 | 7(9.3) | 51(15.6) | |||
| 中度 | 20(26.7) | 121(37.0) | |||
| 重度 | 48(64.0) | 155(47.4) | |||
| 平均SPO2〔M(P25,P75),%〕 | 93.3(91.9,94.9) | 94.1(92.6,95.3) | -2.10c | 0.035 | |
| LSPO2〔M(P25,P75),%〕 | 78.0(67.0,84.0) | 81.0(73.0,85.0) | -2.53c | 0.011 | |
| T90〔M(P25,P75),/30 min〕 | 0.9(0.2,2.6) | 0.4(0.1,1.8) | -2.68c | 0.007 | |
| 影响因素 | β | SE | Wald χ2值 | OR(95%CI) | P值 | |
|---|---|---|---|---|---|---|
| 常数项 | 0.118 | 1.915 | 0.004 | 1.125 | 0.951 | |
| 年龄〔以青年组(18~44岁)为参照〕 | ||||||
| 中年组(45~59岁) | 0.391 | 0.317 | 1.522 | 1.479(0.794,2.775) | 0.217 | |
| 老年组(≥60岁) | -0.947 | 0.444 | 4.545 | 0.388(0.162,0.926) | 0.033 | |
| 性别(以男性为参照) | ||||||
| 女性 | 0.055 | 0.393 | 0.020 | 1.056(0.489,2.282) | 0.889 | |
| 合并症(以否为参照) | ||||||
| 是 | -0.298 | 0.376 | 0.625 | 0.743(0.355,1.553) | 0.429 | |
| 夜间失眠易醒(以否为参照) | ||||||
| 是 | -0.146 | 0.298 | 0.240 | 0.864(0.482,1.549) | 0.624 | |
| 夜间憋醒(以否为参照) | ||||||
| 是 | 0.280 | 0.308 | 0.828 | 1.324(0.724,2.421) | 0.363 | |
| 日间嗜睡(以否为参照) | ||||||
| 是 | -0.022 | 0.300 | 0.005 | 0.978(0.543,1.762) | 0.942 | |
| 颈围 | -0.044 | 0.055 | 0.647 | 0.957(0.860,1.065) | 0.421 | |
| BMI | -0.012 | 0.042 | 0.080 | 0.988(0.909,1.074) | 0.778 | |
| ESS | 0.002 | 0.031 | 0.005 | 1.002(0.942,1.066) | 0.946 | |
| OSAHS严重程度(以轻度为参照) | ||||||
| 中度 | 0.018 | 0.489 | 0.001 | 1.018(0.390,2.656) | 0.971 | |
| 重度 | 0.452 | 0.493 | 0.842 | 1.572(0.598,4.130) | 0.359 | |
| T90 | 0.134 | 0.062 | 4.693 | 1.143(1.013,1.291) | 0.030 | |
表4 NPPV治疗接受情况影响因素的多因素Logistic回归分析
Table 4 Multivariate Logistic regression analysis of factors associated with NPPV acceptance
| 影响因素 | β | SE | Wald χ2值 | OR(95%CI) | P值 | |
|---|---|---|---|---|---|---|
| 常数项 | 0.118 | 1.915 | 0.004 | 1.125 | 0.951 | |
| 年龄〔以青年组(18~44岁)为参照〕 | ||||||
| 中年组(45~59岁) | 0.391 | 0.317 | 1.522 | 1.479(0.794,2.775) | 0.217 | |
| 老年组(≥60岁) | -0.947 | 0.444 | 4.545 | 0.388(0.162,0.926) | 0.033 | |
| 性别(以男性为参照) | ||||||
| 女性 | 0.055 | 0.393 | 0.020 | 1.056(0.489,2.282) | 0.889 | |
| 合并症(以否为参照) | ||||||
| 是 | -0.298 | 0.376 | 0.625 | 0.743(0.355,1.553) | 0.429 | |
| 夜间失眠易醒(以否为参照) | ||||||
| 是 | -0.146 | 0.298 | 0.240 | 0.864(0.482,1.549) | 0.624 | |
| 夜间憋醒(以否为参照) | ||||||
| 是 | 0.280 | 0.308 | 0.828 | 1.324(0.724,2.421) | 0.363 | |
| 日间嗜睡(以否为参照) | ||||||
| 是 | -0.022 | 0.300 | 0.005 | 0.978(0.543,1.762) | 0.942 | |
| 颈围 | -0.044 | 0.055 | 0.647 | 0.957(0.860,1.065) | 0.421 | |
| BMI | -0.012 | 0.042 | 0.080 | 0.988(0.909,1.074) | 0.778 | |
| ESS | 0.002 | 0.031 | 0.005 | 1.002(0.942,1.066) | 0.946 | |
| OSAHS严重程度(以轻度为参照) | ||||||
| 中度 | 0.018 | 0.489 | 0.001 | 1.018(0.390,2.656) | 0.971 | |
| 重度 | 0.452 | 0.493 | 0.842 | 1.572(0.598,4.130) | 0.359 | |
| T90 | 0.134 | 0.062 | 4.693 | 1.143(1.013,1.291) | 0.030 | |
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
李晨阳,尚少梅,万巧琴,等. 阻塞性睡眠呼吸暂停患者气道正压通气治疗依从性管理的新技术研究进展[J]. 中华医学杂志,2020,100(34):2712-2715. DOI:10.3760/cma.j.cn112137-20200611-01818.
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
王拢拢,潘敏霞,陈柏欣,等.公务员人群阻塞性睡眠呼吸暂停筛查、干预的新模式及其影响因素[J]. 中华健康管理学杂志,2021,15(3):213-219. DOI:10.3760/cma.j.cn115624-20210406-00181.
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
中华医学会呼吸病学分会睡眠呼吸障碍学组. 睡眠呼吸疾病无创正压通气临床应用专家共识(草案)[J]. 中华结核和呼吸杂志,2017,40(9):667-677. DOI:10.3760/cma.j.issn.1001-0939.2017.09.011.
|
| [16] |
|
| [17] |
彭莉莉,李进让,孙建军,等. Epworth嗜睡量表简体中文版信度和效度评价[J]. 中华耳鼻咽喉头颈外科杂志,2011,46(1):44-49. DOI:10.3760/cma.j.issn.1673-0860.2011.01.018.
|
| [18] |
|
| [19] |
|
| [20] |
李庆云,林莹妮. 应以生物-心理-社会模式全面分析持续气道正压通气依从性的影响因素[J]. 中华医学杂志,2016,96(30):2369-2371. DOI:10.3760/cma.j.issn.0376-2491.2016.30.001.
|
| [21] |
|
| [22] |
|
| [23] |
洪培川,欧琼,潘敏霞,等. 公务员人群对打鼾危害的认知度及阻塞性睡眠呼吸暂停患病率现状调查[J]. 中华结核和呼吸杂志,2020,43(7):553-556. DOI:10.3760/cma.j.cn112147-20191013-00682.
|
| [24] |
|
| [25] |
|
| [26] |
|
| [27] |
|
| [28] |
|
| [29] |
|
| [30] |
韩芳. 阻塞性睡眠呼吸暂停低通气综合征的诊治与医疗保险政策[J]. 中华结核和呼吸杂志,2006,29(4):224-226. DOI:10.3760/j:issn:1001-0939.2006.04.005.
|
| [31] |
中华医学会,中华医学会杂志社,中华医学会全科医学分会,等. 成人阻塞性睡眠呼吸暂停基层诊疗指南(2018年)[J]. 中华全科医师杂志,2019,18(1):21-29. DOI:10.3760/cma.j.issn.1671-7368.2019.01.007.
|
| [32] |
中国医师协会睡眠医学专业委员会.成人阻塞性睡眠呼吸暂停多学科诊疗指南[J]. 中华医学杂志,2018,98(24):1902-1914. DOI:10.3760/cma.j.issn.0376-2491.2018.24.003.
|
| [33] |
中华医学会呼吸病学分会睡眠呼吸学组,中华医学会糖尿病学分会. 阻塞性睡眠呼吸暂停与糖尿病专家共识[J]. 中华糖尿病杂志,2010,2(2):91-96. DOI:10.3760/cma.j.issn.1674-5809.2010.02.004.
|
| [34] |
| [1] | 梁譞, 那飞扬, 秦梦瑶, 杨辉, 郭丽, 郭琪, 任蕾, 陈德, 刘东海, 张蓉芳. 儿童支气管哮喘合并阻塞性睡眠呼吸暂停低通气综合征的临床特征及影响因素研究[J]. 中国全科医学, 2023, 26(33): 4225-4230. |
| [2] | 邓晶晶, 李夏, 薛倩, 邓利华, 王晶桐. 持续正压通气治疗对阻塞性睡眠呼吸暂停合并胃食管反流患者的疗效观察研究[J]. 中国全科医学, 2023, 26(30): 3753-3758. |
| [3] | 卫梦雨, 王佳佳, 张莹莹, 李春阳, 李建生. 阻塞性睡眠呼吸暂停患者报告结局测评工具研究现状分析[J]. 中国全科医学, 2023, 26(30): 3725-3733. |
| [4] | 瞿慧, 李缓, 唐若涵, 杜宇征, 赵琦. 近十年针刺治疗阻塞性睡眠呼吸暂停低通气综合征随机对照试验结局指标分析[J]. 中国全科医学, 2023, 26(30): 3734-3739. |
| [5] | 温雯, 张凯楠, 陈玉岚, 李瑜, 张向阳. 代谢指数作为预测因子与阻塞性睡眠呼吸暂停的相关性分析[J]. 中国全科医学, 2023, 26(30): 3740-3747. |
| [6] | 胡佳玉, 任丽珏, 靳欢欢, 孙婷婷, 靳美娜, 周雪利, 魏翠英. 阻塞性睡眠呼吸暂停综合征患者脂肪因子Metrnl水平及其与炎症和胰岛素抵抗的关系研究[J]. 中国全科医学, 2023, 26(30): 3748-3752. |
| [7] | 蒋秋惠, 李学军. 运动不是减重之本[J]. 中国全科医学, 2023, 26(28): 3477-3481. |
| [8] | 王丹, 王建辉, 董建秀, 常文红, 秦璐, 刘琪, 陈晨. 基于网络干预对经皮冠状动脉介入治疗术后患者运动行为的影响研究[J]. 中国全科医学, 2023, 26(21): 2603-2608. |
| [9] | 丁晓云, 金菊珍, 杨瑾, 周静, 胡瑾, 蒙玥, 梁晓仙, 盖云, 汪俊华, 王子云. 腰围和空腹血糖对40~65岁人群阻塞性睡眠呼吸暂停综合征与动脉硬化关联的中介效应研究[J]. 中国全科医学, 2023, 26(21): 2597-2602. |
| [10] | 费敏, 雷思, 许琰, 叶云, 卓慧, 张慧, 罗荧荃. 阻塞性睡眠呼吸暂停低通气综合征对高血压患者血压变异性和心率变异性的影响研究[J]. 中国全科医学, 2023, 26(20): 2459-2468. |
| [11] | 王晶玉, 洪申达, 韩芳, 刘国莉. 妊娠期阻塞性睡眠呼吸暂停筛查的研究进展[J]. 中国全科医学, 2023, 26(20): 2555-2558,2566. |
| [12] | 陈轶琳, 林平, 韩永奎, 王旖旎. 经皮冠状动脉介入治疗患者Ⅰ期心脏康复依从性及影响因素模型的构建研究[J]. 中国全科医学, 2023, 26(18): 2209-2216. |
| [13] | 任玉梅, 许敏, 叶梅蕾, 章秋, 胡红琳. 胰岛素受体底物2基因突变可能与青少年起病的成人型糖尿病有关:一例报道及其遗传学分析[J]. 中国全科医学, 2023, 26(18): 2301-2305. |
| [14] | 梁振宇, 王凤燕, 陈子正, 陈荣昌. 2023年GOLD慢性阻塞性肺疾病诊断、管理及预防全球策略更新要点解读[J]. 中国全科医学, 2023, 26(11): 1287-1298. |
| [15] | 衣荟洁, 廖欣意, 皮梦媛, 许力月, 张驰, 董霄松, 韩芳. 基于远程医疗的阻塞性睡眠呼吸暂停诊疗新模式的建立:一项非劣效随机对照试验研究方案[J]. 中国全科医学, 2023, 26(03): 380-385. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





