中国全科医学 ›› 2025, Vol. 28 ›› Issue (29): 3674-3683.DOI: 10.12114/j.issn.1007-9572.2024.0625
董称仙1, 邵健将1, 姚腾1, 翟金婵1, 马娇龙1,2, 胡云华1,2, 刘文3, 牛强1,2, 李小菊1,2, 闫贻忠1,2,*( )
)
收稿日期:2024-11-13
修回日期:2025-02-01
出版日期:2025-10-15
发布日期:2025-08-26
通讯作者:
闫贻忠
作者贡献:
董称仙进行数据收集分析,文章撰写;邵健将、姚腾、翟金婵、刘文进行数据收集;马娇龙负责课题设计,论文指导,数据收集;胡云华、刘文、牛强、李小菊负责论文指导;闫贻忠负责课题设计,论文指导,论文审阅,经费支持。
基金资助:
DONG Chenxian1, SHAO Jianjiang1, YAO Teng1, ZHAI Jinchan1, MA Jiaolong1,2, HU Yunhua1,2, LIU Wen3, NIU Qiang1,2, LI Xiaoju1,2, YAN Yizhong1,2,*( )
)
Received:2024-11-13
Revised:2025-02-01
Published:2025-10-15
Online:2025-08-26
Contact:
YAN Yizhong
摘要: 背景 据WHO估计,孕妇中有37%患有贫血。孕妇贫血易引发不良妊娠结局,炎症性贫血较常见,且妊娠期机体有慢性低度炎症,饮食质量在此期间极为关键,其关联着炎症水平与妊娠状况,膳食炎症指数(DII)可评估饮食炎症潜力,多种膳食模式也对炎症有不同影响。 目的 利用DII评估孕妇的饮食炎症潜力,并提取个人主要膳食模式,探讨不同膳食模式下DII与妊娠期贫血发病风险的关联。 方法 选取2023年4月—2024年4月定期于石河子大学第一附属医院产检的≥18岁孕妇参与调查,收集其人口学、生活行为习惯、膳食摄入等信息。通过问卷调查收集社会人口学信息和生活行为信息。使用食物频率问卷(FFQ)收集孕妇饮食信息,计算DII,并根据DII三分位数将孕妇分成:最低三分位(T1)组、第二三分位(T2)组、最高三分位(T3)组。使用主成分分析法评估食物组,并提取膳食模式。采用多因素Logistic回归分析评估DII及膳食模式与妊娠期贫血的发病风险,使用限制性立方样条图(RCS)分析剂量-反应关系。 结果 共纳入653名孕妇,孕妇的DII为-4.87~3.37,平均值为(0.36±1.94),其中T1组217例,T2组218例,T3组218例。172名(26.3%)孕妇被诊断为妊娠期贫血,其DII为(0.64±1.95)。研究共提取4种膳食模式,分别为多样性、鱼虾豆类、牛奶蛋类及加工食品模式。多因素Logistic回归分析结果显示,调整混杂因素后,DII与妊娠期贫血发病风险之间呈正相关(OR=1.21,95%CI=1.05~1.39,P<0.05);总体孕妇中,T3组妊娠期贫血发病风险是T1组的3.05倍(95%CI=1.62~5.75,P<0.05);在以牛奶蛋类和加工食品模式为特征的孕妇中,T3组妊娠期贫血发病风险分别是T1组的7.69倍(95%CI=1.67~35.45,P<0.05)和5.17倍(95%CI=1.29~20.63,P<0.05)。RCS结果显示,在总人群中,当DII>0.7,膳食炎症会增加妊娠期贫血的发病风险。 结论 饮食的炎症倾向与妊娠期贫血发病风险呈正相关,尤其是在以牛奶蛋类和加工食品为特征的孕妇中。因此,应当减少摄入促炎食品,注重均衡饮食。
| 食物成分 | 炎症反应评分(分) | 全球人均摄入均值 | 人均摄入标准差 |
|---|---|---|---|
| 能量(kcal) | 0.18 | 2 056.00 | 338.00 |
| 蛋白质(g) | 0.021 | 79.40 | 13.90 |
| 碳水化合物(g) | 0.097 | 272.20 | 40.00 |
| 膳食纤维(g) | -0.663 | 18.80 | 4.90 |
| 胆固醇(mg) | 0.110 | 279.40 | 51.20 |
| 总脂肪(g) | 0.298 | 71.40 | 19.40 |
| SFA(g) | 0.373 | 28.60 | 8.00 |
| MUFA(g) | -0.009 | 27.00 | 6.10 |
| PUFA(g) | -0.337 | 13.88 | 3.76 |
| n-3脂肪酸(g) | -0.436 | 1.06 | 1.06 |
| n-6脂肪酸(g) | -0.159 | 10.80 | 7.50 |
| 反式脂肪酸(g) | 0.229 | 3.15 | 3.75 |
| β-胡萝卜素(μg) | -0.584 | 3 718.00 | 1 720.00 |
| 维生素A(μgRE) | -0.401 | 983.90 | 518.60 |
| 硫胺素(mg) | -0.098 | 1.70 | 0.66 |
| 核黄素(mg) | -0.068 | 1.70 | 0.79 |
| 维生素C(mg) | -0.424 | 118.20 | 43.46 |
| 维生素D(μg) | -0.446 | 6.26 | 2.21 |
| 维生素E(mg) | -0.419 | 8.73 | 1.49 |
| 维生素B6(mg) | -0.365 | 1.47 | 0.74 |
| 维生素B12(μg) | 0.106 | 5.15 | 2.70 |
| 叶酸(μg) | -0.190 | 273.00 | 70.70 |
| 烟酸(mg) | -0.246 | 25.90 | 11.77 |
| 铁(mg) | -0.484 | 310.10 | 139.40 |
| 镁(mg) | -0.140 | 0.37 | 1.78 |
| 硒(μg) | -0.191 | 67.00 | 25.10 |
| 锌(mg) | -0.313 | 9.84 | 2.19 |
| 丁香酚(mg) | -0.140 | 0.01 | 0.08 |
| 黄酮(mg) | -0.616 | 1.55 | 0.07 |
| 黄酮醇(mg) | -0.467 | 17.70 | 6.79 |
| 黄烷酮(mg) | -0.250 | 11.70 | 3.82 |
| 花青素(mg) | -0.131 | 18.05 | 21.14 |
| 异黄酮素(mg) | -0.593 | 1.20 | 0.2 |
| 黄烷-3-醇(mg) | -0.042 | 95.80 | 85.90 |
| 大蒜(g) | -0.412 | 4.35 | 2.90 |
| 生姜(g) | -0.453 | 59.00 | 63.20 |
| 洋葱(g) | -0.301 | 35.90 | 18.40 |
| 辣椒(g) | -0.131 | 10.00 | 7.07 |
| 百里香/牛至(mg) | -0.102 | 0.33 | 0.99 |
| 迷迭香(mg) | -0.013 | 1.00 | 15.00 |
| 藏红花(g) | 0.032 | 13.35 | 3.71 |
| 姜黄(mg) | -0.785 | 533.60 | 754.30 |
| 绿/红茶(g) | -0.536 | 1.69 | 1.53 |
| 酒精(g) | -0.278 | 13.98 | 3.72 |
| 咖啡因(g) | -0.110 | 8.05 | 6.67 |
表1 各膳食组分的炎性效应分数及全球人均每日摄入水平[8]
Table 1 Inflammatory effect scores and global per capita daily intake levels for each dietary component
| 食物成分 | 炎症反应评分(分) | 全球人均摄入均值 | 人均摄入标准差 |
|---|---|---|---|
| 能量(kcal) | 0.18 | 2 056.00 | 338.00 |
| 蛋白质(g) | 0.021 | 79.40 | 13.90 |
| 碳水化合物(g) | 0.097 | 272.20 | 40.00 |
| 膳食纤维(g) | -0.663 | 18.80 | 4.90 |
| 胆固醇(mg) | 0.110 | 279.40 | 51.20 |
| 总脂肪(g) | 0.298 | 71.40 | 19.40 |
| SFA(g) | 0.373 | 28.60 | 8.00 |
| MUFA(g) | -0.009 | 27.00 | 6.10 |
| PUFA(g) | -0.337 | 13.88 | 3.76 |
| n-3脂肪酸(g) | -0.436 | 1.06 | 1.06 |
| n-6脂肪酸(g) | -0.159 | 10.80 | 7.50 |
| 反式脂肪酸(g) | 0.229 | 3.15 | 3.75 |
| β-胡萝卜素(μg) | -0.584 | 3 718.00 | 1 720.00 |
| 维生素A(μgRE) | -0.401 | 983.90 | 518.60 |
| 硫胺素(mg) | -0.098 | 1.70 | 0.66 |
| 核黄素(mg) | -0.068 | 1.70 | 0.79 |
| 维生素C(mg) | -0.424 | 118.20 | 43.46 |
| 维生素D(μg) | -0.446 | 6.26 | 2.21 |
| 维生素E(mg) | -0.419 | 8.73 | 1.49 |
| 维生素B6(mg) | -0.365 | 1.47 | 0.74 |
| 维生素B12(μg) | 0.106 | 5.15 | 2.70 |
| 叶酸(μg) | -0.190 | 273.00 | 70.70 |
| 烟酸(mg) | -0.246 | 25.90 | 11.77 |
| 铁(mg) | -0.484 | 310.10 | 139.40 |
| 镁(mg) | -0.140 | 0.37 | 1.78 |
| 硒(μg) | -0.191 | 67.00 | 25.10 |
| 锌(mg) | -0.313 | 9.84 | 2.19 |
| 丁香酚(mg) | -0.140 | 0.01 | 0.08 |
| 黄酮(mg) | -0.616 | 1.55 | 0.07 |
| 黄酮醇(mg) | -0.467 | 17.70 | 6.79 |
| 黄烷酮(mg) | -0.250 | 11.70 | 3.82 |
| 花青素(mg) | -0.131 | 18.05 | 21.14 |
| 异黄酮素(mg) | -0.593 | 1.20 | 0.2 |
| 黄烷-3-醇(mg) | -0.042 | 95.80 | 85.90 |
| 大蒜(g) | -0.412 | 4.35 | 2.90 |
| 生姜(g) | -0.453 | 59.00 | 63.20 |
| 洋葱(g) | -0.301 | 35.90 | 18.40 |
| 辣椒(g) | -0.131 | 10.00 | 7.07 |
| 百里香/牛至(mg) | -0.102 | 0.33 | 0.99 |
| 迷迭香(mg) | -0.013 | 1.00 | 15.00 |
| 藏红花(g) | 0.032 | 13.35 | 3.71 |
| 姜黄(mg) | -0.785 | 533.60 | 754.30 |
| 绿/红茶(g) | -0.536 | 1.69 | 1.53 |
| 酒精(g) | -0.278 | 13.98 | 3.72 |
| 咖啡因(g) | -0.110 | 8.05 | 6.67 |
| 食物组 | 多样性模式 | 鱼虾豆类模式 | 牛奶蛋类模式 | 加工食品模式 |
|---|---|---|---|---|
| 谷类 | 0.454 | |||
| 肉类 | 0.622 | |||
| 菌藻类 | 0.581 | |||
| 加工食品 | 0.307 | 0.834 | ||
| 薯类 | 0.468 | |||
| 蔬菜 | 0.619 | |||
| 水果 | 0.544 | 0.312 | ||
| 蛋类 | 0.390 | 0.418 | ||
| 鱼虾 | 0.486 | 0.345 | ||
| 大豆 | 0.491 | 0.326 | ||
| 坚果 | 0.467 | |||
| 牛奶 | 0.318 | 0.592 |
表2 各食物因子载荷值
Table 2 Loading value of each food factor
| 食物组 | 多样性模式 | 鱼虾豆类模式 | 牛奶蛋类模式 | 加工食品模式 |
|---|---|---|---|---|
| 谷类 | 0.454 | |||
| 肉类 | 0.622 | |||
| 菌藻类 | 0.581 | |||
| 加工食品 | 0.307 | 0.834 | ||
| 薯类 | 0.468 | |||
| 蔬菜 | 0.619 | |||
| 水果 | 0.544 | 0.312 | ||
| 蛋类 | 0.390 | 0.418 | ||
| 鱼虾 | 0.486 | 0.345 | ||
| 大豆 | 0.491 | 0.326 | ||
| 坚果 | 0.467 | |||
| 牛奶 | 0.318 | 0.592 |
| 组别 | 例数 | DII | 年龄(岁) | 孕前BMI (kg/m2) | 民族[例(%)] | 户籍[例(%)] | |||
|---|---|---|---|---|---|---|---|---|---|
| 汉族 | 其他 | 农村 | 城镇 | ||||||
| T1组 | 217 | -1.95±1.10 | 30.7±4.1 | 24.0±4.4 | 202(93.1) | 15(6.9) | 68(31.3) | 149(68.7) | |
| T2组 | 218 | 0.66±0.59 | 30.6±4.2 | 23.9±4.5 | 198(90.8) | 20(9.2) | 88(40.4) | 130(59.6) | |
| T3组 | 218 | 2.37±0.47 | 30.6±4.4 | 23.3±4.4 | 197(90.4) | 21(9.6) | 92(42.2) | 126(57.8) | |
| χ2(F)值 | 1 729.554a | 0.020a | 1.279a | 1.176 | 6.243 | ||||
| P值 | <0.001 | 0.980 | 0.245 | 0.555 | 0.044 | ||||
| 组别 | 文化程度[例(%)] | 家庭年总收入[例(%)] | |||||||
| 初中及以下 | 高中/中专 | 大专/职大 | 本科及以上 | ≤4.9万元 | 5.0万元~9.9万元 | 10.0万元~19.9万元 | ≥20.0万元 | ||
| T1组 | 11(5.1) | 34(15.7) | 59(27.2) | 113(52.1) | 55(25.3) | 88(40.6) | 54(24.9) | 20(9.2) | |
| T2组 | 20(9.2) | 31(14.2) | 61(28.0) | 106(48.6) | 45(20.6) | 92(42.2) | 61(28.0) | 20(9.2) | |
| T3组 | 26(11.9) | 34(15.6) | 64(29.4) | 94(43.1) | 78(35.8) | 71(32.6) | 60(27.5) | 9(4.1) | |
| χ2(F)值 | 8.162 | 18.031 | |||||||
| P值 | 0.226 | 0.006 | |||||||
| 组别 | 在职[例(%)] | 不良孕产史[例(%)] | 吸烟[例(%)] | 饮酒[例(%)] | 锻炼[例(%)] | 膳食模式[例(%)] | |||
| 多样性模式 | 鱼虾豆类模式 | 牛奶蛋类模式 | 加工食品模式 | ||||||
| T1组 | 120(55.3) | 70(32.3) | 3(1.4) | 25(11.5) | 155(71.4) | 144(66.4) | 17(7.8) | 30(13.8) | 26(12.0) |
| T2组 | 116(53.2) | 72(33.0) | 9(4.1) | 24(11.0) | 152(69.7) | 20(9.2) | 80(36.7) | 63(28.9) | 55(25.2) |
| T3组 | 130(59.6) | 70(32.1) | 4(1.8) | 19(8.7) | 132(60.6) | 0 | 128(58.7) | 51(23.4) | 39(17.9) |
| χ2(F)值 | 1.899 | 0.048 | 3.949 | 1.042 | 6.767 | 327.877 | |||
| P值 | 0.387 | 0.976 | 0.139 | 0.594 | 0.034 | <0.001 | |||
表3 不同DII孕妇的基本信息比较
Table 3 Comparison of basic information in different DII pregnant women
| 组别 | 例数 | DII | 年龄(岁) | 孕前BMI (kg/m2) | 民族[例(%)] | 户籍[例(%)] | |||
|---|---|---|---|---|---|---|---|---|---|
| 汉族 | 其他 | 农村 | 城镇 | ||||||
| T1组 | 217 | -1.95±1.10 | 30.7±4.1 | 24.0±4.4 | 202(93.1) | 15(6.9) | 68(31.3) | 149(68.7) | |
| T2组 | 218 | 0.66±0.59 | 30.6±4.2 | 23.9±4.5 | 198(90.8) | 20(9.2) | 88(40.4) | 130(59.6) | |
| T3组 | 218 | 2.37±0.47 | 30.6±4.4 | 23.3±4.4 | 197(90.4) | 21(9.6) | 92(42.2) | 126(57.8) | |
| χ2(F)值 | 1 729.554a | 0.020a | 1.279a | 1.176 | 6.243 | ||||
| P值 | <0.001 | 0.980 | 0.245 | 0.555 | 0.044 | ||||
| 组别 | 文化程度[例(%)] | 家庭年总收入[例(%)] | |||||||
| 初中及以下 | 高中/中专 | 大专/职大 | 本科及以上 | ≤4.9万元 | 5.0万元~9.9万元 | 10.0万元~19.9万元 | ≥20.0万元 | ||
| T1组 | 11(5.1) | 34(15.7) | 59(27.2) | 113(52.1) | 55(25.3) | 88(40.6) | 54(24.9) | 20(9.2) | |
| T2组 | 20(9.2) | 31(14.2) | 61(28.0) | 106(48.6) | 45(20.6) | 92(42.2) | 61(28.0) | 20(9.2) | |
| T3组 | 26(11.9) | 34(15.6) | 64(29.4) | 94(43.1) | 78(35.8) | 71(32.6) | 60(27.5) | 9(4.1) | |
| χ2(F)值 | 8.162 | 18.031 | |||||||
| P值 | 0.226 | 0.006 | |||||||
| 组别 | 在职[例(%)] | 不良孕产史[例(%)] | 吸烟[例(%)] | 饮酒[例(%)] | 锻炼[例(%)] | 膳食模式[例(%)] | |||
| 多样性模式 | 鱼虾豆类模式 | 牛奶蛋类模式 | 加工食品模式 | ||||||
| T1组 | 120(55.3) | 70(32.3) | 3(1.4) | 25(11.5) | 155(71.4) | 144(66.4) | 17(7.8) | 30(13.8) | 26(12.0) |
| T2组 | 116(53.2) | 72(33.0) | 9(4.1) | 24(11.0) | 152(69.7) | 20(9.2) | 80(36.7) | 63(28.9) | 55(25.2) |
| T3组 | 130(59.6) | 70(32.1) | 4(1.8) | 19(8.7) | 132(60.6) | 0 | 128(58.7) | 51(23.4) | 39(17.9) |
| χ2(F)值 | 1.899 | 0.048 | 3.949 | 1.042 | 6.767 | 327.877 | |||
| P值 | 0.387 | 0.976 | 0.139 | 0.594 | 0.034 | <0.001 | |||
| 分类 | 例数 | DII | 年龄(岁) | 孕前BMI (kg/m2) | 民族[例(%)] | 户籍[例(%)] | 文化程度[例(%)] | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 汉族 | 其他 | 农村 | 城镇 | 初中及以下 | 高中/中专 | 大专/职大 | 本科及以上 | |||||
| 贫血 | 172 | 0.64±1.95 | 30.5±4.3 | 22.6±3.8 | 154(89.5) | 18(10.5) | 70(40.7) | 102(59.3) | 18(10.5) | 21(12.2) | 43(25.0) | 90(52.3) |
| 非贫血 | 481 | 0.26±1.92 | 30.7±4.2 | 24.1±4.6 | 443(92.1) | 38(7.9) | 178(37.0) | 303(63.0) | 39(8.1) | 78(16.2) | 141(29.3) | 223(46.4) |
| χ2(t)值 | -2.236a | 0.543a | 3.687a | 1.063 | 0.733 | 3.925 | ||||||
| P值 | 0.026 | 0.588 | <0.001 | 0.303 | 0.392 | 0.270 | ||||||
| 分类 | 家庭年总收入[例(%)] | 在职[例(%)] | 不良孕产史[例(%)] | 吸烟[例(%)] | 饮酒[例(%)] | 锻炼[例(%)] | ||||||
| ≤4.9万元 | 5.0万元~9.9万元 | 10.0万元~19.9万元 | ≥20.0万元 | |||||||||
| 贫血 | 45(26.2) | 73(42.4) | 44(25.6) | 10(5.8) | 101(58.7) | 51(29.7) | 5(2.9) | 15(8.7) | 117(68.0) | |||
| 非贫血 | 133(27.7) | 178(37.0) | 131(27.2) | 39(8.1) | 265(55.1) | 161(33.5) | 11(2.3) | 53(11.0) | 322(66.9) | |||
| χ2(t)值 | 2.095 | 0.677 | 0.844 | 0.204 | 0.717 | 0.067 | ||||||
| P值 | 0.553 | 0.411 | 0.358 | 0.652 | 0.397 | 0.796 | ||||||
表4 贫血和非贫血者基本信息比较
Table 4 Comparison of basic information on anemic and non-anemic pregnant women
| 分类 | 例数 | DII | 年龄(岁) | 孕前BMI (kg/m2) | 民族[例(%)] | 户籍[例(%)] | 文化程度[例(%)] | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 汉族 | 其他 | 农村 | 城镇 | 初中及以下 | 高中/中专 | 大专/职大 | 本科及以上 | |||||
| 贫血 | 172 | 0.64±1.95 | 30.5±4.3 | 22.6±3.8 | 154(89.5) | 18(10.5) | 70(40.7) | 102(59.3) | 18(10.5) | 21(12.2) | 43(25.0) | 90(52.3) |
| 非贫血 | 481 | 0.26±1.92 | 30.7±4.2 | 24.1±4.6 | 443(92.1) | 38(7.9) | 178(37.0) | 303(63.0) | 39(8.1) | 78(16.2) | 141(29.3) | 223(46.4) |
| χ2(t)值 | -2.236a | 0.543a | 3.687a | 1.063 | 0.733 | 3.925 | ||||||
| P值 | 0.026 | 0.588 | <0.001 | 0.303 | 0.392 | 0.270 | ||||||
| 分类 | 家庭年总收入[例(%)] | 在职[例(%)] | 不良孕产史[例(%)] | 吸烟[例(%)] | 饮酒[例(%)] | 锻炼[例(%)] | ||||||
| ≤4.9万元 | 5.0万元~9.9万元 | 10.0万元~19.9万元 | ≥20.0万元 | |||||||||
| 贫血 | 45(26.2) | 73(42.4) | 44(25.6) | 10(5.8) | 101(58.7) | 51(29.7) | 5(2.9) | 15(8.7) | 117(68.0) | |||
| 非贫血 | 133(27.7) | 178(37.0) | 131(27.2) | 39(8.1) | 265(55.1) | 161(33.5) | 11(2.3) | 53(11.0) | 322(66.9) | |||
| χ2(t)值 | 2.095 | 0.677 | 0.844 | 0.204 | 0.717 | 0.067 | ||||||
| P值 | 0.553 | 0.411 | 0.358 | 0.652 | 0.397 | 0.796 | ||||||
| 自变量 | 赋值 |
|---|---|
| 民族 | 汉族=1,其他=2 |
| 文化程度 | 初中及以下=1,高中/中专=2,大专/职大=3,本科及以上=4 |
| 户籍 | 农村=1,城镇=2 |
| 家庭年总收入 | ≤4.9万元=1,5.0万元~9.9万元=2,10.0万元~19.9万元=3,≤20.0万元=4 |
| 是否锻炼 | 否=0,是=1 |
| 主要膳食模式 | 多样性模式=1,鱼虾豆类模式=2,牛奶蛋类模式=3,加工食品模式=4 |
表5 DII与妊娠期贫血发病风险关联的Logistic回归分析中二分类变量的赋值情况
Table 5 The assignment of values for binary variables in Logistic regression analysis of association between DII and risk of developing anemia in pregnancy
| 自变量 | 赋值 |
|---|---|
| 民族 | 汉族=1,其他=2 |
| 文化程度 | 初中及以下=1,高中/中专=2,大专/职大=3,本科及以上=4 |
| 户籍 | 农村=1,城镇=2 |
| 家庭年总收入 | ≤4.9万元=1,5.0万元~9.9万元=2,10.0万元~19.9万元=3,≤20.0万元=4 |
| 是否锻炼 | 否=0,是=1 |
| 主要膳食模式 | 多样性模式=1,鱼虾豆类模式=2,牛奶蛋类模式=3,加工食品模式=4 |
| 特征 | 模型1 | 模型2 | 模型3 | |||
|---|---|---|---|---|---|---|
| OR(95%CI) | P值 | OR(95%CI) | P值 | OR(95%CI) | P值 | |
| 总人群 | 1.11(1.01~1.22) | 0.026 | 1.10(1.00~1.21) | 0.041 | 1.21(1.05~1.39) | 0.009 |
| T1 | 1.00 | 1.00 | 1.00 | |||
| T2 | 0.99(0.63~1.57) | 0.980 | 0.99(0.62~1.56) | 0.954 | 1.29(0.71~2.33) | 0.401 |
| T3 | 2.01(1.32~3.08) | 0.001 | 1.95(1.27~2.99) | 0.002 | 3.05(1.62~5.75) | <0.001 |
| 多样性模式 | 1.03(0.78~1.34) | 0.848 | 1.01(0.77~1.33) | 0.920 | 0.98(0.75~1.30) | 0.915 |
| T1 | 1.00 | 1.00 | 1.00 | |||
| T2 | 1.00(0.34~2.95) | 1.000 | 0.99(0.33~2.95) | 0.988 | 0.94(0.31~2.87) | 0.911 |
| 鱼虾豆类模式 | 1.20(0.92~1.55) | 0.182 | 1.18(0.91~1.54) | 0.209 | 1.15(0.87~1.51) | 0.322 |
| T1 | 1.00 | 1.00 | 1.00 | |||
| T2 | 0.81(0.23~2.83) | 0.744 | 0.88(0.25~3.10) | 0.845 | 0.86(0.24~3.10) | 0.815 |
| T3 | 1.32(0.40~4.32) | 0.645 | 1.35(0.41~4.45) | 0.621 | 1.26(0.37~4.23) | 0.712 |
| 牛奶蛋类模式 | 1.44(1.08~1.93) | 0.015 | 1.41(1.05~1.90) | 0.023 | 1.48(1.06~2.07) | 0.022 |
| T1 | 1.00 | 1.00 | 1.00 | |||
| T2 | 2.57(0.68~9.75) | 0.165 | 2.72(0.70~10.53) | 0.147 | 3.81(0.82~17.59) | 0.087 |
| T3 | 6.83(1.83~25.43) | 0.004 | 6.05(1.59~23.00) | 0.008 | 7.69(1.67~35.45) | 0.009 |
| 加工食品模式 | 1.35(0.98~1.84) | 0.063 | 1.34(0.98~1.84) | 0.066 | 1.34(0.95~1.89) | 0.097 |
| T1 | 1.00 | 1.00 | 1.00 | |||
| T2 | 1.53(0.44~5.32) | 0.499 | 1.44(0.40~5.10) | 0.575 | 1.65(0.41~6.67) | 0.479 |
| T3 | 5.22(1.52~17.99) | 0.009 | 5.10(1.48~17.63) | 0.010 | 5.17(1.29~20.63) | 0.020 |
表6 DII与妊娠期贫血发病风险关联的Logistic回归分析
Table 6 Logistic regression analysis of association between DII and risk of developing anemia in pregnancy
| 特征 | 模型1 | 模型2 | 模型3 | |||
|---|---|---|---|---|---|---|
| OR(95%CI) | P值 | OR(95%CI) | P值 | OR(95%CI) | P值 | |
| 总人群 | 1.11(1.01~1.22) | 0.026 | 1.10(1.00~1.21) | 0.041 | 1.21(1.05~1.39) | 0.009 |
| T1 | 1.00 | 1.00 | 1.00 | |||
| T2 | 0.99(0.63~1.57) | 0.980 | 0.99(0.62~1.56) | 0.954 | 1.29(0.71~2.33) | 0.401 |
| T3 | 2.01(1.32~3.08) | 0.001 | 1.95(1.27~2.99) | 0.002 | 3.05(1.62~5.75) | <0.001 |
| 多样性模式 | 1.03(0.78~1.34) | 0.848 | 1.01(0.77~1.33) | 0.920 | 0.98(0.75~1.30) | 0.915 |
| T1 | 1.00 | 1.00 | 1.00 | |||
| T2 | 1.00(0.34~2.95) | 1.000 | 0.99(0.33~2.95) | 0.988 | 0.94(0.31~2.87) | 0.911 |
| 鱼虾豆类模式 | 1.20(0.92~1.55) | 0.182 | 1.18(0.91~1.54) | 0.209 | 1.15(0.87~1.51) | 0.322 |
| T1 | 1.00 | 1.00 | 1.00 | |||
| T2 | 0.81(0.23~2.83) | 0.744 | 0.88(0.25~3.10) | 0.845 | 0.86(0.24~3.10) | 0.815 |
| T3 | 1.32(0.40~4.32) | 0.645 | 1.35(0.41~4.45) | 0.621 | 1.26(0.37~4.23) | 0.712 |
| 牛奶蛋类模式 | 1.44(1.08~1.93) | 0.015 | 1.41(1.05~1.90) | 0.023 | 1.48(1.06~2.07) | 0.022 |
| T1 | 1.00 | 1.00 | 1.00 | |||
| T2 | 2.57(0.68~9.75) | 0.165 | 2.72(0.70~10.53) | 0.147 | 3.81(0.82~17.59) | 0.087 |
| T3 | 6.83(1.83~25.43) | 0.004 | 6.05(1.59~23.00) | 0.008 | 7.69(1.67~35.45) | 0.009 |
| 加工食品模式 | 1.35(0.98~1.84) | 0.063 | 1.34(0.98~1.84) | 0.066 | 1.34(0.95~1.89) | 0.097 |
| T1 | 1.00 | 1.00 | 1.00 | |||
| T2 | 1.53(0.44~5.32) | 0.499 | 1.44(0.40~5.10) | 0.575 | 1.65(0.41~6.67) | 0.479 |
| T3 | 5.22(1.52~17.99) | 0.009 | 5.10(1.48~17.63) | 0.010 | 5.17(1.29~20.63) | 0.020 |
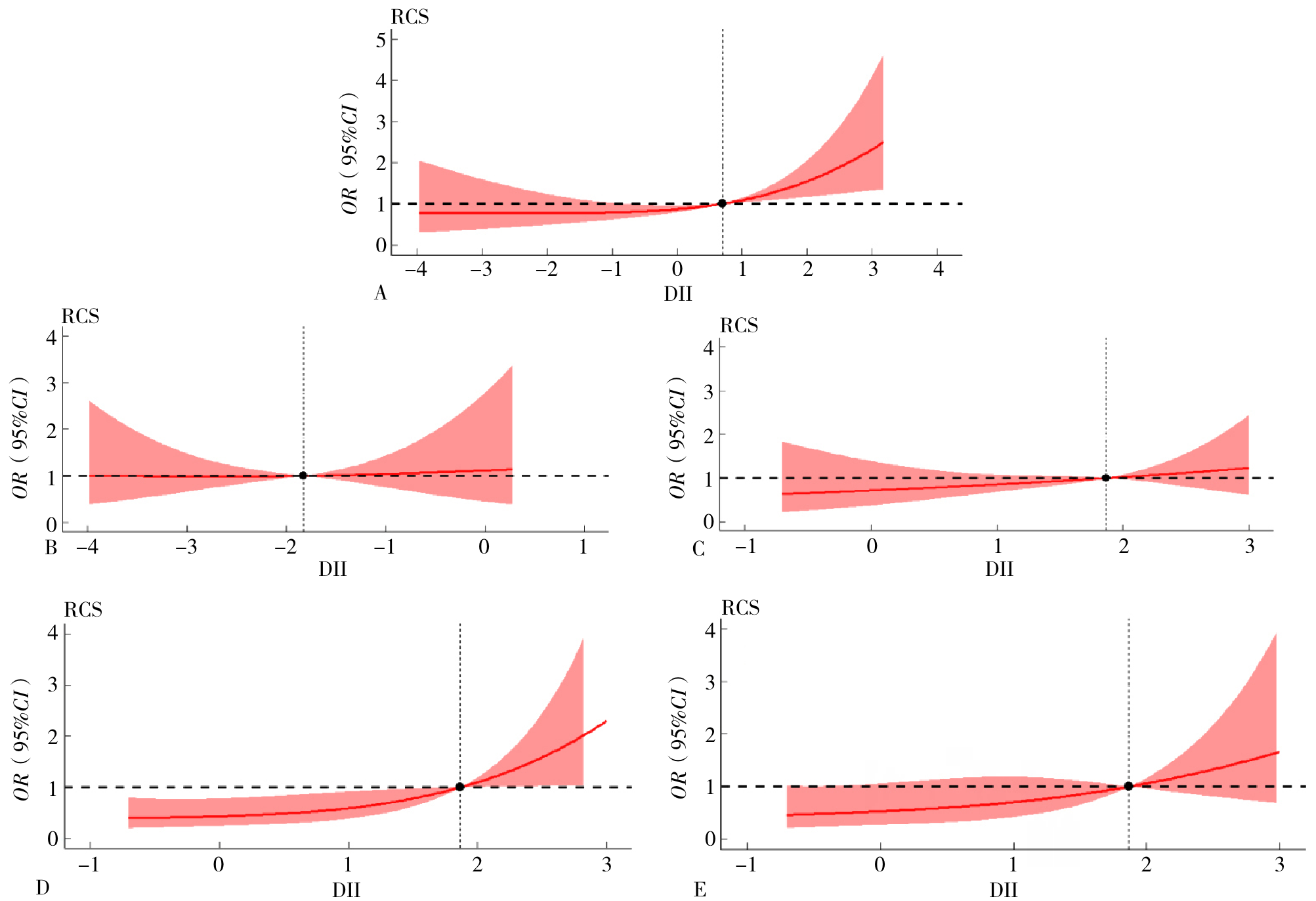
图2 DII与妊娠期贫血的发病风险关系注:A为总人群;B为多样性模式;C为鱼虾豆类模式;D为牛奶蛋类模式;E为加工食品模式。A调整了孕前BMI、年龄、民族、文化程度、户籍、家庭年总收入、锻炼及主要膳食模式;B~E调整了孕前BMI、年龄、民族、文化程度、户籍、家庭年总收入、锻炼;DII=膳食炎症指数。
Figure 2 Relationship between DII and risk of developing anemia in pregnancy
| 特征 | 例数 | 妊娠期贫血[例(%)] | DII[OR(95%CI)] | P 交互值 | ||
|---|---|---|---|---|---|---|
| T1组 | T2组 | T3组 | ||||
| 年龄 | 0.435 | |||||
| <35岁 | 525 | 134(25.5) | 1.00 | 1.71(0.86~3.41) | 3.87(1.85~8.11) | |
| ≥35岁 | 128 | 38(29.7) | 1.00 | 0.54(0.10~1.91) | 2.20(0.47~10.24) | |
| 孕前BMI(kg/m2) | 0.129 | |||||
| <18.5 kg/m2 | 51 | 20(39.2) | 1.00 | 0.57(0.02~13.52) | 0.83(0.04~19.49) | |
| 18.5~23.9 kg/m2 | 341 | 104(30.5) | 1.00 | 1.71(0.76~3.89) | 3.46(1.44~8.35) | |
| ≥24.0 kg/m2 | 261 | 48(18.4) | 1.00 | 1.12(0.38~3.34) | 4.50(1.40~14.48) | |
| 民族 | 0.854 | |||||
| 汉族 | 597 | 154(25.8) | 1.00 | 1.17(0.63~2.16) | 2.98(1.55~5.71) | |
| 其他 | 56 | 18(32.1) | 1.00 | 10.86(0.26~450.91) | 10.41(0.18~595.52) | |
| 户籍 | 0.751 | |||||
| 农村 | 248 | 70(28.2) | 1.00 | 1.44(0.51~4.10) | 2.12(0.68~6.54) | |
| 城镇 | 405 | 102(25.2) | 1.00 | 1.25(0.59~2.64) | 3.77(1.73~8.25) | |
| 锻炼 | 0.176 | |||||
| 是 | 439 | 117(26.7) | 1.00 | 1.60(0.79~3.21) | 3.97(1.82~8.66) | |
| 否 | 214 | 55(25.7) | 1.00 | 0.71(0.22~2.28) | 1.50(0.47~4.77) | |
表7 DII与妊娠期贫血发生风险关联的亚组分析
Table 7 Subgroup analysis of the association between DII and the risk of developing anemia in pregnancy
| 特征 | 例数 | 妊娠期贫血[例(%)] | DII[OR(95%CI)] | P 交互值 | ||
|---|---|---|---|---|---|---|
| T1组 | T2组 | T3组 | ||||
| 年龄 | 0.435 | |||||
| <35岁 | 525 | 134(25.5) | 1.00 | 1.71(0.86~3.41) | 3.87(1.85~8.11) | |
| ≥35岁 | 128 | 38(29.7) | 1.00 | 0.54(0.10~1.91) | 2.20(0.47~10.24) | |
| 孕前BMI(kg/m2) | 0.129 | |||||
| <18.5 kg/m2 | 51 | 20(39.2) | 1.00 | 0.57(0.02~13.52) | 0.83(0.04~19.49) | |
| 18.5~23.9 kg/m2 | 341 | 104(30.5) | 1.00 | 1.71(0.76~3.89) | 3.46(1.44~8.35) | |
| ≥24.0 kg/m2 | 261 | 48(18.4) | 1.00 | 1.12(0.38~3.34) | 4.50(1.40~14.48) | |
| 民族 | 0.854 | |||||
| 汉族 | 597 | 154(25.8) | 1.00 | 1.17(0.63~2.16) | 2.98(1.55~5.71) | |
| 其他 | 56 | 18(32.1) | 1.00 | 10.86(0.26~450.91) | 10.41(0.18~595.52) | |
| 户籍 | 0.751 | |||||
| 农村 | 248 | 70(28.2) | 1.00 | 1.44(0.51~4.10) | 2.12(0.68~6.54) | |
| 城镇 | 405 | 102(25.2) | 1.00 | 1.25(0.59~2.64) | 3.77(1.73~8.25) | |
| 锻炼 | 0.176 | |||||
| 是 | 439 | 117(26.7) | 1.00 | 1.60(0.79~3.21) | 3.97(1.82~8.66) | |
| 否 | 214 | 55(25.7) | 1.00 | 0.71(0.22~2.28) | 1.50(0.47~4.77) | |
| [1] |
|
| [2] |
Anaemia[EB/OL]. [2024-07-29].
|
| [3] |
|
| [4] |
|
| [5] |
Comprehensive implementation plan on maternal,infant and young child nutrition[EB/OL]. [2024-07-31].
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
姑丽切克然·艾斯克,开比努尔·再比布力,迪娜·木合亚提,等. 和田县农村居民膳食模式与炎症因子相关性研究[J]. 中国食物与营养,2023,29(5):81-84. DOI:10.19870/j.cnki.11-3716/ts.2023.05.001.
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
徐大凤,戴民慧,李甘,等. 东方膳食模式对2型糖尿病患者体重、血压、血糖、血脂影响的随机临床试验[J]. 公共卫生与预防医学,2024,35(4):28-31.
|
| [15] |
秦秋兰,周为文,李晓鹏,等. 广西成年居民膳食模式与代谢综合征的关系研究[J]. 应用预防医学,2024,30(4):226-230.
|
| [16] |
古丽菲热·居来提,张国珍. 伊犁哈萨克自治州农村居民膳食模式与代谢综合征相关性研究[J]. 中国预防医学杂志,2024,25(6):751-756. DOI:10.16506/j.1009-6639.2024.06.018.
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] | |
| [21] |
谢幸,孔北华,段涛. 《妇产科学》[M]. 9版. 北京:人民卫生出版社,2018.
|
| [22] |
《中国食物成分表》标准版第6版第一二册出版[J]. 营养学报,2019,41(5):426.
|
| [23] |
FoodData Central Search Results[EB/OL]. [2024-07-31].
|
| [24] |
|
| [25] |
覃钰婷,陆青贵,黄婕,等. 孕妇膳食炎性指数和白细胞介素6与出生体重的关系[J]. 卫生研究,2021,50(3):460-465. DOI:10.19813/j.cnki.weishengyanjiu.2021.03.019.
|
| [26] |
|
| [27] |
|
| [28] |
|
| [29] |
|
| [30] |
|
| [31] |
|
| [32] |
赵梅,于晓玲,王红菊,等. 孕中期膳食抗炎指数、高敏C反应蛋白与妊娠期糖尿病关系的队列研究[J]. 中华疾病控制杂志,2018,22(2):113-116. DOI:10.16462/j.cnki.zhjbkz.2018.02.003.
|
| [33] |
|
| [34] |
林秋琳. 安徽省淮北市孕妇孕晚期膳食结构分析及膳食炎症指数对低出生体重的影响[D]. 合肥:安徽医科大学,2023.
|
| [35] |
|
| [36] |
|
| [37] |
|
| [38] |
|
| [39] |
|
| [1] | 邵晓颖, 邵洁, 朱焱, 邵金玲, 尚灵, 吴振莲, 赵钰, 张加才. 贵州省6~36月龄儿童铁缺乏现状及缺铁性贫血影响因素研究[J]. 中国全科医学, 2025, 28(27): 3368-3374. |
| [2] | 郑传雷, 丁睿聪, 王琪, 郭逸星, 李剑, 黄争春, 董明华, 罗晓婷, 吴清锋. ≥35岁居民膳食模式与血脂异常相关性研究:基于赣南慢病队列调查数据[J]. 中国全科医学, 2024, 27(30): 3739-3745. |
| [3] | 胡桂萍, 林平, 赵振娟, 王旖旎, 鄢明强, 孙晓. 膳食炎症潜能与急性冠脉综合征患者冠状动脉病变严重程度的关系研究[J]. 中国全科医学, 2024, 27(24): 3000-3006. |
| [4] | 陈玟瑾, 陈飘盈, 杨晓华, 陈轶凡, 蔡业峰, 倪小佳. 膳食模式与脑血管疾病相关的流行病学研究新进展[J]. 中国全科医学, 2024, 27(08): 900-907. |
| [5] | 李纪新, 邱林杰, 任燕, 王文茹, 李美洁, 张晋. 膳食炎症指数与超重和肥胖及腹型肥胖关系的Meta分析[J]. 中国全科医学, 2023, 26(32): 4089-4097. |
| [6] | 翟蕾蕾, 赵书鹏, 姚萍. 膳食炎症指数与上消化道肿瘤风险关系的Meta分析[J]. 中国全科医学, 2023, 26(18): 2286-2292. |
| [7] | 王湾湾,李园园,石小天,马清. 营养对衰弱影响的研究进展[J]. 中国全科医学, 2021, 24(6): 673-677. |
| [8] | 李海霞,李向培,赵宵帝,王玲. 2型糖尿病患者血糖管理中的医学营养策略[J]. 中国全科医学, 2021, 24(13): 1702-1706. |
| [9] | 王佳,洪忠新,武力,丁冰杰,毕研霞,顾中一,李伟. 中老年人膳食模式与高血压发病机制探讨[J]. 中国全科医学, 2016, 19(14): 1706-1710. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





