中国全科医学 ›› 2024, Vol. 27 ›› Issue (15): 1802-1810.DOI: 10.12114/j.issn.1007-9572.2023.0808
张国莉1, 赵荣荣2, 彭国恬1, 孙瑞仪1, 乔鹏宇1, 燕芳红1,3, 韩琳1,3,4,*( )
)
收稿日期:2023-10-12
修回日期:2024-01-04
出版日期:2024-05-20
发布日期:2024-02-28
通讯作者:
韩琳
基金资助:
ZHANG Guoli1, ZHAO Rongrong2, PENG Guotian1, SUN Ruiyi1, QIAO Pengyu1, YAN Fanghong1,3, HAN Lin1,3,4,*( )
)
Received:2023-10-12
Revised:2024-01-04
Published:2024-05-20
Online:2024-02-28
Contact:
HAN Lin
摘要: 背景 ST段抬高型心肌梗死(STEMI)患者经皮冠状动脉介入治疗(PCI)术后远期发生主要不良心血管事件(MACEs)的风险大,指南指出准确的早期危险分层对STEMI患者PCI术后MACEs的管理具有重要意义。目前,常用的风险评分系统包括年龄、血肌酐和射血分数(ACEF)评分、心肌梗死溶栓(TIMI)评分、Zwolle评分、首次心肌梗死血管成形术(PAMI)评分、使用控制阿昔单抗和装置的研究以降低晚期血管成形术并发症(CADILLAC),然而哪种风险评分系统更适用于预测STEMI患者PCI治疗远期预后尚无定论。目的 分析我国STEMI患者PCI术后远期MACEs发生的危险因素并比较我国目前常用的ACEF、TIMI、Zwolle、PAMI、CADILLAC五种风险评分系统对其远期MACEs发生风险的预测价值。方法 回顾性选取2016年6月—2020年6月在甘肃省人民医院心内科成功完成首次PCI术的687例STEMI患者为研究对象。收集患者一般资料与实验室及影像学检查结果,患者入组后均采用ACEF、TIMI、Zwolle、PAMI、CADILLAC风险评分系统进行评分。出院后通过电话及门诊复查方式随访患者,每年随访1次,随访时间截至2023年8月,主要记录随访期间患者MACEs的发生情况。采用多因素Logistic回归分析探究STEMI患者PCI术后远期MACEs发生的影响因素。绘制不同风险评分系统诊断MACEs的受试者工作特征曲线(ROC曲线),采用DeLong检验比较各风险评分系统的ROC曲线下面积(AUC)。结果 687例STEMI患者接受了PCI术,随访过程中44例患者因基本资料数据缺失过多被剔除,最终纳入643例患者,中位随访时间为37(25,49)个月。至随访结束共有134例发生MACEs,发生率为20.8%。MACEs组和非MACEs组年龄、住院时间、Killip分级、脑利钠肽前体、纤维蛋白原、贫血、左心室射血分数、估算肾小球滤过率、血肌酐、瓣膜返流比较,差异有统计学意义(P<0.05)。多因素Logistic回归分析结果显示:住院时间延长(OR=1.071,95%CI=1.012~1.134,P=0.018)、血肌酐升高(OR=1.018,95%CI=1.006~1.030,P=0.003)、纤维蛋白原升高(OR=1.226,95%CI=1.066~1.409,P=0.004)为患者发生MACEs的危险因素,左心室射血分数增加(OR=0.980,95%CI=0.960~1.000,P=0.045)、瓣膜轻度返流(OR=0.377,95%CI=0.151~0.938,P=0.036)和中度返流(OR=0.164,95%CI=0.051~0.522,P=0.002)为患者发生MACEs的保护因素。MACEs组的ACEF、TIMI、Zwolle、PAMI、CADILLAC风险评分系统得分均高于非MACEs组(P<0.05)。绘制5种风险评分系统预测STEMI患者PCI术后远期发生MACEs的ROC曲线,5种风险评分系统对STEMI患者PCI术后远期MACEs的预测价值比较,差异无统计学意义(P>0.05)。结论 住院时间、血肌酐水平、纤维蛋白原、左心室射血分数、瓣膜返流状态是影响STEMI患者PCI术后远期发生MACEs的影响因素。ACEF、TIMI、Zwolle、PAMI、CADILLAC五种风险评分系统均能预测STEMI患者PCI术后远期MACEs的发生,但从区分度和灵敏度方面考虑推荐使用CADILLAC评分。
| 项目 | ACEF | TIMI | Zwolle | PAMI | CADILLAC |
|---|---|---|---|---|---|
| 年龄 | + | + | + | + | + |
| 病史 | |||||
| 糖尿病 | + | + | |||
| 高血压 | + | ||||
| 心绞痛 | + | ||||
| 心肌缺血时间 | + | + | |||
| 体格检查 | |||||
| 收缩压 | + | ||||
| 心率 | + | + | |||
| 体质量 | + | ||||
| 影像学检查 | |||||
| 梗死部位 | + | + | + | ||
| 左心室射血分数 | + | + | |||
| 心功能分级 | + | + | + | + | |
| TIMI血流分级 | + | + | |||
| 病变血管支数 | + | + | |||
| 实验室检查 | |||||
| 血肌酐 | + | ||||
| eGFR | + | ||||
| 血红蛋白计数 | + |
表1 不同风险评分系统指标
Table 1 Different risk scoring system indicators
| 项目 | ACEF | TIMI | Zwolle | PAMI | CADILLAC |
|---|---|---|---|---|---|
| 年龄 | + | + | + | + | + |
| 病史 | |||||
| 糖尿病 | + | + | |||
| 高血压 | + | ||||
| 心绞痛 | + | ||||
| 心肌缺血时间 | + | + | |||
| 体格检查 | |||||
| 收缩压 | + | ||||
| 心率 | + | + | |||
| 体质量 | + | ||||
| 影像学检查 | |||||
| 梗死部位 | + | + | + | ||
| 左心室射血分数 | + | + | |||
| 心功能分级 | + | + | + | + | |
| TIMI血流分级 | + | + | |||
| 病变血管支数 | + | + | |||
| 实验室检查 | |||||
| 血肌酐 | + | ||||
| eGFR | + | ||||
| 血红蛋白计数 | + |
| 组别 | 例数 | 年龄[M(P25,P75),岁] | 性别(男/女) | 高血压[例(%)] | 糖尿病[例(%)] | 血脂异常[例(%)] | 脑卒中[例(%)] | 吸烟[例(%)] | 饮酒[例(%)] | 发生急性心肌缺血时间>4 h[例(%)] | 身高[M(P25,P75),cm] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 非MACEs组 | 509 | 60.0(52.0,66.0) | 436/73 | 231(45.4) | 96(18.9) | 17(3.3) | 46(9.0) | 323(63.5) | 162(31.8) | 442(86.8) | 170.0(165.0,172.0) | |
| MACEs组 | 134 | 64.0(54.0,69.0) | 112/22 | 71(53.0) | 30(22.3) | 5(3.7) | 18(13.4) | 78(58.2) | 31(23.1) | 121(90.3) | 170.0(165.0,173.9) | |
| Z(χ2)值 | -2.428 | 0.363a | 2.461a | 0.838a | 0.049a | 2.287a | 1.548a | 3.816a | 1.167a | -1.287 | ||
| P值 | 0.015 | 0.547 | 0.117 | 0.360 | 0.824 | 0.130 | 0.213 | 0.051 | 0.280 | 0.198 | ||
| 组别 | 体质量[M(P25,P75),kg] | 收缩压[M(P25,P75),mmHg] | 舒张压[M(P25,P75),mmHg] | 心率[M(P25,P75),次/min] | 住院时间[M(P25,P75),d] | Killip分级[例(%)] | 糖化血红蛋白[M(P25,P75),%] | |||||
| Ⅰ级 | Ⅱ级 | Ⅲ级+Ⅳ级 | ||||||||||
| 非MACEs组 | 70.0(65.0,78.3) | 125(115,140) | 80(70,88) | 76(66,85) | 7(5,10) | 429(84.3) | 68(13.4) | 12(2.3) | 5.7(5.3,6.2) | |||
| MACEs组 | 76.0(64.7,79.8) | 125(113,139) | 78(69,86) | 77(67,86) | 8.0(5,11) | 100(74.6) | 25(18.7) | 9(6.7) | 5.7(5.4,6.3) | |||
| Z(χ2)值 | -0.296 | -0.668 | -1.370 | -0.293 | -3.024 | 9.431a | -0.359 | |||||
| P值 | 0.767 | 0.504 | 0.171 | 0.769 | 0.002 | 0.009 | 0.719 | |||||
| 组别 | 空腹血糖[M(P25,P75),mmol/L] | 白细胞计数[M(P25,P75),×109/L] | 中性粒细胞计数[M(P25,P75),×109/L] | 淋巴细胞计数[M(P25,P75),×109/L] | 高密度脂蛋白[M(P25,P75),g/L] | 低密度脂蛋白[M(P25,P75),g/L] | 丙氨酸氨基转移酶[M(P25,P75),U/L] | 天冬氨酸氨基转移酶[M(P25,P75),U/L] | ||||
| 非MACEs组 | 6.6(5.4,8.7) | 9.3(7.1,11.8) | 7.0(5.0,9.7) | 1.4(1.0,1.8) | 1.0(0.8,1.1) | 2.3(1.9,2.9) | 41.0(26.0,65.6) | 105.0(40.0,235.0) | ||||
| MACEs组 | 6.8(5.3,9.4) | 9.3(7.4,12.0) | 7.2(5.4,10.0) | 1.3(1.0,1.7) | 1.0(0.8,1.1) | 2.2(1.7,2.8) | 43.0(26.3,74.0) | 113.0(43.0,278.4) | ||||
| Z(χ2)值 | -0.191 | -0.417 | -0.711 | -1.306 | -0.059 | -1.341 | -0.608 | -0.099 | ||||
| P值 | 0.849 | 0.676 | 0.477 | 0.191 | 0.953 | 0.180 | 0.543 | 0.549 | ||||
| 组别 | 同型半胱氨酸[M(P25,P75),U/L] | 超敏肌钙蛋白[M(P25,P75),μg/L] | 乳酸脱氢酶峰值[M(P25,P75),U/L] | 肌酸激酶峰值[M(P25,P75),U/L] | 肌酸激酶同工酶[M(P25,P75),U/L] | 脑利钠肽前体[M(P25,P75),ng/L] | ||||||
| 非MACEs组 | 17.5(11.8,34.9) | 0.7(0.1,3.0) | 511.4(320.3,819.0) | 1 170.3(242.0,3 347.0) | 107.8(28.0,273.3) | 675.2(247.2,1 860.5) | ||||||
| MACEs组 | 17.8(11.6,29.7) | 0.8(0.0,5.1) | 523.2(321.0,875.6) | 1 097.4(251.3,2 799.0) | 89.8(25.6,259.9) | 996.5(342.9,2 773.0) | ||||||
| Z(χ2)值 | -0.138 | -0.451 | -0.560 | -0.576 | -0.728 | -2.399 | ||||||
| P值 | 0.890 | 0.652 | 0.575 | 0.564 | 0.467 | 0.016 | ||||||
| 组别 | 入院凝血酶原时间[M(P25,P75),s] | 入院活化部分凝血酶原时间[M(P25,P75),s] | 血肌酐[M(P25,P75),μmol/L] | 纤维蛋白原[M(P25,P75),g/L] | 贫血[例(%)] | 左心室射血分数[M(P25,P75),%] | 支架数目[M(P25,P75),个] | 心腔大小正常[例(%)] | 室壁瘤[例(%)] | |||
| 非MACEs组 | 13.4(12.8,14.0) | 35.6(32.5,39.5) | 66.0(58.0,75.6) | 3.3(2.8,4.2) | 89(17.5) | 52.0(46.0,59.0) | 2(1,2) | 308(60.5) | 13(2.6) | |||
| MACEs组 | 13.5(12.8,14.2) | 35.7(32.7,39.9) | 72.0(60.1,85.3) | 3.6(2.9,4.7) | 38(28.4) | 50.0(43.0,56.5) | 2(1,2) | 92(68.7) | 6(4.5) | |||
| Z(χ2)值 | -0.786 | -0.210 | -3.786 | -2.635 | 7.912a | -2.397 | -1.155 | 2.994a | 1.369a | |||
| P值 | 0.432 | 0.833 | <0.001 | 0.008 | 0.005 | 0.017 | 0.248 | 0.084 | 0.242 | |||
| 组别 | eGFR[例(%)] | TIMI血流分级[例(%)] | 瓣膜返流[例(%)] | 心肌梗死部位[例(%)] | 病变血管数[例(%)] | |||||||
| 异常 | 正常 | 无复流/慢血流 | 正常血流 | 轻度返流 | 中度返流 | 重度返流 | 前壁 | 非前壁 | 单支 | 双支 | 左主干或三支病变 | |
| 非MACEs组 | 35(6.9) | 474(93.1) | 279(54.8) | 230(45.2) | 450(88.4) | 47(9.2) | 12(2.4) | 241(47.3) | 268(52.7) | 117(23.0) | 163(32.0) | 229(45.0) |
| MACEs组 | 1(0.8) | 133(99.2) | 78(58.2) | 56(41.8) | 114(85.1) | 9(6.7) | 11(8.2) | 64(47.8) | 70(52.2) | 26(19.4) | 36(26.9) | 72(53.7) |
| Z(χ2)值 | 7.541a | 0.495a | 11.060a | 0.007a | 3.256a | |||||||
| P值 | 0.006 | 0.482 | 0.004 | 0.932 | 0.196 | |||||||
表2 非MACEs组和MACEs组患者一般资料比较结果
Table 2 Comparison of general data between non-MACES group and MACEs group
| 组别 | 例数 | 年龄[M(P25,P75),岁] | 性别(男/女) | 高血压[例(%)] | 糖尿病[例(%)] | 血脂异常[例(%)] | 脑卒中[例(%)] | 吸烟[例(%)] | 饮酒[例(%)] | 发生急性心肌缺血时间>4 h[例(%)] | 身高[M(P25,P75),cm] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 非MACEs组 | 509 | 60.0(52.0,66.0) | 436/73 | 231(45.4) | 96(18.9) | 17(3.3) | 46(9.0) | 323(63.5) | 162(31.8) | 442(86.8) | 170.0(165.0,172.0) | |
| MACEs组 | 134 | 64.0(54.0,69.0) | 112/22 | 71(53.0) | 30(22.3) | 5(3.7) | 18(13.4) | 78(58.2) | 31(23.1) | 121(90.3) | 170.0(165.0,173.9) | |
| Z(χ2)值 | -2.428 | 0.363a | 2.461a | 0.838a | 0.049a | 2.287a | 1.548a | 3.816a | 1.167a | -1.287 | ||
| P值 | 0.015 | 0.547 | 0.117 | 0.360 | 0.824 | 0.130 | 0.213 | 0.051 | 0.280 | 0.198 | ||
| 组别 | 体质量[M(P25,P75),kg] | 收缩压[M(P25,P75),mmHg] | 舒张压[M(P25,P75),mmHg] | 心率[M(P25,P75),次/min] | 住院时间[M(P25,P75),d] | Killip分级[例(%)] | 糖化血红蛋白[M(P25,P75),%] | |||||
| Ⅰ级 | Ⅱ级 | Ⅲ级+Ⅳ级 | ||||||||||
| 非MACEs组 | 70.0(65.0,78.3) | 125(115,140) | 80(70,88) | 76(66,85) | 7(5,10) | 429(84.3) | 68(13.4) | 12(2.3) | 5.7(5.3,6.2) | |||
| MACEs组 | 76.0(64.7,79.8) | 125(113,139) | 78(69,86) | 77(67,86) | 8.0(5,11) | 100(74.6) | 25(18.7) | 9(6.7) | 5.7(5.4,6.3) | |||
| Z(χ2)值 | -0.296 | -0.668 | -1.370 | -0.293 | -3.024 | 9.431a | -0.359 | |||||
| P值 | 0.767 | 0.504 | 0.171 | 0.769 | 0.002 | 0.009 | 0.719 | |||||
| 组别 | 空腹血糖[M(P25,P75),mmol/L] | 白细胞计数[M(P25,P75),×109/L] | 中性粒细胞计数[M(P25,P75),×109/L] | 淋巴细胞计数[M(P25,P75),×109/L] | 高密度脂蛋白[M(P25,P75),g/L] | 低密度脂蛋白[M(P25,P75),g/L] | 丙氨酸氨基转移酶[M(P25,P75),U/L] | 天冬氨酸氨基转移酶[M(P25,P75),U/L] | ||||
| 非MACEs组 | 6.6(5.4,8.7) | 9.3(7.1,11.8) | 7.0(5.0,9.7) | 1.4(1.0,1.8) | 1.0(0.8,1.1) | 2.3(1.9,2.9) | 41.0(26.0,65.6) | 105.0(40.0,235.0) | ||||
| MACEs组 | 6.8(5.3,9.4) | 9.3(7.4,12.0) | 7.2(5.4,10.0) | 1.3(1.0,1.7) | 1.0(0.8,1.1) | 2.2(1.7,2.8) | 43.0(26.3,74.0) | 113.0(43.0,278.4) | ||||
| Z(χ2)值 | -0.191 | -0.417 | -0.711 | -1.306 | -0.059 | -1.341 | -0.608 | -0.099 | ||||
| P值 | 0.849 | 0.676 | 0.477 | 0.191 | 0.953 | 0.180 | 0.543 | 0.549 | ||||
| 组别 | 同型半胱氨酸[M(P25,P75),U/L] | 超敏肌钙蛋白[M(P25,P75),μg/L] | 乳酸脱氢酶峰值[M(P25,P75),U/L] | 肌酸激酶峰值[M(P25,P75),U/L] | 肌酸激酶同工酶[M(P25,P75),U/L] | 脑利钠肽前体[M(P25,P75),ng/L] | ||||||
| 非MACEs组 | 17.5(11.8,34.9) | 0.7(0.1,3.0) | 511.4(320.3,819.0) | 1 170.3(242.0,3 347.0) | 107.8(28.0,273.3) | 675.2(247.2,1 860.5) | ||||||
| MACEs组 | 17.8(11.6,29.7) | 0.8(0.0,5.1) | 523.2(321.0,875.6) | 1 097.4(251.3,2 799.0) | 89.8(25.6,259.9) | 996.5(342.9,2 773.0) | ||||||
| Z(χ2)值 | -0.138 | -0.451 | -0.560 | -0.576 | -0.728 | -2.399 | ||||||
| P值 | 0.890 | 0.652 | 0.575 | 0.564 | 0.467 | 0.016 | ||||||
| 组别 | 入院凝血酶原时间[M(P25,P75),s] | 入院活化部分凝血酶原时间[M(P25,P75),s] | 血肌酐[M(P25,P75),μmol/L] | 纤维蛋白原[M(P25,P75),g/L] | 贫血[例(%)] | 左心室射血分数[M(P25,P75),%] | 支架数目[M(P25,P75),个] | 心腔大小正常[例(%)] | 室壁瘤[例(%)] | |||
| 非MACEs组 | 13.4(12.8,14.0) | 35.6(32.5,39.5) | 66.0(58.0,75.6) | 3.3(2.8,4.2) | 89(17.5) | 52.0(46.0,59.0) | 2(1,2) | 308(60.5) | 13(2.6) | |||
| MACEs组 | 13.5(12.8,14.2) | 35.7(32.7,39.9) | 72.0(60.1,85.3) | 3.6(2.9,4.7) | 38(28.4) | 50.0(43.0,56.5) | 2(1,2) | 92(68.7) | 6(4.5) | |||
| Z(χ2)值 | -0.786 | -0.210 | -3.786 | -2.635 | 7.912a | -2.397 | -1.155 | 2.994a | 1.369a | |||
| P值 | 0.432 | 0.833 | <0.001 | 0.008 | 0.005 | 0.017 | 0.248 | 0.084 | 0.242 | |||
| 组别 | eGFR[例(%)] | TIMI血流分级[例(%)] | 瓣膜返流[例(%)] | 心肌梗死部位[例(%)] | 病变血管数[例(%)] | |||||||
| 异常 | 正常 | 无复流/慢血流 | 正常血流 | 轻度返流 | 中度返流 | 重度返流 | 前壁 | 非前壁 | 单支 | 双支 | 左主干或三支病变 | |
| 非MACEs组 | 35(6.9) | 474(93.1) | 279(54.8) | 230(45.2) | 450(88.4) | 47(9.2) | 12(2.4) | 241(47.3) | 268(52.7) | 117(23.0) | 163(32.0) | 229(45.0) |
| MACEs组 | 1(0.8) | 133(99.2) | 78(58.2) | 56(41.8) | 114(85.1) | 9(6.7) | 11(8.2) | 64(47.8) | 70(52.2) | 26(19.4) | 36(26.9) | 72(53.7) |
| Z(χ2)值 | 7.541a | 0.495a | 11.060a | 0.007a | 3.256a | |||||||
| P值 | 0.006 | 0.482 | 0.004 | 0.932 | 0.196 | |||||||
| 变量 | B | SE | Wald χ2值 | P值 | OR(95%CI) |
|---|---|---|---|---|---|
| 年龄 | 0.010 | 0.010 | 0.964 | 0.326 | 1.010(0.990~1.030) |
| 住院时间 | 0.069 | 0.029 | 5.585 | 0.018 | 1.071(1.012~1.134) |
| eGFR分级正常 | 1.614 | 1.040 | 2.406 | 0.121 | 5.021(0.654~38.577) |
| 血肌酐 | 0.018 | 0.006 | 8.819 | 0.003 | 1.018(1.006~1.030) |
| 脑利纳肽前体 | 0.000 | 0.000 | 1.480 | 0.224 | 1.000(1.000~1.000) |
| 纤维蛋白原 | 0.203 | 0.071 | 8.142 | 0.004 | 1.226(1.066~1.409) |
| 左心室射血分数 | -0.021 | 0.010 | 4.008 | 0.045 | 0.980(0.960~1.000) |
| 贫血 | 0.411 | 0.246 | 2.787 | 0.095 | 1.508(0.931~2.443) |
| 瓣膜返流(以重度返流为参照) | |||||
| 轻度返流 | -0.976 | 0.465 | 4.400 | 0.036 | 0.377(0.151~0.938) |
| 中度返流 | -1.809 | 0.591 | 9.358 | 0.002 | 0.164(0.051~0.522) |
| Killip分级(以Ⅲ级+Ⅳ级为参照) | |||||
| Ⅰ级 | -0.620 | 0.539 | 1.326 | 0.250 | 0.538(0.187~1.546) |
| Ⅱ级 | -0.450 | 0.567 | 0.631 | 0.427 | 0.637(0.210~1.937) |
表3 STEMI患者PCI术后远期MACEs影响因素的多因素Logistic回归分析结果
Table 3 Multivariate Logistic regression analysis of long-term MACEs after PCI in STEMI patients
| 变量 | B | SE | Wald χ2值 | P值 | OR(95%CI) |
|---|---|---|---|---|---|
| 年龄 | 0.010 | 0.010 | 0.964 | 0.326 | 1.010(0.990~1.030) |
| 住院时间 | 0.069 | 0.029 | 5.585 | 0.018 | 1.071(1.012~1.134) |
| eGFR分级正常 | 1.614 | 1.040 | 2.406 | 0.121 | 5.021(0.654~38.577) |
| 血肌酐 | 0.018 | 0.006 | 8.819 | 0.003 | 1.018(1.006~1.030) |
| 脑利纳肽前体 | 0.000 | 0.000 | 1.480 | 0.224 | 1.000(1.000~1.000) |
| 纤维蛋白原 | 0.203 | 0.071 | 8.142 | 0.004 | 1.226(1.066~1.409) |
| 左心室射血分数 | -0.021 | 0.010 | 4.008 | 0.045 | 0.980(0.960~1.000) |
| 贫血 | 0.411 | 0.246 | 2.787 | 0.095 | 1.508(0.931~2.443) |
| 瓣膜返流(以重度返流为参照) | |||||
| 轻度返流 | -0.976 | 0.465 | 4.400 | 0.036 | 0.377(0.151~0.938) |
| 中度返流 | -1.809 | 0.591 | 9.358 | 0.002 | 0.164(0.051~0.522) |
| Killip分级(以Ⅲ级+Ⅳ级为参照) | |||||
| Ⅰ级 | -0.620 | 0.539 | 1.326 | 0.250 | 0.538(0.187~1.546) |
| Ⅱ级 | -0.450 | 0.567 | 0.631 | 0.427 | 0.637(0.210~1.937) |
| 组别 | 例数 | ACEF评分 | TIMI评分 | Zwolle评分 | PAMI评分 | CADILLAC评分 |
|---|---|---|---|---|---|---|
| 非MACEs组 | 509 | 1.1(1.0,1.3) | 6.0(4.0,7.0) | 4.0(3.0,6.0) | 2.0(0,4.0) | 4.0(2.0,6.0) |
| MACEs组 | 134 | 1.2(1.0,1.5) | 6.0(5.0,8.0) | 5.0(3.0,7.0) | 2.0(2.0,6.0) | 4.0(2.0,7.0) |
| Z值 | -2.925 | -2.333 | -2.524 | -3.288 | -3.434 | |
| P值 | 0.003 | 0.020 | 0.012 | 0.001 | <0.001 |
表4 非MACEs组和MACEs组患者5种风险评分系统得分比较[M(P25,P75),分]
Table 4 Comparison of 5 risk score systems between non-MACES group and MACEs group
| 组别 | 例数 | ACEF评分 | TIMI评分 | Zwolle评分 | PAMI评分 | CADILLAC评分 |
|---|---|---|---|---|---|---|
| 非MACEs组 | 509 | 1.1(1.0,1.3) | 6.0(4.0,7.0) | 4.0(3.0,6.0) | 2.0(0,4.0) | 4.0(2.0,6.0) |
| MACEs组 | 134 | 1.2(1.0,1.5) | 6.0(5.0,8.0) | 5.0(3.0,7.0) | 2.0(2.0,6.0) | 4.0(2.0,7.0) |
| Z值 | -2.925 | -2.333 | -2.524 | -3.288 | -3.434 | |
| P值 | 0.003 | 0.020 | 0.012 | 0.001 | <0.001 |
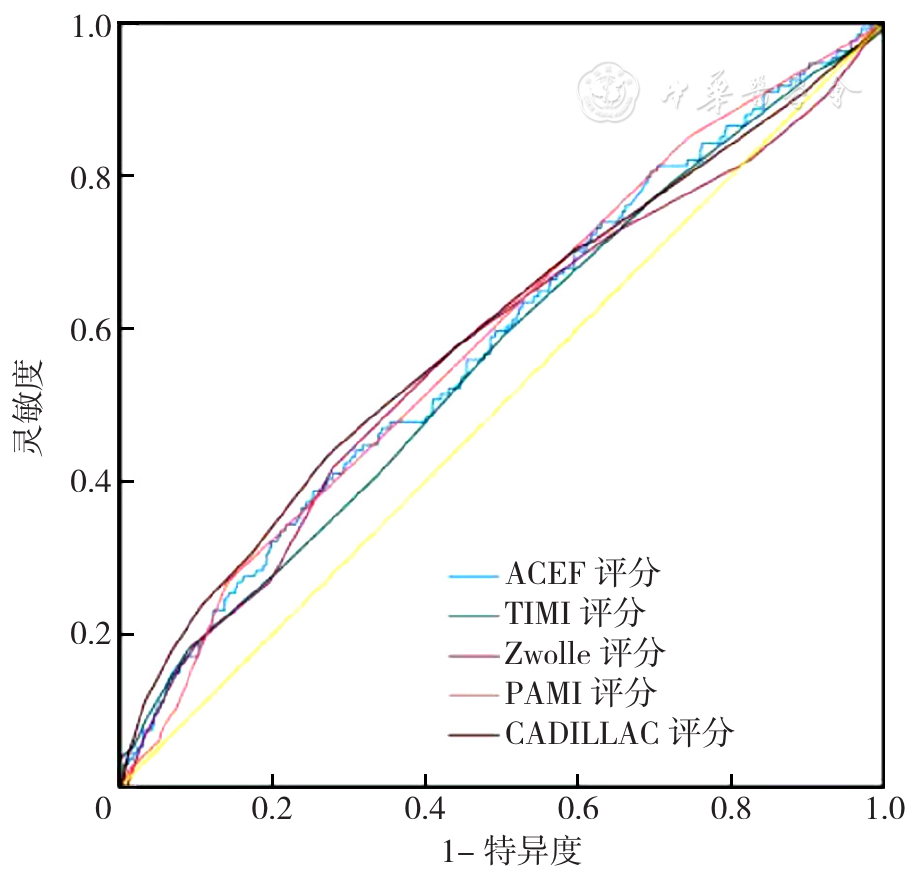
图1 5种风险评分系统预测STEMI患者PCI术后远期发生MACEs的ROC曲线注:ACEF=年龄、血肌酐和射血分数,TIMI=心肌梗死溶栓,PAMI=首次心肌梗死血管成形术,CADILLAC=使用控制阿昔单抗和装置的研究以降低晚期血管成形术并发症。
Figure 1 ROC curves of five risk scoring systems predicting MACEs after PCI in STEMI patients
| 指标 | AUC | 95%CI | 最佳截断值 | 灵敏度 | 特异度 | 约登指数 | P值 |
|---|---|---|---|---|---|---|---|
| ACEF评分 | 0.582 | (0.527~0.637) | 1.34分 | 0.388 | 0.747 | 0.135 | 0.003 |
| TIMI评分 | 0.565 | (0.509~0.620) | 8.50分 | 0.179 | 0.912 | 0.091 | 0.021 |
| Zwolle评分 | 0.570 | (0.513~0.627) | 5.50分 | 0.418 | 0.721 | 0.139 | 0.012 |
| PAMI评分 | 0.589 | (0.535~0.643) | 5.00分 | 0.269 | 0.859 | 0.127 | 0.002 |
| CADILLAC评分 | 0.595 | (0.538~0.652) | 5.50分 | 0.433 | 0.729 | 0.162 | 0.001 |
表5 5种风险评分系统对STEMI患者PCI术后远期MACEs的预测价值
Table 5 Predictive value of five risk score systems for long-term MACEs after PCI in STEMI patients
| 指标 | AUC | 95%CI | 最佳截断值 | 灵敏度 | 特异度 | 约登指数 | P值 |
|---|---|---|---|---|---|---|---|
| ACEF评分 | 0.582 | (0.527~0.637) | 1.34分 | 0.388 | 0.747 | 0.135 | 0.003 |
| TIMI评分 | 0.565 | (0.509~0.620) | 8.50分 | 0.179 | 0.912 | 0.091 | 0.021 |
| Zwolle评分 | 0.570 | (0.513~0.627) | 5.50分 | 0.418 | 0.721 | 0.139 | 0.012 |
| PAMI评分 | 0.589 | (0.535~0.643) | 5.00分 | 0.269 | 0.859 | 0.127 | 0.002 |
| CADILLAC评分 | 0.595 | (0.538~0.652) | 5.50分 | 0.433 | 0.729 | 0.162 | 0.001 |
| 指标 | ΔAUC | Z值 | P值 |
|---|---|---|---|
| ACEF评分比CADILLAC评分 | 0.013 | 0.493 | 0.622 |
| ACEF评分比PAMI评分 | 0.007 | 0.234 | 0.815 |
| ACEF评分比TIMI评分 | 0.017 | 0.540 | 0.589 |
| ACEF评分比Zwolle评分 | 0.012 | 0.390 | 0.697 |
| CADILLAC评分比PAMI评分 | 0.006 | 0.259 | 0.796 |
| CADILLAC评分比TIMI评分 | 0.030 | 1.097 | 0.273 |
| CADILLAC评分比Zwolle评分 | 0.025 | 1.244 | 0.214 |
| PAMI评分比TIMI评分 | 0.024 | 1.156 | 0.248 |
| PAMI评分比Zwolle评分 | 0.018 | 0.773 | 0.440 |
| TIMI评分比Zwolle评分 | 0.005 | 0.216 | 0.829 |
表6 5种风险评分系统预测STEMI患者PCI术后远期MACEs的AUC比较
Table 6 AUC comparison of five risk scoring systems predicting long-term MACEs after PCI in STEMI patients
| 指标 | ΔAUC | Z值 | P值 |
|---|---|---|---|
| ACEF评分比CADILLAC评分 | 0.013 | 0.493 | 0.622 |
| ACEF评分比PAMI评分 | 0.007 | 0.234 | 0.815 |
| ACEF评分比TIMI评分 | 0.017 | 0.540 | 0.589 |
| ACEF评分比Zwolle评分 | 0.012 | 0.390 | 0.697 |
| CADILLAC评分比PAMI评分 | 0.006 | 0.259 | 0.796 |
| CADILLAC评分比TIMI评分 | 0.030 | 1.097 | 0.273 |
| CADILLAC评分比Zwolle评分 | 0.025 | 1.244 | 0.214 |
| PAMI评分比TIMI评分 | 0.024 | 1.156 | 0.248 |
| PAMI评分比Zwolle评分 | 0.018 | 0.773 | 0.440 |
| TIMI评分比Zwolle评分 | 0.005 | 0.216 | 0.829 |
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
中华医学会心血管病学分会,中华心血管病杂志编辑委员会. 急性ST段抬高型心肌梗死诊断和治疗指南(2019)[J]. 中华心血管病杂志,2019,47(10):766-783. DOI:10.3760/cma.j.issn.0253?3758.2019.10.003.
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
李子孝,王春娟,王伊龙,等. 卒中临床诊疗和疾病管理核心数据元及定义专家共识[J]. 中国卒中杂志,2020,15(4):416-434. DOI:10.3969/j.issn.1673-5765.2020.04.01.
|
| [14] |
郭颖,张瑞生. 中国成人心脏瓣膜病超声心动图规范化检查专家共识[J]. 中国循环杂志,2021,36(2):109-125. DOI:10.3969/j.issn.1000-3614.2021.02.00.
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
梁峰,胡大一,方全,等. 基于指南的ST段抬高型心肌梗死后长期二级预防治疗与风险因素控制最新进展[J]. 中国全科医学,2019,22(8):888-900,908. DOI:10.12114/j.issn.1007-9572.2019.00.029.
|
| [19] |
|
| [20] |
高斯德,刘青波,丁晓松,等. ST段抬高型心肌梗死患者经皮冠状动脉介入治疗后近期和远期预后的性别差异[J]. 中国循环杂志,2019,34(7):646-652. DOI:10.3969/j.issn.1000-3614.2019.07.005.
|
| [21] |
梁峰,胡大一,方全,等. 急性ST段抬高型心肌梗死的再灌注治疗[J]. 中国循证心血管医学杂志,2019,11(3):263-274. DOI:10.3969/j.issn.1674-4055.2019.03.02.
|
| [22] |
|
| [23] |
|
| [24] |
吕俊兴,许海燕,杨跃进,等. 中国急性心肌梗死患者住院时间及其延长的影响因素分析[J]. 临床心血管病杂志,2020,36(10):890-894. DOI:10.13201/j.issn.1001-1439.2020.10.004.
|
| [25] |
|
| [26] |
|
| [27] |
|
| [28] |
|
| [29] |
|
| [30] |
|
| [31] |
郭超,罗晓亮,高晓津,等. 不同评分系统对急性心肌梗死合并心源性休克患者近期死亡预测价值的比较[J]. 中华心血管病杂志,2018,46(7):529-535. DOI:10.3760/cma.j.issn.0253-3758.2018.07.005.
|
| [32] |
高国峰,周林丽,张冬,等. ACEF评分在中国经皮冠状动脉介入治疗患者中的预测价值研究[J]. 中国循环杂志,2019,34(11):1047-1054. DOI:10.3969/j.issn.1000-3614.2019.11.002.
|
| [33] |
|
| [34] |
黄思壮,高斯德,林徐泽,等. TIMI危险评分对ST段抬高型冠状动脉非阻塞性心肌梗死患者远期预后的预测价值[J]. 中国循环杂志,2022,37(11):1091-1096. DOI:10.3969/j.issn.1000-3614.2022.11.003.
|
| [35] |
李相儒,左惠娟,杨红霞,等. 35岁及以下成年STEMI患者的临床特点及其预后研究[J]. 中华心血管病杂志,2021,49(11):1124-1129. DOI:10.3760/cma.j.cn112148-20210805-00672.
|
| [36] |
赵振燕,杨进刚,赵延延,等. 中国省、市和县级医院ST段抬高型心肌梗死住院患者就诊时间差异和延迟就诊的相关因素分析[J]. 中国循环杂志,2020,35(6):554-559. DOI:10.3969/j.issn.1000-3614.2020.06.006.
|
| [37] |
|
| [1] | 吴兰心, 张艳, 孟李雪, 刘莉, 赵婷. 老年共病患者自我管理现状及影响因素分析[J]. 中国全科医学, 2024, 27(21): 2565-2566. |
| [2] | 王晓霞, 曹学华, 李艳, 熊浪宇, 胡婉琴, 向凤, 贾钰. 中国维持性血液透析患者衰弱患病率及影响因素的Meta分析[J]. 中国全科医学, 2024, 27(20): 2534-2544. |
| [3] | 谢可欣, 杜芳, 张丹. 社区老年慢性病共病患者家庭医生签约服务成效影响因素研究[J]. 中国全科医学, 2024, 27(20): 2512-2519. |
| [4] | 李兴洋, 孙婉琪, 尹孟洁, 窦婷婷, 吕逸丽, 徐伟, 查震球. 慢性阻塞性肺疾病患者睡眠质量和焦虑抑郁情况及其影响因素:一项多中心横断面研究[J]. 中国全科医学, 2024, 27(20): 2437-2444. |
| [5] | 侯娜娜, 冯金章, 刘锁红, 冯俊芳, 薛小艳, 尹娜, 迟戈夫. 血尿酸/肌酐比值与代谢相关脂肪性肝病的相关性研究[J]. 中国全科医学, 2024, 27(20): 2476-2482. |
| [6] | 关新月, 王萧冉, 张丹. 老年共病患者服药依从性及其影响因素研究[J]. 中国全科医学, 2024, 27(20): 2520-2526. |
| [7] | 廖艳萍, 李云意, 周志衡, 王皓翔. 65岁及以上老年人群中基于脂肪组织过多引起的慢性疾病患病情况及影响因素分析[J]. 中国全科医学, 2024, 27(19): 2357-2363. |
| [8] | 荆冠宁, 邹颖, 禚小琪, 时司晏, 宋应柳, 姚弥, 迟春花, 李俊霞. 社区居民长期服用质子泵抑制剂和处方精简的现状及影响因素研究[J]. 中国全科医学, 2024, 27(19): 2344-2351. |
| [9] | 李静, 马雷雷, 王冠然, 姜晨, 邢海涛, 杨洪涛. 尿毒症腹膜透析相关胃肠功能紊乱的临床特征及影响因素研究[J]. 中国全科医学, 2024, 27(18): 2198-2204. |
| [10] | 马桂芬, 章倩, 刘娟, 孙菁, 林根来. Ⅲ期胃癌D2根治术后辅助放化疗患者长期预后的影响因素:基于10年随访数据[J]. 中国全科医学, 2024, 27(17): 2091-2097. |
| [11] | 徐苏, 蔡文玮, 李晨奕, 王光辉, 许又端. 社区老年人吞咽障碍现状及其影响因素:一项横断面研究[J]. 中国全科医学, 2024, 27(17): 2083-2090. |
| [12] | 周路路, 陆媛, 张怡, 高欣, 刘芳, 成园, 封玉琴, 于德华. 轻度认知障碍家庭照料者社会支持度及影响因素研究[J]. 中国全科医学, 2024, 27(16): 1977-1983. |
| [13] | 马佳, 张敏珏, 张韶伟, 于海燕, 陈慎, 古丽拜尔·马木提, 洪娟, 陆媛. 社区管理的老年2型糖尿病患者并发轻度认知功能障碍相关影响因素研究[J]. 中国全科医学, 2024, 27(16): 1984-1989. |
| [14] | 张曌, 郑婷婷, 王钰姝, 罗飞, 刘蕾. 退行性脊柱畸形患者的自我管理现状及影响因素研究[J]. 中国全科医学, 2024, 27(15): 1867-1872. |
| [15] | 赵帮豪, 袁腾, 赵翎, 阿曼古丽·如则, 尼鲁帕尔·谢甫开提, 马依彤, 杨毅宁, 高晓明. 预后营养指数与急性ST段抬高型心肌梗死合并2型糖尿病患者经皮冠状动脉介入术后院内主要不良心血管事件关系的研究[J]. 中国全科医学, 2024, 27(15): 1817-1824. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





