中国全科医学 ›› 2025, Vol. 28 ›› Issue (36): 4566-4577.DOI: 10.12114/j.issn.1007-9572.2024.0521
所属专题: 心血管最新文章合辑
刘瑞越1,2, 杨雪梅3, 赵乃慧4, 温薪冉1,2, 蔡汐1,2, 梁雅靖1,2, 马佳佳1,2, 吴寿岭5, 崔刘福2,*( )
)
收稿日期:2024-11-04
修回日期:2025-06-30
出版日期:2025-12-20
发布日期:2025-12-04
通讯作者:
崔刘福
作者贡献:
刘瑞越负责论文起草,研究的实施,数据收集、采集、清洗和统计学分析、绘制图表;杨雪梅负责提出研究思路,设计研究方案,研究命题的提出、设计;赵乃慧、温薪冉、蔡汐、梁雅靖、马佳佳负责数据收集、采集、清洗;吴寿岭、崔刘福负责文章的质量控制与审查,对文章整体负责,监督管理。
LIU Ruiyue1,2, YANG Xuemei3, ZHAO Naihui4, WEN Xinran1,2, CAI Xi1,2, LIANG Yajing1,2, MA Jiajia1,2, WU Shouling5, CUI Liufu2,*( )
)
Received:2024-11-04
Revised:2025-06-30
Published:2025-12-20
Online:2025-12-04
Contact:
CUI Liufu
摘要: 背景 心血管疾病(CVD)是最常见的慢性非传染性疾病,其患病率在全球范围内呈上升趋势,也是世界上人口死亡的主要原因。超敏C反应蛋白(hs-CRP)与白蛋白(ALB)比值(CAR)是一种新型的炎症指标,既往本研究团队对其与CVD的关联进行了研究,发现高CAR与CVD发病风险增加密切相关。且目前已有研究报道了从中年人群(51~64岁)到老年人群(≥65岁),高水平的hs-CRP所致的CVD发病风险逐渐降低。然而,CAR作为评估CVD风险的新型指标,其对新发CVD的影响在不同年龄段人群中是否存在差异尚不明确。 目的 探讨不同年龄段CAR对新发CVD的影响。 方法 纳入参加开滦队列研究2010年度第3次体检的54 951例参与者为研究对象,收集参与者人口学与临床数据、体检资料与实验室检查指标。计算CAR并进行对数转化(lgCAR),依据lgCAR四分位数将研究对象分为Q1组(lgCAR<-4.34,n=13 744)、Q2组(-4.34≤lgCAR<-3.67,n=13 731)、Q3组(-3.67≤lgCAR<-2.83,n=13 736)、Q4组(lgCAR≥-2.83,n=13 740),并按年龄进行分层,即<40岁(n=9 617)、40~49岁(n=12 633)、50~59岁(n=17 740)和≥60岁(n=14 691)。以完成2010年度体检的时间为随访起点,以发生CVD、全因死亡和到达随访结束日期为随访终点对患者进行随访,随访截至2021-12-31。采用Kaplan-Meier方法计算总人群和各年龄段人群CVD累积发病率,并采用Log-rank检验进行组间比较。采用Cox比例风险回归分析不同CAR水平总人群发生CVD的风险。通过Cox比例风险回归模型探究年龄与CAR各分位数组间的乘法交互作用,并按年龄进行分层重复上述分析。为了消除服用药物对结果产生的影响,排除基线和随访时服用降压、降糖、降脂药物的研究对象后进行敏感性分析;为了消除反向因果关系和随访时间过短对结果造成的影响,排除随访时间<1年的研究对象后进行敏感性分析;由于CVD的死亡风险较高,CVD和患者死亡之间可能存在相互竞争,因此对60岁以上的参与者采用死亡竞争风险模型分析不同CAR水平对CVD的影响。 结果 最终纳入54 951例研究对象,其中男41 083例(74.8%),女13 868例(25.2%),研究对象平均年龄(51.7±12.8)岁,Q1~Q4组平均lgCAR分别为-5.6±1.5、-4.0±0.2、-3.3±0.2、-2.2±0.6。Q1~Q4组年龄、性别、接受高等教育、吸烟、饮酒、体育锻炼、BMI、hs-CRP、低密度脂蛋白胆固醇、高密度脂蛋白胆固醇、总胆固醇、收缩压、舒张压、糖尿病、高血压、服用降压药、服用降糖药、服用降脂药、估算肾小球滤过率、丙氨酸氨基转移酶、ALB、lgCAR比较,差异有统计学意义(P<0.05)。平均随访(10.38±1.99)年,随访期间共3 444例(6.27%)研究对象发生了CVD,Q1~Q4组新发CVD病例分别为659、809、901、1 075例;累积发病率分别为4.79%、5.89%、6.56%、7.82%,Log-rank结果表明,总人群与不同年龄段Q1~Q4组研究对象CVD的累积发病率差异有统计学意义(P<0.05)。Cox比例风险回归模型分析结果表明,在校正混杂因素后,Q4组人群新发CVD的风险是Q1组的1.20倍(HR=1.20,95%CI=1.07~1.35),年龄和CAR组与CVD存在交互作用(P交互=0.021)。在<40岁、40~49岁、50~59岁和≥60岁人群中Q4组新发CVD的风险分别为Q1组的1.13倍(HR=1.13,95%CI=0.55~2.33)、1.44倍(HR=1.44,95%CI=1.06~1.96)、1.24倍(HR=1.24,95%CI=1.02~1.50)和1.11倍(HR=1.11,95%CI=0.93~1.33)。敏感性分析结果显示,在排除基线和随访期间服用降脂药的人群中,年龄和CAR组与CVD存在交互作用(P交互=0.020),在排除基线和随访期间服用降糖药的人群中,年龄和CAR组与CVD存在交互作用(P交互=0.015),在排除随访时间<1年的人群中,年龄和CAR组与CVD存在交互作用(P交互=0.045);Cox比例风险回归模型分析结果与主结果保持一致,CAR分组与新发CVD的关联在中年人群(40~59岁)中依然存在,并且随着年龄的增长,CAR升高所导致的CVD发病风险降低。排除在基线和随访期间服用降压药的人群后,年龄和CAR组与CVD之间的交互作用不显著(P交互=0.114);Cox比例风险回归模型分析发现,与主结果相比,在50~59岁人群中,CAR分组与新发CVD的统计学关联无意义(P>0.05)。对≥60岁研究对象采用死亡竞争风险模型分析不同CAR水平对CVD的影响,结果与主结果保持一致,CAR与新发心血管事件无关联。 结论 高CAR水平是新发CVD的独立危险因素,CAR与CVD发病风险的关联在中年人群呈年龄依赖性,而随着年龄增加,高CAR所致的CVD发病风险呈下降趋势。
| 组别 | 例数 | 年龄(岁) | 性别(男/女) | 接受高等教育[例(%)] | 吸烟[例(%)] | 饮酒[例(%)] | 体育锻炼[例(%)] | BMI(kg/m2) | hs-CRP[M(P25,P75),mg/L] | LDL-C(mmol/L) | HDL-C(mmol/L) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1组 | 13 744 | 49.9±13.4 | 10 039/3 705 | 3 279(23.9) | 4 300(31.3) | 635(4.6) | 1 807(13.1) | 23.8±3.1 | 0.3(0.1,0.5) | 2.3±0.9 | 1.6±0.5 | ||
| Q2组 | 13 731 | 52.4±12.6 | 9 850/3 881 | 2 533(18.4) | 4 476(32.6) | 732(5.3) | 2 319(16.9) | 24.6±3.1 | 0.9(0.7,1.0) | 2.6±0.8 | 1.7±0.5 | ||
| Q3组 | 13 736 | 52.1±12.3 | 10 522/3 214 | 2 210(16.1) | 4 618(33.6) | 712(5.2) | 1 840(13.4) | 25.5±3.3 | 1.8(1.4,2.2) | 2.6±1.0 | 1.5±0.4 | ||
| Q4组 | 13 740 | 52.4±12.7 | 10 672/3 068 | 1 934(14.1) | 4 741(34.5) | 606(4.4) | 1 527(11.1) | 25.9±3.6 | 4.7(3.5,7.1) | 2.5±1.0 | 1.5±0.4 | ||
| 检验统计量值 | 125.58a | 174.45b | 495.66b | 35.72b | 17.24b | 201.06b | 1 155.63a | 51 340.37c | 237.46a | 630.80a | |||
| P值 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | |||
| 组别 | TC(mmol/L) | TG[M(P25,P75),mmol/L] | 收缩压(mmHg) | 舒张压(mmHg) | 糖尿病[例(%)] | 高血压[例(%)] | 服用降压药[例(%)] | 服用降糖药[例(%)] | 服用降脂药[例(%)] | eGFR[mL·min-1·(1.73 m2)-1] | ALT(U/L) | ALB(g/L) | lgCAR |
| Q1组 | 4.9±1.0 | 1.1(0.8,1.7) | 125±19 | 82±11 | 1 057(7.7) | 6 219(45.2) | 1 421(10.3) | 465(3.4) | 137(1.0) | 99.3±17.0 | 19.1±13.3 | 46.6±2.8 | -5.6±1.5 |
| Q2组 | 4.9±1.0 | 1.3(0.9,1.8) | 128±19 | 83±11 | 1 344(9.8) | 7 361(53.6) | 1 999(14.6) | 561(4.1) | 215(1.6) | 97.1±16.3 | 20.5±14.2 | 46.6±3.1 | -4.0±0.2 |
| Q3组 | 5.0±1.0 | 1.4(1.0,2.1) | 131±19 | 85±11 | 1 596(11.6) | 8 231(59.9) | 2 075(15.1) | 582(4.2) | 209(1.5) | 94.0±17.8 | 22.8±17.9 | 46.6±3.2 | -3.3±0.2 |
| Q4组 | 5.0±1.0 | 1.4(0.9,2.1) | 132±19 | 85±11 | 1 916(13.9) | 8 636(62.9) | 2 364(17.2) | 603(4.4) | 221(1.6) | 92.0±17.8 | 23.7±18.8 | 46.4±3.1 | -2.2±0.6 |
| 检验统计量值 | 66.70a | 1 266.77c | 331.12a | 295.96a | 304.03b | 1 013.67b | 278.58b | 21.09b | 24.11b | 487.64a | 237.17a | 12.50a | 44 981.90a |
| P值 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 |
表1 总人群中不同CAR分组的基线特征
Table 1 Baseline characteristics of different CAR groups in the total population
| 组别 | 例数 | 年龄(岁) | 性别(男/女) | 接受高等教育[例(%)] | 吸烟[例(%)] | 饮酒[例(%)] | 体育锻炼[例(%)] | BMI(kg/m2) | hs-CRP[M(P25,P75),mg/L] | LDL-C(mmol/L) | HDL-C(mmol/L) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1组 | 13 744 | 49.9±13.4 | 10 039/3 705 | 3 279(23.9) | 4 300(31.3) | 635(4.6) | 1 807(13.1) | 23.8±3.1 | 0.3(0.1,0.5) | 2.3±0.9 | 1.6±0.5 | ||
| Q2组 | 13 731 | 52.4±12.6 | 9 850/3 881 | 2 533(18.4) | 4 476(32.6) | 732(5.3) | 2 319(16.9) | 24.6±3.1 | 0.9(0.7,1.0) | 2.6±0.8 | 1.7±0.5 | ||
| Q3组 | 13 736 | 52.1±12.3 | 10 522/3 214 | 2 210(16.1) | 4 618(33.6) | 712(5.2) | 1 840(13.4) | 25.5±3.3 | 1.8(1.4,2.2) | 2.6±1.0 | 1.5±0.4 | ||
| Q4组 | 13 740 | 52.4±12.7 | 10 672/3 068 | 1 934(14.1) | 4 741(34.5) | 606(4.4) | 1 527(11.1) | 25.9±3.6 | 4.7(3.5,7.1) | 2.5±1.0 | 1.5±0.4 | ||
| 检验统计量值 | 125.58a | 174.45b | 495.66b | 35.72b | 17.24b | 201.06b | 1 155.63a | 51 340.37c | 237.46a | 630.80a | |||
| P值 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | |||
| 组别 | TC(mmol/L) | TG[M(P25,P75),mmol/L] | 收缩压(mmHg) | 舒张压(mmHg) | 糖尿病[例(%)] | 高血压[例(%)] | 服用降压药[例(%)] | 服用降糖药[例(%)] | 服用降脂药[例(%)] | eGFR[mL·min-1·(1.73 m2)-1] | ALT(U/L) | ALB(g/L) | lgCAR |
| Q1组 | 4.9±1.0 | 1.1(0.8,1.7) | 125±19 | 82±11 | 1 057(7.7) | 6 219(45.2) | 1 421(10.3) | 465(3.4) | 137(1.0) | 99.3±17.0 | 19.1±13.3 | 46.6±2.8 | -5.6±1.5 |
| Q2组 | 4.9±1.0 | 1.3(0.9,1.8) | 128±19 | 83±11 | 1 344(9.8) | 7 361(53.6) | 1 999(14.6) | 561(4.1) | 215(1.6) | 97.1±16.3 | 20.5±14.2 | 46.6±3.1 | -4.0±0.2 |
| Q3组 | 5.0±1.0 | 1.4(1.0,2.1) | 131±19 | 85±11 | 1 596(11.6) | 8 231(59.9) | 2 075(15.1) | 582(4.2) | 209(1.5) | 94.0±17.8 | 22.8±17.9 | 46.6±3.2 | -3.3±0.2 |
| Q4组 | 5.0±1.0 | 1.4(0.9,2.1) | 132±19 | 85±11 | 1 916(13.9) | 8 636(62.9) | 2 364(17.2) | 603(4.4) | 221(1.6) | 92.0±17.8 | 23.7±18.8 | 46.4±3.1 | -2.2±0.6 |
| 检验统计量值 | 66.70a | 1 266.77c | 331.12a | 295.96a | 304.03b | 1 013.67b | 278.58b | 21.09b | 24.11b | 487.64a | 237.17a | 12.50a | 44 981.90a |
| P值 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 |
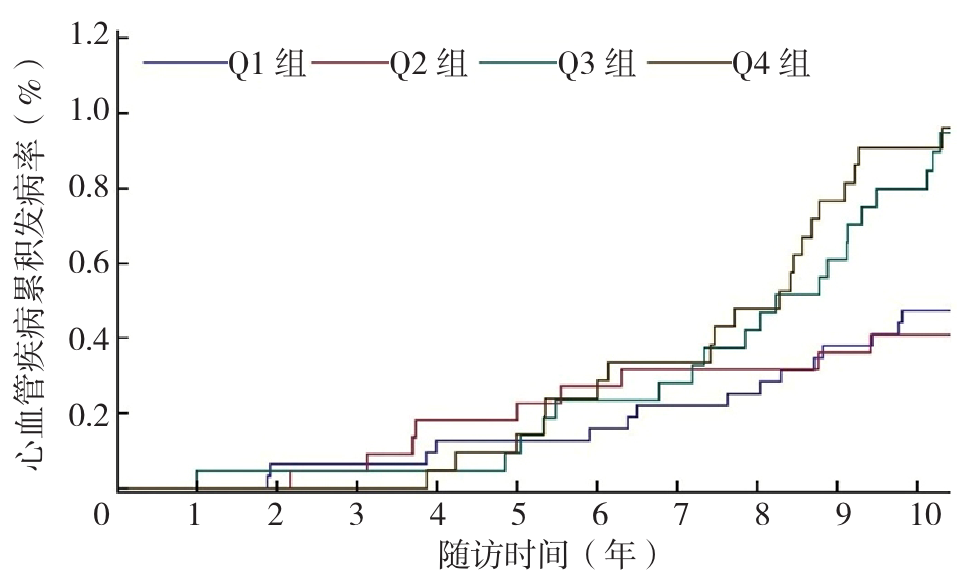
图3 <40岁人群不同CAR分组CVD累积发病率的Kaplan-Meier生存分析曲线
Figure 2 Kaplan-Meier survival analysis curves of cumulative incidence of CVD in different CAR groups in people under 40 years old
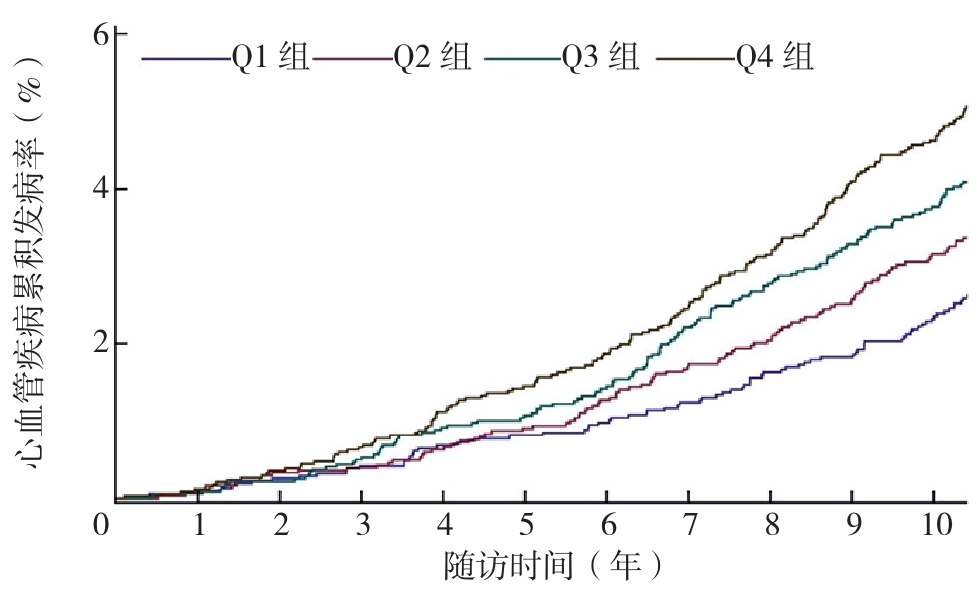
图4 40~49岁人群不同CAR分组CVD累积发病率的Kaplan-Meier生存分析曲线
Figure 4 Kaplan-Meier survival analysis curves of cumulative incidence of CVD in different CAR groups in people aged 40-49 years
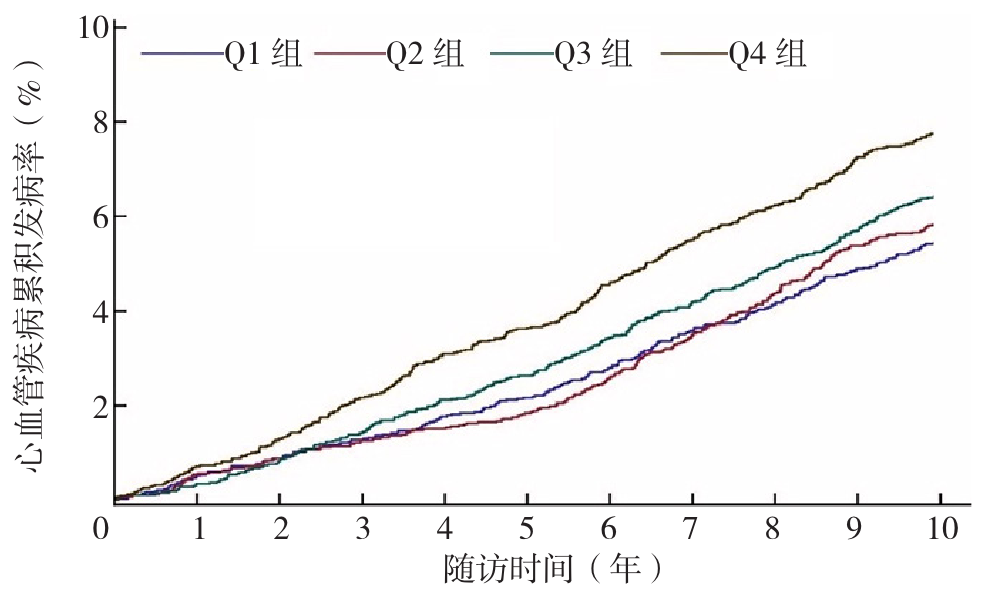
图5 50~59岁人群不同CAR分组CVD累积发病率的Kaplan-Meier生存分析曲线
Figure 5 Kaplan-Meier survival analysis curves of cumulative incidence of CVD in different CAR groups in people aged 50-59 years
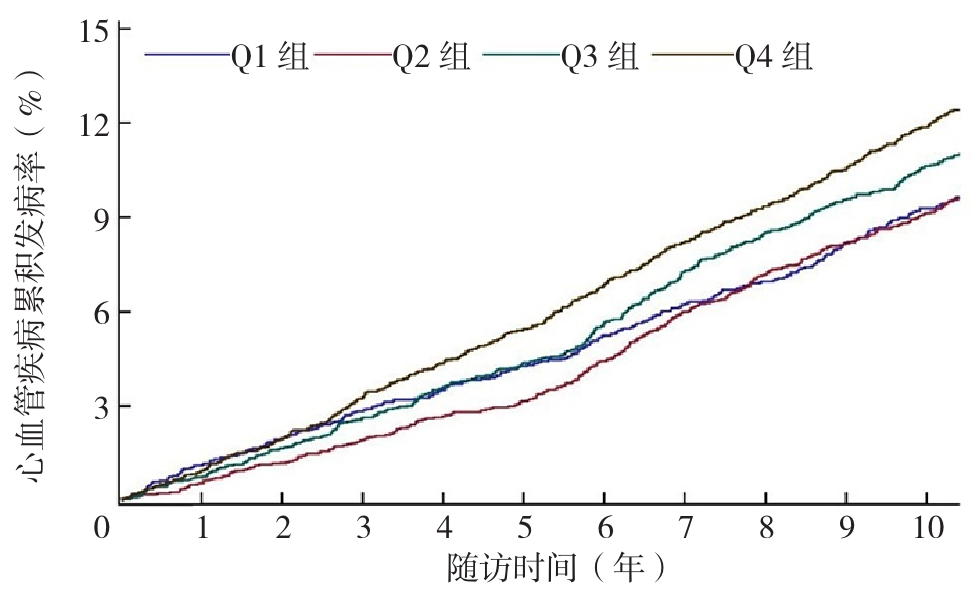
图6 ≥60岁人群不同CAR分组CVD累积发病率的Kaplan-Meier生存分析曲线
Figure 6 Kaplan-Meier survival analysis curves of cumulative incidence of CVD in people over 60 years old in different CAR groups
| 分组 | CVD发病人数(例) | 总人数(例) | 累积发病率(%) | 发病密度(例/千人年) |
|---|---|---|---|---|
| 总人群 | ||||
| Q1组 | 659 | 13 744 | 4.79 | 4.62 |
| Q2组 | 809 | 13 731 | 5.89 | 5.64 |
| Q3组 | 901 | 13 736 | 6.56 | 6.30 |
| Q4组 | 1 075 | 13 740 | 7.82 | 7.60 |
| <40岁 | ||||
| Q1组 | 17 | 3 168 | 0.54 | 0.50 |
| Q2组 | 10 | 2 212 | 0.45 | 0.41 |
| Q3组 | 25 | 2 143 | 1.17 | 1.06 |
| Q4组 | 29 | 2 094 | 1.38 | 1.25 |
| 40~49岁 | ||||
| Q1组 | 88 | 3 084 | 2.85 | 2.64 |
| Q2组 | 115 | 3 016 | 3.81 | 3.52 |
| Q3组 | 146 | 3 196 | 4.57 | 4.21 |
| Q4组 | 195 | 3 337 | 5.84 | 5.40 |
| 50~59岁 | ||||
| Q1组 | 261 | 4 326 | 6.03 | 5.81 |
| Q2组 | 280 | 4 324 | 6.48 | 6.15 |
| Q3组 | 329 | 4 666 | 7.05 | 6.72 |
| Q4组 | 392 | 4 424 | 8.86 | 8.55 |
| ≥60岁 | ||||
| Q1组 | 293 | 3 166 | 9.25 | 9.74 |
| Q2组 | 404 | 4 179 | 9.67 | 9.87 |
| Q3组 | 401 | 3 731 | 10.75 | 11.23 |
| Q4组 | 459 | 3 885 | 11.81 | 12.68 |
表2 Q1~Q4组各年龄分层CVD的发病情况
Table 2 Incidence of CVD in each age stratum of Q1-Q4 groups
| 分组 | CVD发病人数(例) | 总人数(例) | 累积发病率(%) | 发病密度(例/千人年) |
|---|---|---|---|---|
| 总人群 | ||||
| Q1组 | 659 | 13 744 | 4.79 | 4.62 |
| Q2组 | 809 | 13 731 | 5.89 | 5.64 |
| Q3组 | 901 | 13 736 | 6.56 | 6.30 |
| Q4组 | 1 075 | 13 740 | 7.82 | 7.60 |
| <40岁 | ||||
| Q1组 | 17 | 3 168 | 0.54 | 0.50 |
| Q2组 | 10 | 2 212 | 0.45 | 0.41 |
| Q3组 | 25 | 2 143 | 1.17 | 1.06 |
| Q4组 | 29 | 2 094 | 1.38 | 1.25 |
| 40~49岁 | ||||
| Q1组 | 88 | 3 084 | 2.85 | 2.64 |
| Q2组 | 115 | 3 016 | 3.81 | 3.52 |
| Q3组 | 146 | 3 196 | 4.57 | 4.21 |
| Q4组 | 195 | 3 337 | 5.84 | 5.40 |
| 50~59岁 | ||||
| Q1组 | 261 | 4 326 | 6.03 | 5.81 |
| Q2组 | 280 | 4 324 | 6.48 | 6.15 |
| Q3组 | 329 | 4 666 | 7.05 | 6.72 |
| Q4组 | 392 | 4 424 | 8.86 | 8.55 |
| ≥60岁 | ||||
| Q1组 | 293 | 3 166 | 9.25 | 9.74 |
| Q2组 | 404 | 4 179 | 9.67 | 9.87 |
| Q3组 | 401 | 3 731 | 10.75 | 11.23 |
| Q4组 | 459 | 3 885 | 11.81 | 12.68 |
| 分组 | 模型1 | 模型2 | 模型3 | 模型4 | ||||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | |
| 总人群 | <0.01a | <0.01a | <0.01a | <0.01a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.11(1.00~1.23) | 0.04 | 1.05(0.94~1.16) | 0.38 | 1.04(0.94~1.15) | 0.45 | 1.04(0.93~1.15) | 0.51 |
| Q3组 | 1.26(1.14~1.39) | <0.01 | 1.11(1.00~1.23) | 0.03 | 1.11(1.00~1.23) | 0.04 | 1.10(0.99~1.22) | 0.07 |
| Q4组 | 1.49(1.35~1.64) | <0.01 | 1.27(1.15~1.40) | <0.01 | 1.26(1.15~1.40) | <0.01 | 1.20(1.07~1.35) | <0.01 |
| <40岁 | <0.01a | 0.08a | 0.06a | 0.35a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 0.64(0.28~1.43) | 0.27 | 0.57(0.25~1.28) | 0.17 | 0.56(0.25~1.26) | 0.16 | 0.55(0.24~1.23) | 0.14 |
| Q3组 | 1.65(0.89~3.07) | 0.11 | 1.31(0.70~2.46) | 0.39 | 1.36(0.72~2.55) | 0.33 | 1.28(0.68~2.42) | 0.44 |
| Q4组 | 1.92(1.05~3.51) | 0.03 | 1.44(0.77~2.69) | 0.25 | 1.47(0.79~2.75) | 0.22 | 1.13(0.55~2.33) | 0.74 |
| 40~49岁 | <0.01a | <0.01a | <0.01a | 0.03a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.29(0.98~1.70) | 0.07 | 1.21(0.92~1.60) | 0.17 | 1.21(0.92~1.60) | 0.17 | 1.21(0.91~1.60) | 0.18 |
| Q3组 | 1.42(1.09~1.85) | 0.01 | 1.22(0.93~1.59) | 0.14 | 1.23(0.94~1.61) | 0.12 | 1.22(0.93~1.60) | 0.14 |
| Q4组 | 1.76(1.36~2.26) | <0.01 | 1.45(1.12~1.87) | 0.01 | 1.47(1.14~1.91) | <0.01 | 1.44(1.06~1.96) | 0.02 |
| 50~59岁 | <0.01a | <0.01a | <0.01a | 0.04a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.13(0.95~1.33) | 0.16 | 1.06(0.90~1.26) | 0.48 | 1.06(0.90~1.26) | 0.49 | 1.06(0.90~1.26) | 0.49 |
| Q3组 | 1.17(0.99~1.38) | 0.05 | 1.04(0.88~1.22) | 0.67 | 1.03(0.88~1.22) | 0.68 | 1.03(0.87~1.22) | 0.72 |
| Q4组 | 1.48(1.27~1.73) | <0.01 | 1.27(1.08~1.49) | <0.01 | 1.26(1.08~1.48) | <0.01 | 1.24(1.02~1.50) | 0.03 |
| ≥60岁 | <0.01a | <0.01a | <0.01a | 0.13a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.03(0.89~1.20) | 0.70 | 0.99(0.85~1.15) | 0.91 | 0.98(0.85~1.14) | 0.82 | 0.98(0.84~1.13) | 0.73 |
| Q3组 | 1.19(1.02~1.38) | 0.02 | 1.11(0.95~1.29) | 0.18 | 1.10(0.95~1.28) | 0.20 | 1.08(0.93~1.26) | 0.33 |
| Q4组 | 1.33(1.15~1.54) | <0.01 | 1.21(1.05~1.41) | 0.01 | 1.20(1.03~1.39) | 0.01 | 1.11(0.93~1.33) | 0.24 |
表3 不同CAR分组总人群及不同年龄段人群CVD发生率的Cox比例风险回归模型分析结果
Table 3 Cox proportional hazards model analysis results of CVD incidence in the total population and different age groups in different CAR groups
| 分组 | 模型1 | 模型2 | 模型3 | 模型4 | ||||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | |
| 总人群 | <0.01a | <0.01a | <0.01a | <0.01a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.11(1.00~1.23) | 0.04 | 1.05(0.94~1.16) | 0.38 | 1.04(0.94~1.15) | 0.45 | 1.04(0.93~1.15) | 0.51 |
| Q3组 | 1.26(1.14~1.39) | <0.01 | 1.11(1.00~1.23) | 0.03 | 1.11(1.00~1.23) | 0.04 | 1.10(0.99~1.22) | 0.07 |
| Q4组 | 1.49(1.35~1.64) | <0.01 | 1.27(1.15~1.40) | <0.01 | 1.26(1.15~1.40) | <0.01 | 1.20(1.07~1.35) | <0.01 |
| <40岁 | <0.01a | 0.08a | 0.06a | 0.35a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 0.64(0.28~1.43) | 0.27 | 0.57(0.25~1.28) | 0.17 | 0.56(0.25~1.26) | 0.16 | 0.55(0.24~1.23) | 0.14 |
| Q3组 | 1.65(0.89~3.07) | 0.11 | 1.31(0.70~2.46) | 0.39 | 1.36(0.72~2.55) | 0.33 | 1.28(0.68~2.42) | 0.44 |
| Q4组 | 1.92(1.05~3.51) | 0.03 | 1.44(0.77~2.69) | 0.25 | 1.47(0.79~2.75) | 0.22 | 1.13(0.55~2.33) | 0.74 |
| 40~49岁 | <0.01a | <0.01a | <0.01a | 0.03a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.29(0.98~1.70) | 0.07 | 1.21(0.92~1.60) | 0.17 | 1.21(0.92~1.60) | 0.17 | 1.21(0.91~1.60) | 0.18 |
| Q3组 | 1.42(1.09~1.85) | 0.01 | 1.22(0.93~1.59) | 0.14 | 1.23(0.94~1.61) | 0.12 | 1.22(0.93~1.60) | 0.14 |
| Q4组 | 1.76(1.36~2.26) | <0.01 | 1.45(1.12~1.87) | 0.01 | 1.47(1.14~1.91) | <0.01 | 1.44(1.06~1.96) | 0.02 |
| 50~59岁 | <0.01a | <0.01a | <0.01a | 0.04a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.13(0.95~1.33) | 0.16 | 1.06(0.90~1.26) | 0.48 | 1.06(0.90~1.26) | 0.49 | 1.06(0.90~1.26) | 0.49 |
| Q3组 | 1.17(0.99~1.38) | 0.05 | 1.04(0.88~1.22) | 0.67 | 1.03(0.88~1.22) | 0.68 | 1.03(0.87~1.22) | 0.72 |
| Q4组 | 1.48(1.27~1.73) | <0.01 | 1.27(1.08~1.49) | <0.01 | 1.26(1.08~1.48) | <0.01 | 1.24(1.02~1.50) | 0.03 |
| ≥60岁 | <0.01a | <0.01a | <0.01a | 0.13a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.03(0.89~1.20) | 0.70 | 0.99(0.85~1.15) | 0.91 | 0.98(0.85~1.14) | 0.82 | 0.98(0.84~1.13) | 0.73 |
| Q3组 | 1.19(1.02~1.38) | 0.02 | 1.11(0.95~1.29) | 0.18 | 1.10(0.95~1.28) | 0.20 | 1.08(0.93~1.26) | 0.33 |
| Q4组 | 1.33(1.15~1.54) | <0.01 | 1.21(1.05~1.41) | 0.01 | 1.20(1.03~1.39) | 0.01 | 1.11(0.93~1.33) | 0.24 |
| 分组 | 模型1 | 模型2 | 模型3 | 模型4 | ||||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | |
| 总人群 | <0.01a | <0.01a | <0.01a | <0.01a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.07(0.95~1.22) | 0.26 | 1.02(0.90~1.16) | 0.70 | 1.02(0.90~1.16) | 0.74 | 1.02(0.90~1.15) | 0.80 |
| Q3组 | 1.26(1.12~1.42) | <0.01 | 1.12(0.99~1.27) | 0.06 | 1.12(0.99~1.26) | 0.07 | 1.10(0.97~1.25) | 0.12 |
| Q4组 | 1.47(1.30~1.65) | <0.01 | 1.28(1.13~1.44) | <0.01 | 1.27(1.13~1.43) | <0.01 | 1.21(1.04~1.39) | 0.01 |
| <40岁 | 0.26a | 0.80a | 0.79a | 0.96a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 0.58(0.24~1.42) | 0.23 | 0.52(0.21~1.28) | 0.15 | 0.52(0.21~1.27) | 0.15 | 0.50(0.20~1.24) | 0.13 |
| Q3组 | 1.57(0.80~3.08) | 0.18 | 1.22(0.61~2.43) | 0.57 | 1.24(0.62~2.46) | 0.54 | 1.15(0.58~2.31) | 0.68 |
| Q4组 | 1.17(0.57~2.40) | 0.66 | 0.88(0.42~1.87) | 0.74 | 0.88(0.42~1.86) | 0.73 | 0.65(0.27~2.57) | 0.33 |
| 40~49岁 | <0.01a | <0.01a | <0.01a | 0.01a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.35(0.96~1.90) | 0.08 | 1.29(0.91~1.81) | 0.15 | 1.27(0.90~1.79) | 0.16 | 1.26(0.89~1.78) | 0.18 |
| Q3组 | 1.49(1.07~2.07) | 0.01 | 1.33(0.95~1.85) | 0.09 | 1.32(0.95~1.84) | 0.10 | 1.30(0.93~1.81) | 0.12 |
| Q4组 | 2.01(1.47~2.73) | <0.01 | 1.73(1.26~2.37) | <0.01 | 1.73(1.26~2.37) | <0.01 | 1.62(1.12~2.34) | 0.01 |
| 50~59岁 | <0.01a | 0.05a | 0.07a | 0.22a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.00(0.82~1.23) | 0.96 | 0.96(0.78~1.18) | 0.71 | 0.96(0.78~1.18) | 0.69 | 0.97(0.79~1.19) | 0.75 |
| Q3组 | 1.05(0.86~1.27) | 0.65 | 0.94(0.77~1.14) | 0.51 | 0.93(0.76~1.14) | 0.48 | 0.94(0.77~1.15) | 0.53 |
| Q4组 | 1.39(1.15~1.68) | <0.01 | 1.22(1.00~1.47) | 0.04 | 1.21(0.99~1.46) | 0.05 | 1.23(0.97~1.57) | 0.08 |
| ≥60岁 | <0.01a | <0.01a | <0.01a | 0.13a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.05(0.87~1.25) | 0.63 | 1.01(0.84~1.21) | 0.92 | 1.00(0.84~1.20) | 0.97 | 0.99(0.83~1.19) | 0.95 |
| Q3组 | 1.29(1.08~1.54) | 0.01 | 1.19(0.99~1.43) | 0.06 | 1.18(0.99~1.42) | 0.06 | 1.16(0.96~1.39) | 0.11 |
| Q4组 | 1.34(1.12~1.60) | <0.01 | 1.22(0.02~1.47) | 0.02 | 1.21(1.01~1.46) | 0.03 | 1.12(0.90~1.39) | 0.31 |
表4 排除服用降压药研究对象后不同CAR分组总人群及不同年龄段人群CVD发生率的Cox比例风险回归模型分析结果
Table 4 Results of Cox proportional hazards model analysis on the incidence of cvd in different car groups and different age groups after excluding study subjects taking antihypertensive medications
| 分组 | 模型1 | 模型2 | 模型3 | 模型4 | ||||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | |
| 总人群 | <0.01a | <0.01a | <0.01a | <0.01a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.07(0.95~1.22) | 0.26 | 1.02(0.90~1.16) | 0.70 | 1.02(0.90~1.16) | 0.74 | 1.02(0.90~1.15) | 0.80 |
| Q3组 | 1.26(1.12~1.42) | <0.01 | 1.12(0.99~1.27) | 0.06 | 1.12(0.99~1.26) | 0.07 | 1.10(0.97~1.25) | 0.12 |
| Q4组 | 1.47(1.30~1.65) | <0.01 | 1.28(1.13~1.44) | <0.01 | 1.27(1.13~1.43) | <0.01 | 1.21(1.04~1.39) | 0.01 |
| <40岁 | 0.26a | 0.80a | 0.79a | 0.96a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 0.58(0.24~1.42) | 0.23 | 0.52(0.21~1.28) | 0.15 | 0.52(0.21~1.27) | 0.15 | 0.50(0.20~1.24) | 0.13 |
| Q3组 | 1.57(0.80~3.08) | 0.18 | 1.22(0.61~2.43) | 0.57 | 1.24(0.62~2.46) | 0.54 | 1.15(0.58~2.31) | 0.68 |
| Q4组 | 1.17(0.57~2.40) | 0.66 | 0.88(0.42~1.87) | 0.74 | 0.88(0.42~1.86) | 0.73 | 0.65(0.27~2.57) | 0.33 |
| 40~49岁 | <0.01a | <0.01a | <0.01a | 0.01a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.35(0.96~1.90) | 0.08 | 1.29(0.91~1.81) | 0.15 | 1.27(0.90~1.79) | 0.16 | 1.26(0.89~1.78) | 0.18 |
| Q3组 | 1.49(1.07~2.07) | 0.01 | 1.33(0.95~1.85) | 0.09 | 1.32(0.95~1.84) | 0.10 | 1.30(0.93~1.81) | 0.12 |
| Q4组 | 2.01(1.47~2.73) | <0.01 | 1.73(1.26~2.37) | <0.01 | 1.73(1.26~2.37) | <0.01 | 1.62(1.12~2.34) | 0.01 |
| 50~59岁 | <0.01a | 0.05a | 0.07a | 0.22a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.00(0.82~1.23) | 0.96 | 0.96(0.78~1.18) | 0.71 | 0.96(0.78~1.18) | 0.69 | 0.97(0.79~1.19) | 0.75 |
| Q3组 | 1.05(0.86~1.27) | 0.65 | 0.94(0.77~1.14) | 0.51 | 0.93(0.76~1.14) | 0.48 | 0.94(0.77~1.15) | 0.53 |
| Q4组 | 1.39(1.15~1.68) | <0.01 | 1.22(1.00~1.47) | 0.04 | 1.21(0.99~1.46) | 0.05 | 1.23(0.97~1.57) | 0.08 |
| ≥60岁 | <0.01a | <0.01a | <0.01a | 0.13a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.05(0.87~1.25) | 0.63 | 1.01(0.84~1.21) | 0.92 | 1.00(0.84~1.20) | 0.97 | 0.99(0.83~1.19) | 0.95 |
| Q3组 | 1.29(1.08~1.54) | 0.01 | 1.19(0.99~1.43) | 0.06 | 1.18(0.99~1.42) | 0.06 | 1.16(0.96~1.39) | 0.11 |
| Q4组 | 1.34(1.12~1.60) | <0.01 | 1.22(0.02~1.47) | 0.02 | 1.21(1.01~1.46) | 0.03 | 1.12(0.90~1.39) | 0.31 |
| 分组 | 模型1 | 模型2 | 模型3 | 模型4 | ||||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | |
| 总人群 | <0.01a | <0.01a | <0.01a | <0.01a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.09(0.99~1.22) | 0.09 | 1.03(0.93~1.14) | 0.58 | 1.02(0.92~1.14) | 0.67 | 1.02(0.92~1.13) | 0.74 |
| Q3组 | 1.25(1.13~1.39) | <0.01 | 1.10(1.00~1.22) | 0.06 | 1.10(0.99~1.22) | 0.06 | 1.09(0.98~1.21) | 0.12 |
| Q4组 | 1.48(1.34~1.63) | <0.01 | 1.27(1.15~1.40) | <0.01 | 1.26(1.14~1.39) | <0.01 | 1.19(1.06~1.34) | <0.01 |
| <40岁 | <0.01a | 0.09a | 0.07a | 0.40a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 0.57(0.25~1.32) | 0.18 | 0.51(0.22~1.17) | 0.11 | 0.50(0.21~1.15) | 0.10 | 0.48(0.21~1.12) | 0.09 |
| Q3组 | 1.60(0.86~2.98) | 0.14 | 1.26(0.67~2.38) | 0.47 | 1.30(0.69~2.46) | 0.41 | 1.22(0.65~2.32) | 0.53 |
| Q4组 | 1.87(1.02~3.43) | 0.04 | 1.39(0.74~2.61) | 0.30 | 1.42(0.75~2.66) | 0.28 | 1.08(0.52~2.24) | 0.83 |
| 40~49岁 | <0.01a | <0.01a | <0.01a | 0.04a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.34(1.01~1.78) | 0.04 | 1.26(0.95~1.68) | 0.10 | 1.26(0.95~1.67) | 0.11 | 1.25(0.94~1.66) | 0.12 |
| Q3组 | 1.45(1.11~1.91) | 0.01 | 1.25(0.95~1.65) | 0.11 | 1.26(0.96~1.66) | 0.10 | 1.24(0.94~1.64) | 0.12 |
| Q4组 | 1.77(1.36~2.30) | <0.01 | 1.47(1.12~1.91) | 0.01 | 1.49(1.14~1.95) | <0.01 | 1.43(1.04~1.96) | 0.02 |
| 50~59岁 | <0.01a | <0.01a | <0.01a | 0.04a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.12(0.94~1.33) | 0.21 | 1.05(0.89~1.25) | 0.55 | 1.05(0.89~1.25) | 0.55 | 1.05(0.89~1.25) | 0.55 |
| Q3组 | 1.18(0.99~1.39) | 0.05 | 1.04(0.88~1.23) | 0.63 | 1.04(0.88~1.23) | 0.63 | 1.04(0.88~1.23) | 0.64 |
| Q4组 | 1.49(1.27~1.74) | <0.01 | 1.27(1.08~1.50) | <0.01 | 1.27(1.08~1.49) | <0.01 | 1.26(1.03~1.53) | 0.02 |
| ≥60岁 | <0.01a | <0.01a | <0.01a | 0.19a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.00(0.86~1.16) | 0.97 | 0.96(0.82~1.12) | 0.57 | 0.95(0.81~1.11) | 0.49 | 0.94(0.81~1.10) | 0.42 |
| Q3组 | 1.16(0.99~1.35) | 0.06 | 1.07(0.92~1.25) | 0.36 | 1.07(0.92~1.25) | 0.36 | 1.04(0.89~1.22) | 0.58 |
| Q4组 | 1.32(1.14~1.53) | <0.01 | 1.20(1.03~1.40) | 0.01 | 1.19(1.02~1.38) | 0.02 | 1.09(0.91~1.30) | 0.35 |
表5 排除服用降脂药研究对象后不同CAR分组总人群及不同年龄段人群CVD发生率的Cox比例风险回归模型分析结果
Table 5 Results of Cox proportional hazards model analysis on the incidence of cvd in different car groups and different age groups after excluding study subjects taking lipid-lowering medications
| 分组 | 模型1 | 模型2 | 模型3 | 模型4 | ||||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | |
| 总人群 | <0.01a | <0.01a | <0.01a | <0.01a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.09(0.99~1.22) | 0.09 | 1.03(0.93~1.14) | 0.58 | 1.02(0.92~1.14) | 0.67 | 1.02(0.92~1.13) | 0.74 |
| Q3组 | 1.25(1.13~1.39) | <0.01 | 1.10(1.00~1.22) | 0.06 | 1.10(0.99~1.22) | 0.06 | 1.09(0.98~1.21) | 0.12 |
| Q4组 | 1.48(1.34~1.63) | <0.01 | 1.27(1.15~1.40) | <0.01 | 1.26(1.14~1.39) | <0.01 | 1.19(1.06~1.34) | <0.01 |
| <40岁 | <0.01a | 0.09a | 0.07a | 0.40a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 0.57(0.25~1.32) | 0.18 | 0.51(0.22~1.17) | 0.11 | 0.50(0.21~1.15) | 0.10 | 0.48(0.21~1.12) | 0.09 |
| Q3组 | 1.60(0.86~2.98) | 0.14 | 1.26(0.67~2.38) | 0.47 | 1.30(0.69~2.46) | 0.41 | 1.22(0.65~2.32) | 0.53 |
| Q4组 | 1.87(1.02~3.43) | 0.04 | 1.39(0.74~2.61) | 0.30 | 1.42(0.75~2.66) | 0.28 | 1.08(0.52~2.24) | 0.83 |
| 40~49岁 | <0.01a | <0.01a | <0.01a | 0.04a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.34(1.01~1.78) | 0.04 | 1.26(0.95~1.68) | 0.10 | 1.26(0.95~1.67) | 0.11 | 1.25(0.94~1.66) | 0.12 |
| Q3组 | 1.45(1.11~1.91) | 0.01 | 1.25(0.95~1.65) | 0.11 | 1.26(0.96~1.66) | 0.10 | 1.24(0.94~1.64) | 0.12 |
| Q4组 | 1.77(1.36~2.30) | <0.01 | 1.47(1.12~1.91) | 0.01 | 1.49(1.14~1.95) | <0.01 | 1.43(1.04~1.96) | 0.02 |
| 50~59岁 | <0.01a | <0.01a | <0.01a | 0.04a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.12(0.94~1.33) | 0.21 | 1.05(0.89~1.25) | 0.55 | 1.05(0.89~1.25) | 0.55 | 1.05(0.89~1.25) | 0.55 |
| Q3组 | 1.18(0.99~1.39) | 0.05 | 1.04(0.88~1.23) | 0.63 | 1.04(0.88~1.23) | 0.63 | 1.04(0.88~1.23) | 0.64 |
| Q4组 | 1.49(1.27~1.74) | <0.01 | 1.27(1.08~1.50) | <0.01 | 1.27(1.08~1.49) | <0.01 | 1.26(1.03~1.53) | 0.02 |
| ≥60岁 | <0.01a | <0.01a | <0.01a | 0.19a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.00(0.86~1.16) | 0.97 | 0.96(0.82~1.12) | 0.57 | 0.95(0.81~1.11) | 0.49 | 0.94(0.81~1.10) | 0.42 |
| Q3组 | 1.16(0.99~1.35) | 0.06 | 1.07(0.92~1.25) | 0.36 | 1.07(0.92~1.25) | 0.36 | 1.04(0.89~1.22) | 0.58 |
| Q4组 | 1.32(1.14~1.53) | <0.01 | 1.20(1.03~1.40) | 0.01 | 1.19(1.02~1.38) | 0.02 | 1.09(0.91~1.30) | 0.35 |
| 分组 | 模型1 | 模型2 | 模型3 | 模型4 | ||||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | |
| 总人群 | <0.01a | <0.01a | <0.01a | <0.01a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.13(1.01~1.26) | 0.02 | 1.07(0.96~1.20) | 0.22 | 1.06(0.95~1.19) | 0.28 | 1.06(0.95~1.18) | 0.33 |
| Q3组 | 1.26(1.13~1.40) | <0.01 | 1.12(1.00~1.25) | 0.04 | 1.11(0.99~1.24) | 0.05 | 1.10(0.98~1.22) | 0.10 |
| Q4组 | 1.51(1.36~1.67) | <0.01 | 1.31(1.18~1.46) | <0.01 | 1.30(1.17~1.44) | <0.01 | 1.21(1.07~1.38) | <0.01 |
| <40岁 | 0.01a | 0.15a | 0.12a | 0.48a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 0.65(0.29~1.45) | 0.28 | 0.57(0.26~1.29) | 0.17 | 0.57(0.25~1.28) | 0.17 | 0.56(0.25~1.25) | 0.15 |
| Q3组 | 1.61(0.86~3.00) | 0.13 | 1.28(0.68~2.41) | 0.44 | 1.33(0.71~2.51) | 0.38 | 1.25(0.66~2.37) | 0.49 |
| Q4组 | 1.77(0.96~3.27) | 0.06 | 1.33(0.70~2.51) | 0.38 | 1.35(0.71~2.56) | 0.35 | 1.05(0.50~2.21) | 0.90 |
| 40~49岁 | <0.01a | <0.01a | <0.01a | 0.04a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.39(1.04~1.86) | 0.02 | 1.31(0.98~1.76) | 0.06 | 1.31(0.98~1.75) | 0.07 | 1.30(0.97~1.74) | 0.08 |
| Q3组 | 1.42(1.07~1.89) | 0.01 | 1.23(0.93~1.64) | 0.15 | 1.24(0.94~1.65) | 0.13 | 1.23(0.92~1.63) | 0.16 |
| Q4组 | 1.82(1.39~2.38) | <0.01 | 1.53(1.16~2.01) | <0.01 | 1.55(1.18~2.03) | <0.01 | 1.47(1.07~2.04) | 0.01 |
| 50~59岁 | <0.01a | <0.01a | <0.01a | 0.04a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.10(0.91~1.31) | 0.32 | 1.05(0.87~1.26) | 0.61 | 1.04(0.87~1.25) | 0.65 | 1.04(0.87~1.25) | 0.66 |
| Q3组 | 1.18(0.99~1.40) | 0.06 | 1.06(0.89~1.26) | 0.52 | 1.05(0.89~1.26) | 0.55 | 1.05(0.88~1.25) | 0.58 |
| Q4组 | 1.50(1.27~1.77) | <0.01 | 1.32(1.11~1.56) | <0.01 | 1.30(1.10~1.55) | <0.01 | 1.28(1.04~1.58) | 0.01 |
| ≥60岁 | <0.01a | <0.01a | <0.01a | 0.24a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.06(0.91~1.25) | 0.45 | 1.03(0.87~1.21) | 0.76 | 1.02(0.87~1.20) | 0.84 | 1.01(0.85~1.18) | 0.95 |
| Q3组 | 1.18(1.00~1.39) | 0.04 | 1.10(0.93~1.29) | 0.27 | 1.09(0.93~1.29) | 0.29 | 1.06(0.90~1.25) | 0.48 |
| Q4组 | 1.35(1.16~1.58) | <0.01 | 1.24(1.06~1.46) | 0.01 | 1.23(1.05~1.44) | 0.01 | 1.10(0.91~1.33) | 0.30 |
表6 排除服用降糖药研究对象后不同CAR分组总人群及不同年龄段人群CVD发生率的Cox比例风险回归模型分析结果
Table 6 Results of Cox proportional hazards model analysis on the incidence of cvd in different car groups and different age groups after excluding study subjects taking antidiabetic medications
| 分组 | 模型1 | 模型2 | 模型3 | 模型4 | ||||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | |
| 总人群 | <0.01a | <0.01a | <0.01a | <0.01a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.13(1.01~1.26) | 0.02 | 1.07(0.96~1.20) | 0.22 | 1.06(0.95~1.19) | 0.28 | 1.06(0.95~1.18) | 0.33 |
| Q3组 | 1.26(1.13~1.40) | <0.01 | 1.12(1.00~1.25) | 0.04 | 1.11(0.99~1.24) | 0.05 | 1.10(0.98~1.22) | 0.10 |
| Q4组 | 1.51(1.36~1.67) | <0.01 | 1.31(1.18~1.46) | <0.01 | 1.30(1.17~1.44) | <0.01 | 1.21(1.07~1.38) | <0.01 |
| <40岁 | 0.01a | 0.15a | 0.12a | 0.48a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 0.65(0.29~1.45) | 0.28 | 0.57(0.26~1.29) | 0.17 | 0.57(0.25~1.28) | 0.17 | 0.56(0.25~1.25) | 0.15 |
| Q3组 | 1.61(0.86~3.00) | 0.13 | 1.28(0.68~2.41) | 0.44 | 1.33(0.71~2.51) | 0.38 | 1.25(0.66~2.37) | 0.49 |
| Q4组 | 1.77(0.96~3.27) | 0.06 | 1.33(0.70~2.51) | 0.38 | 1.35(0.71~2.56) | 0.35 | 1.05(0.50~2.21) | 0.90 |
| 40~49岁 | <0.01a | <0.01a | <0.01a | 0.04a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.39(1.04~1.86) | 0.02 | 1.31(0.98~1.76) | 0.06 | 1.31(0.98~1.75) | 0.07 | 1.30(0.97~1.74) | 0.08 |
| Q3组 | 1.42(1.07~1.89) | 0.01 | 1.23(0.93~1.64) | 0.15 | 1.24(0.94~1.65) | 0.13 | 1.23(0.92~1.63) | 0.16 |
| Q4组 | 1.82(1.39~2.38) | <0.01 | 1.53(1.16~2.01) | <0.01 | 1.55(1.18~2.03) | <0.01 | 1.47(1.07~2.04) | 0.01 |
| 50~59岁 | <0.01a | <0.01a | <0.01a | 0.04a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.10(0.91~1.31) | 0.32 | 1.05(0.87~1.26) | 0.61 | 1.04(0.87~1.25) | 0.65 | 1.04(0.87~1.25) | 0.66 |
| Q3组 | 1.18(0.99~1.40) | 0.06 | 1.06(0.89~1.26) | 0.52 | 1.05(0.89~1.26) | 0.55 | 1.05(0.88~1.25) | 0.58 |
| Q4组 | 1.50(1.27~1.77) | <0.01 | 1.32(1.11~1.56) | <0.01 | 1.30(1.10~1.55) | <0.01 | 1.28(1.04~1.58) | 0.01 |
| ≥60岁 | <0.01a | <0.01a | <0.01a | 0.24a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.06(0.91~1.25) | 0.45 | 1.03(0.87~1.21) | 0.76 | 1.02(0.87~1.20) | 0.84 | 1.01(0.85~1.18) | 0.95 |
| Q3组 | 1.18(1.00~1.39) | 0.04 | 1.10(0.93~1.29) | 0.27 | 1.09(0.93~1.29) | 0.29 | 1.06(0.90~1.25) | 0.48 |
| Q4组 | 1.35(1.16~1.58) | <0.01 | 1.24(1.06~1.46) | 0.01 | 1.23(1.05~1.44) | 0.01 | 1.10(0.91~1.33) | 0.30 |
| 分组 | 模型1 | 模型2 | 模型3 | 模型4 | ||||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | |
| 总人群 | <0.01a | <0.01a | <0.01a | <0.01a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.15(1.03~1.28) | 0.01 | 1.08(0.97~1.20) | 0.15 | 1.08(0.97~1.20) | 0.18 | 1.07(0.96~1.19) | 0.21 |
| Q3组 | 1.31(1.18~1.46) | <0.01 | 1.16(1.04~1.29) | 0.01 | 1.16(1.04~1.28) | 0.01 | 1.14(1.03~1.27) | 0.01 |
| Q4组 | 1.53(1.38~1.69) | <0.01 | 1.30(1.18~1.45) | <0.01 | 1.30(1.17~1.44) | <0.01 | 1.24(1.09~1.40) | <0.01 |
| <40岁 | <0.01a | 0.07a | 0.06a | 0.35a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 0.64(0.28~1.43) | 0.27 | 0.57(0.26~1.28) | 0.17 | 0.56(0.25~1.26) | 0.15 | 0.55(0.24~1.23) | 0.14 |
| Q3组 | 1.59(0.85~2.96) | 0.14 | 1.27(0.67~2.39) | 0.46 | 1.31(0.70~2.48) | 0.39 | 1.24(0.66~2.35) | 0.50 |
| Q4组 | 1.92(1.05~3.50) | 0.03 | 1.46(0.78~2.72) | 0.23 | 1.49(0.80~2.79) | 0.21 | 1.15(0.56~2.36) | 0.71 |
| 40~49岁 | <0.01a | <0.01a | <0.01a | 0.03a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.29(0.98~1.71) | 0.07 | 1.22(0.92~1.61) | 0.16 | 1.22(0.92~1.61) | 0.17 | 1.21(0.91~1.60) | 0.18 |
| Q3组 | 1.42(1.09~1.86) | 0.01 | 1.22(0.93~1.60) | 0.14 | 1.23(0.94~1.62) | 0.13 | 1.22(0.93~1.61) | 0.15 |
| Q4组 | 1.76(1.36~2.27) | <0.01 | 1.45(1.11~1.88) | 0.01 | 1.47(1.13~1.91) | <0.01 | 1.43(1.05~1.95) | 0.02 |
| 50~59岁 | <0.01a | <0.01a | <0.01a | 0.04a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.13(0.95~1.35) | 0.16 | 1.07(0.90~1.28) | 0.46 | 1.07(0.89~1.27) | 0.47 | 1.07(0.89~1.27) | 0.48 |
| Q3组 | 1.22(1.03~1.44) | 0.02 | 1.08(0.91~1.28) | 0.38 | 1.08(0.91~1.28) | 0.39 | 1.07(0.90~1.27) | 0.46 |
| Q4组 | 1.49(1.27~1.76) | <0.01 | 1.28(1.08~1.51) | <0.01 | 1.27(1.08~1.50) | <0.01 | 1.22(1.01~1.49) | 0.04 |
| ≥60岁 | <0.01a | <0.01a | <0.01a | 0.03a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.10(0.94~1.29) | 0.24 | 1.06(0.90~1.24) | 0.48 | 1.05(0.90~1.23) | 0.54 | 1.04(0.89~1.22) | 0.59 |
| Q3组 | 1.25(1.07~1.47) | 0.00 | 1.17(0.99~1.37) | 0.05 | 1.17(0.99~1.37) | 0.06 | 1.15(0.98~1.35) | 0.09 |
| Q4组 | 1.39(1.19~1.62) | <0.01 | 1.27(1.09~1.49) | <0.01 | 1.26(1.07~1.47) | <0.01 | 1.20(0.99~1.44) | 0.05 |
表7 排除随访时间<1年研究对象后不同CAR分组总人群及不同年龄段人群CVD发生率的Cox比例风险回归模型分析结果
Table 7 Results of Cox proportional hazards model analysis on the incidence of cvd in different car groups and different age groups after excluding study subjects with follow-up time <1 year
| 分组 | 模型1 | 模型2 | 模型3 | 模型4 | ||||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | |
| 总人群 | <0.01a | <0.01a | <0.01a | <0.01a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.15(1.03~1.28) | 0.01 | 1.08(0.97~1.20) | 0.15 | 1.08(0.97~1.20) | 0.18 | 1.07(0.96~1.19) | 0.21 |
| Q3组 | 1.31(1.18~1.46) | <0.01 | 1.16(1.04~1.29) | 0.01 | 1.16(1.04~1.28) | 0.01 | 1.14(1.03~1.27) | 0.01 |
| Q4组 | 1.53(1.38~1.69) | <0.01 | 1.30(1.18~1.45) | <0.01 | 1.30(1.17~1.44) | <0.01 | 1.24(1.09~1.40) | <0.01 |
| <40岁 | <0.01a | 0.07a | 0.06a | 0.35a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 0.64(0.28~1.43) | 0.27 | 0.57(0.26~1.28) | 0.17 | 0.56(0.25~1.26) | 0.15 | 0.55(0.24~1.23) | 0.14 |
| Q3组 | 1.59(0.85~2.96) | 0.14 | 1.27(0.67~2.39) | 0.46 | 1.31(0.70~2.48) | 0.39 | 1.24(0.66~2.35) | 0.50 |
| Q4组 | 1.92(1.05~3.50) | 0.03 | 1.46(0.78~2.72) | 0.23 | 1.49(0.80~2.79) | 0.21 | 1.15(0.56~2.36) | 0.71 |
| 40~49岁 | <0.01a | <0.01a | <0.01a | 0.03a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.29(0.98~1.71) | 0.07 | 1.22(0.92~1.61) | 0.16 | 1.22(0.92~1.61) | 0.17 | 1.21(0.91~1.60) | 0.18 |
| Q3组 | 1.42(1.09~1.86) | 0.01 | 1.22(0.93~1.60) | 0.14 | 1.23(0.94~1.62) | 0.13 | 1.22(0.93~1.61) | 0.15 |
| Q4组 | 1.76(1.36~2.27) | <0.01 | 1.45(1.11~1.88) | 0.01 | 1.47(1.13~1.91) | <0.01 | 1.43(1.05~1.95) | 0.02 |
| 50~59岁 | <0.01a | <0.01a | <0.01a | 0.04a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.13(0.95~1.35) | 0.16 | 1.07(0.90~1.28) | 0.46 | 1.07(0.89~1.27) | 0.47 | 1.07(0.89~1.27) | 0.48 |
| Q3组 | 1.22(1.03~1.44) | 0.02 | 1.08(0.91~1.28) | 0.38 | 1.08(0.91~1.28) | 0.39 | 1.07(0.90~1.27) | 0.46 |
| Q4组 | 1.49(1.27~1.76) | <0.01 | 1.28(1.08~1.51) | <0.01 | 1.27(1.08~1.50) | <0.01 | 1.22(1.01~1.49) | 0.04 |
| ≥60岁 | <0.01a | <0.01a | <0.01a | 0.03a | ||||
| Q1组 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Q2组 | 1.10(0.94~1.29) | 0.24 | 1.06(0.90~1.24) | 0.48 | 1.05(0.90~1.23) | 0.54 | 1.04(0.89~1.22) | 0.59 |
| Q3组 | 1.25(1.07~1.47) | 0.00 | 1.17(0.99~1.37) | 0.05 | 1.17(0.99~1.37) | 0.06 | 1.15(0.98~1.35) | 0.09 |
| Q4组 | 1.39(1.19~1.62) | <0.01 | 1.27(1.09~1.49) | <0.01 | 1.26(1.07~1.47) | <0.01 | 1.20(0.99~1.44) | 0.05 |
| 分组 | 模型1 | 模型2 | 模型3 | 模型4 | ||||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | |
| Q1组 | 1.00 | <0.01a | 1.00 | <0.01a | 1.00 | <0.01a | 1.00 | <0.01a |
| Q2组 | 1.03(0.89~1.20) | 0.70 | 0.99(0.85~1.15) | 0.91 | 0.98(0.85~1.14) | 0.82 | 0.98(0.84~1.13) | 0.73 |
| Q3组 | 1.19(1.02~1.38) | 0.02 | 1.11(0.95~1.29) | 0.18 | 1.10(0.95~1.28) | 0.20 | 1.08(0.93~1.26) | 0.33 |
| Q4组 | 1.33(1.15~1.54) | <0.01 | 1.21(1.05~1.41) | 0.01 | 1.20(1.03~1.39) | 0.01 | 1.11(0.93~1.33) | 0.24 |
表8 ≥60岁不同CAR分组人群CVD发生率的死亡竞争风险模型分析
Table 8 Analysis of the mortality competitive risk model for the incidence of CVD in different CAR groups aged ≥60 years
| 分组 | 模型1 | 模型2 | 模型3 | 模型4 | ||||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | HR(95%CI) | P(P趋势)值 | |
| Q1组 | 1.00 | <0.01a | 1.00 | <0.01a | 1.00 | <0.01a | 1.00 | <0.01a |
| Q2组 | 1.03(0.89~1.20) | 0.70 | 0.99(0.85~1.15) | 0.91 | 0.98(0.85~1.14) | 0.82 | 0.98(0.84~1.13) | 0.73 |
| Q3组 | 1.19(1.02~1.38) | 0.02 | 1.11(0.95~1.29) | 0.18 | 1.10(0.95~1.28) | 0.20 | 1.08(0.93~1.26) | 0.33 |
| Q4组 | 1.33(1.15~1.54) | <0.01 | 1.21(1.05~1.41) | 0.01 | 1.20(1.03~1.39) | 0.01 | 1.11(0.93~1.33) | 0.24 |
| [1] |
GBD 2021 Diseases and Injuries Collaborators. Global incidence,prevalence,years lived with disability(YLDs),disability-adjusted life-years(DALYs),and healthy life expectancy(HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations,1990-2021:a systematic analysis for the Global Burden of Disease Study 2021[J]. Lancet,2024,403(10440):2133-2161. DOI:10.1016/S0140-6736(24)00757-8.
|
| [2] |
GBD 2021 Causes of Death Collaborators. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations,1990-2021:a systematic analysis for the Global Burden of Disease Study 2021[J]. Lancet,2024,403(10440):2100-2132. DOI:10.1016/S0140-6736(24)00367-2.
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
Emerging Risk Factors Collaboration,
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [21] |
|
| [22] |
|
| [23] |
|
| [24] |
|
| [25] |
|
| [26] |
|
| [27] |
|
| [28] |
|
| [29] |
|
| [30] |
|
| [31] |
|
| [32] |
|
| [33] |
|
| [34] |
|
| [35] |
|
| [36] |
|
| [37] |
吴寿岭,赵晓琳,高明,等. 唐山地区健康成年人群血清高敏C反应蛋白的正常值参考范围[J]. 中华高血压杂志,2013,21(7):675-678. DOI:10.16439/j.cnki.1673-7245.2013.07.004.
|
| [38] |
|
| [1] | 范转转, 李文婷, 马国亮. 绝经后女性内脏脂肪指数与心血管疾病的关联性分析:前瞻性队列研究[J]. 中国全科医学, 2026, 29(02): 180-187. |
| [2] | 张姝, 程钰, 吴寿岭, 陈朔华, 吴云涛. 非糖尿病人群累积血浆致动脉粥样硬化指数暴露对新发心血管疾病影响的队列研究[J]. 中国全科医学, 2025, 28(36): 4558-4565. |
| [3] | 张颖, 廖晓阳, 杨寒飞, 余泳君, 刘力滴, 贾禹, 沈灿, 李霄, 黄传应, 杨荣. 2024年《国际高血压学会立场文件:血压测量与报告技术创新》解读及对中国的启示[J]. 中国全科医学, 2025, 28(36): 4541-4549. |
| [4] | 曾明慧, 蒯文涛, 陈林, 韩家鑫, 徐连欣, 葛立颖, 代容容, 宓余强, 徐亮. 2型糖尿病对核苷(酸)类似物治疗慢性乙型肝炎效果的影响研究[J]. 中国全科医学, 2025, 28(35): 4414-4420. |
| [5] | 赵倬, 王贺. 缺氧诱导因子2α在心血管系统疾病中的作用机制研究进展[J]. 中国全科医学, 2025, 28(33): 4241-4248. |
| [6] | 王碧优, 高鹰, 尤俊方, 刘莉, 张卿, 苏海燕. 心血管疾病风险人群脂质比值与炎症指标的典型相关性研究[J]. 中国全科医学, 2025, 28(33): 4132-4139. |
| [7] | 陈慧龙, 廖芸楚, 刘育伟, 孔政辉, 黄兴辉, 徐嘉辉, 漆娜, 王远平, 梁文坚. 相对脂肪量与中老年人群心血管疾病之间的关联:一项基于CHARLS的横断面与纵向研究[J]. 中国全科医学, 2025, 28(32): 4047-4054. |
| [8] | 刘明波, 何新叶, 杨晓红, 王增武. 《中国心血管健康与疾病报告2024》要点解读[J]. 中国全科医学, 2025, 28(32): 3989-4008. |
| [9] | 廖姣姣, 王照宇, 李兆基, 赵威, 詹思延, 王鹏, 陶立元. 非高密度脂蛋白胆固醇动态变化对颈动脉内中膜增厚的预测价值:一项双向性队列研究[J]. 中国全科医学, 2025, 28(31): 3932-3941. |
| [10] | 张骥, 周婕, 李凌, 吴延莉, 吉维, 刘涛. 空腹血糖水平与全因死亡和特定原因死亡风险的前瞻性队列研究[J]. 中国全科医学, 2025, 28(31): 3924-3931. |
| [11] | 苏晴, 徐曜, 李一航, 汪丽燕, 蔡业峰, 倪小佳. 脑卒中及其风险人群中医证候演变规律研究的方法学质量评价[J]. 中国全科医学, 2025, 28(29): 3694-3702. |
| [12] | 邓洁, 齐祺, 吴欣雨, 韩全乐, 李雷, 蒋越, 郁静, 吴若洁, 吴寿岭, 李康博. 血浆致动脉硬化指数与体检人群新发心力衰竭风险的队列研究[J]. 中国全科医学, 2025, 28(29): 3645-3652. |
| [13] | 周晟, 邓长生, 邹冠炀, 宋健平. 疟疾心血管疾病并发症发病机制的研究进展[J]. 中国全科医学, 2025, 28(27): 3466-3472. |
| [14] | 程雨欣, 方嘉敏, 梁好, 汪志玲, 魏琳, 廖惠莲, 徐明明, 陈玉梅, 李燕芬, 董丽娟, 郭银桂. 老年择期手术患者术前血小板计数/白蛋白比值与术后新发衰弱的相关性分析:一项多中心研究[J]. 中国全科医学, 2025, 28(27): 3359-3367. |
| [15] | 向心月, 张冰青, 欧阳煜钦, 汤文娟, 冯文焕. 短期内科门诊减重对肥胖患者动脉粥样硬化性心血管疾病风险的影响研究[J]. 中国全科医学, 2025, 28(26): 3229-3239. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





