中国全科医学 ›› 2024, Vol. 27 ›› Issue (06): 670-678.DOI: 10.12114/j.issn.1007-9572.2023.0349
所属专题: 孕产妇健康研究最新文章合辑
袁仙仙1, 李静2, 王佳1, 张可欣1, 杨蕊华1, 郑薇1, 李光辉1,*( )
)
收稿日期:2023-06-18
修回日期:2023-08-09
出版日期:2024-02-20
发布日期:2023-11-21
通讯作者:
李光辉
基金资助:
YUAN Xianxian1, LI Jing2, WANG Jia1, ZHANG Kexin1, YANG Ruihua1, ZHENG Wei1, LI Guanghui1,*( )
)
Received:2023-06-18
Revised:2023-08-09
Published:2024-02-20
Online:2023-11-21
Contact:
LI Guanghui
摘要: 背景 妊娠期血脂异常升高可对母儿健康造成不良影响,不仅增加了子痫前期、妊娠期糖尿病(GDM)、高甘油三酯胰腺炎、晚期流产、早产以及巨大儿的发生风险,亦显著增加了母儿产后心血管疾病的风险。目的 分析妊娠早、中、晚期血脂异常的分布特征及其早期血脂水平对妊娠中、晚期血脂异常的预测价值。方法 本研究为单中心回顾性研究,纳入2018年1月—2019年6月在首都医科大学附属北京妇产医院产科建档产检至分娩的单胎孕妇,收集临床资料及妊娠早、中、晚期血脂数据[总胆固醇(TC)、三酰甘油(TG)、低密度脂蛋白胆固醇(LDL-C)、高密度脂蛋白胆固醇(HDL-C)]。以首都医科大学附属北京妇产医院妊娠期血脂参考范围作为血脂异常诊断标准:包括高总胆固醇血症、高甘油三酯血症、低高密度脂蛋白胆固醇血症和高低密度脂蛋白胆固醇血症。采用二分类Logistic回归分析妊娠早期血脂水平与妊娠中、晚期血脂异常的相关性,绘制受试者工作特征(ROC)曲线,计算曲线下面积(AUC),评价妊娠早期血脂水平对妊娠中、晚期血脂异常的预测价值,根据灵敏度和特异度确定最佳截断值。结果 研究共纳入单胎孕妇8 511名,平均年龄为(31.7±3.9)岁,平均孕前BMI为(21.7±3.2)kg/m2,其中孕前低体质量988名(11.6%)、正常体质量5 568名(65.4%)、超重1 271名(14.9%)、肥胖366名(4.3%),GDM孕妇1 415名(16.7%),妊娠期高血压疾病(HDP)孕妇650名(7.6%)。妊娠中、晚期TC、TG、LDL-C水平均高于妊娠早期(P<0.05),妊娠晚期HDL-C水平高于妊娠早期,但低于妊娠中期(P<0.05)。妊娠早期血脂异常患病率为23.4%(1 990/8 511),妊娠中、晚期血脂异常患病率低于妊娠早期(P<0.05)。孕前超重、肥胖孕妇妊娠早期血脂异常患病率高于孕前正常体质量孕妇,但妊娠晚期血脂异常患病率比较,差异无统计学意义(P>0.05);GDM组孕妇妊娠早、中期血脂异常患病率均高于非GDM孕妇,HDP孕妇妊娠早、中、晚期血脂异常患病率高于非HDP孕妇(P<0.05)。排除可能影响血脂的妊娠合并症及并发症后,妊娠早期预测妊娠中期血脂异常的最佳截断值分别为TC 4.485 mmol/L(AUC=0.854)、TG 1.325 mmol/L(AUC=0.864)、HDL-C 1.275 mmol/L(AUC=0.908)、LDL-C 2.265 mmol/L(AUC=0.823);妊娠早期预测妊娠晚期血脂异常的最佳截断值分别为TC 4.485 mmol/L(AUC=0.809)、TG 1.145 mmol/L(AUC=0.833)、HDL-C 1.285 mmol/L(AUC=0.851)、LDL-C 2.195 mmol/L(AUC=0.766)。结论 妊娠期血脂异常患病率并未增加,不同孕前BMI、GDM与非GDM、HDP与非HDP孕妇之间妊娠期血脂异常患病率具有显著差异,妊娠早期血脂水平有预测妊娠中晚期血脂异常的价值。
| 血脂 | 妊娠早期 | 妊娠中期 | 妊娠晚期 | Wald χ2值 | P值 |
|---|---|---|---|---|---|
| TC | 4.21(3.78,4.70) | 5.94(5.31,6.60)a | 6.38(5.70,7.17)ab | 34 945.567 | <0.001 |
| TG | 1.01(0.79,1.32) | 2.11(1.68,2.64)a | 2.86(2.32,3.58)ab | 22 692.258 | <0.001 |
| HDL-C | 1.45(1.27,1.65) | 1.88(1.65,2.14)a | 1.81(1.58,2.05)ab | 12 221.304 | <0.001 |
| LDL-C | 2.14(1.80,2.52) | 3.13(2.62,3.69)a | 3.43(2.80,4.09)ab | 13 782.571 | <0.001 |
表1 孕妇妊娠早、中、晚期血脂水平比较[M(P25,P75),mmol/L]
Table 1 Comparison of blood lipid levels in the first,second and third trimesters of pregnancy
| 血脂 | 妊娠早期 | 妊娠中期 | 妊娠晚期 | Wald χ2值 | P值 |
|---|---|---|---|---|---|
| TC | 4.21(3.78,4.70) | 5.94(5.31,6.60)a | 6.38(5.70,7.17)ab | 34 945.567 | <0.001 |
| TG | 1.01(0.79,1.32) | 2.11(1.68,2.64)a | 2.86(2.32,3.58)ab | 22 692.258 | <0.001 |
| HDL-C | 1.45(1.27,1.65) | 1.88(1.65,2.14)a | 1.81(1.58,2.05)ab | 12 221.304 | <0.001 |
| LDL-C | 2.14(1.80,2.52) | 3.13(2.62,3.69)a | 3.43(2.80,4.09)ab | 13 782.571 | <0.001 |
| 类别 | 妊娠早期 | 妊娠中期 | 妊娠晚期 | χ2值 | P值 |
|---|---|---|---|---|---|
| 未排除妊娠合并症及并发症(n=8 511) | |||||
| 血脂异常 | 1 990(23.4) | 1 659(19.5)a | 1 558(18.3)ab | 73.915 | <0.001 |
| 高总胆固醇血症 | 556(6.5) | 526(6.2) | 571(6.7) | 2.038 | 0.361 |
| 高甘油三酯血症 | 730(8.6) | 612(7.2)a | 678(8.0) | 11.281 | 0.004 |
| 低高密度脂蛋白胆固醇血症 | 802(9.4) | 425(5.0)a | 285(3.3)ab | 301.602 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 744(8.7) | 716(8.4) | 629(7.4)ab | 11.250 | 0.004 |
| 排除妊娠合并症及并发症后(n=5 336) | |||||
| 血脂异常 | 1 004(18.8) | 914(17.1)a | 908(17.0)a | 7.456 | 0.024 |
| 高总胆固醇血症 | 277(5.2) | 340(6.4)a | 382(7.2)a | 17.891 | <0.001 |
| 高甘油三酯血症 | 299(5.6) | 262(4.9) | 348(6.5)b | 13.023 | 0.001 |
| 低高密度脂蛋白胆固醇血症 | 420(7.9) | 187(3.5)a | 126(2.4)ab | 206.518 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 361(6.8) | 491(9.2)a | 435(8.2)a | 21.556 | <0.001 |
表2 孕妇妊娠各期血脂异常患病情况比较[名(%)]
Table 2 Comparison of the prevalence of dyslipidemia in pregnant women at various stages of pregnancy
| 类别 | 妊娠早期 | 妊娠中期 | 妊娠晚期 | χ2值 | P值 |
|---|---|---|---|---|---|
| 未排除妊娠合并症及并发症(n=8 511) | |||||
| 血脂异常 | 1 990(23.4) | 1 659(19.5)a | 1 558(18.3)ab | 73.915 | <0.001 |
| 高总胆固醇血症 | 556(6.5) | 526(6.2) | 571(6.7) | 2.038 | 0.361 |
| 高甘油三酯血症 | 730(8.6) | 612(7.2)a | 678(8.0) | 11.281 | 0.004 |
| 低高密度脂蛋白胆固醇血症 | 802(9.4) | 425(5.0)a | 285(3.3)ab | 301.602 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 744(8.7) | 716(8.4) | 629(7.4)ab | 11.250 | 0.004 |
| 排除妊娠合并症及并发症后(n=5 336) | |||||
| 血脂异常 | 1 004(18.8) | 914(17.1)a | 908(17.0)a | 7.456 | 0.024 |
| 高总胆固醇血症 | 277(5.2) | 340(6.4)a | 382(7.2)a | 17.891 | <0.001 |
| 高甘油三酯血症 | 299(5.6) | 262(4.9) | 348(6.5)b | 13.023 | 0.001 |
| 低高密度脂蛋白胆固醇血症 | 420(7.9) | 187(3.5)a | 126(2.4)ab | 206.518 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 361(6.8) | 491(9.2)a | 435(8.2)a | 21.556 | <0.001 |
| 类别 | 孕前低体质量组(n=988) | 孕前正常体质量组(n=5 568) | 孕前超重组(n=1 271) | 孕前肥胖组(n=366) | χ2值 | P值 |
|---|---|---|---|---|---|---|
| 妊娠早期 | ||||||
| 血脂异常 | 90(9.1) | 1 129(20.3)a | 515(40.5)ab | 182(49.7)abc | 492.418 | <0.001 |
| 高总胆固醇血症 | 33(3.3) | 350(6.3)a | 117(9.2)ab | 33(9.0)ab | 35.743 | <0.001 |
| 高甘油三酯血症 | 22(2.2) | 370(6.6)a | 220(17.3)ab | 83(22.7)abc | 296.572 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 30(3.0) | 431(7.7)a | 237(18.6)ab | 78(21.3)ab | 251.796 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 29(2.9) | 425(7.6)a | 189(14.9)ab | 77(21.0)abc | 178.670 | <0.001 |
| 妊娠中期 | ||||||
| 血脂异常 | 148(15.0) | 1 053(18.9)a | 326(25.6)ab | 78(21.3)a | 45.268 | <0.001 |
| 高总胆固醇血症 | 77(7.8) | 385(6.9) | 50(3.9)ab | 9(2.5)ab | 28.201 | <0.001 |
| 高甘油三酯血症 | 21(2.1) | 355(6.4)a | 164(12.9)ab | 46(12.6)ab | 122.115 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 12(1.2) | 229(4.1)a | 129(10.1)ab | 33(9.0)ab | 124.215 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 109(11.0) | 514(9.2) | 77(6.1)ab | 10(2.7)abc | 36.440 | <0.001 |
| 妊娠晚期 | ||||||
| 血脂异常 | 174(17.6) | 1 016(18.2) | 261(20.5) | 55(15.0) | 7.131 | 0.068 |
| 高总胆固醇血症 | 102(10.3) | 398(7.1)a | 50(3.9)ab | 9(2.5)ab | 47.624 | <0.001 |
| 高甘油三酯血症 | 39(3.9) | 437(7.8)a | 143(11.3)ab | 34(9.3)a | 41.431 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 17(1.7) | 161(2.9)a | 80(6.3)ab | 12(3.3)c | 46.405 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 112(11.3) | 433(7.8)a | 61(4.8)ab | 11(3.0)ab | 45.407 | <0.001 |
表3 孕前不同BMI分组孕妇妊娠早、中、晚期血脂异常患病情况比较[名(%)]
Table 3 Comparison of the prevalence of dyslipidemia in pregnant women with different pre-pregnancy BMI subgroups in the first,second and third trimesters of pregnancy
| 类别 | 孕前低体质量组(n=988) | 孕前正常体质量组(n=5 568) | 孕前超重组(n=1 271) | 孕前肥胖组(n=366) | χ2值 | P值 |
|---|---|---|---|---|---|---|
| 妊娠早期 | ||||||
| 血脂异常 | 90(9.1) | 1 129(20.3)a | 515(40.5)ab | 182(49.7)abc | 492.418 | <0.001 |
| 高总胆固醇血症 | 33(3.3) | 350(6.3)a | 117(9.2)ab | 33(9.0)ab | 35.743 | <0.001 |
| 高甘油三酯血症 | 22(2.2) | 370(6.6)a | 220(17.3)ab | 83(22.7)abc | 296.572 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 30(3.0) | 431(7.7)a | 237(18.6)ab | 78(21.3)ab | 251.796 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 29(2.9) | 425(7.6)a | 189(14.9)ab | 77(21.0)abc | 178.670 | <0.001 |
| 妊娠中期 | ||||||
| 血脂异常 | 148(15.0) | 1 053(18.9)a | 326(25.6)ab | 78(21.3)a | 45.268 | <0.001 |
| 高总胆固醇血症 | 77(7.8) | 385(6.9) | 50(3.9)ab | 9(2.5)ab | 28.201 | <0.001 |
| 高甘油三酯血症 | 21(2.1) | 355(6.4)a | 164(12.9)ab | 46(12.6)ab | 122.115 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 12(1.2) | 229(4.1)a | 129(10.1)ab | 33(9.0)ab | 124.215 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 109(11.0) | 514(9.2) | 77(6.1)ab | 10(2.7)abc | 36.440 | <0.001 |
| 妊娠晚期 | ||||||
| 血脂异常 | 174(17.6) | 1 016(18.2) | 261(20.5) | 55(15.0) | 7.131 | 0.068 |
| 高总胆固醇血症 | 102(10.3) | 398(7.1)a | 50(3.9)ab | 9(2.5)ab | 47.624 | <0.001 |
| 高甘油三酯血症 | 39(3.9) | 437(7.8)a | 143(11.3)ab | 34(9.3)a | 41.431 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 17(1.7) | 161(2.9)a | 80(6.3)ab | 12(3.3)c | 46.405 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 112(11.3) | 433(7.8)a | 61(4.8)ab | 11(3.0)ab | 45.407 | <0.001 |
| 类别 | GDM组(n=1 415) | 非GDM组(n=7 069) | χ2值 | P值 |
|---|---|---|---|---|
| 妊娠早期 | ||||
| 血脂异常 | 498(35.2) | 1 481(21.0) | 133.742 | <0.001 |
| 高总胆固醇血症 | 131(9.3) | 416(5.9) | 22.240 | <0.001 |
| 高甘油三酯血症 | 245(17.3) | 484(6.8) | 164.478 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 194(13.7) | 608(8.6) | 35.958 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 199(14.1) | 535(7.6) | 62.939 | <0.001 |
| 妊娠中期 | ||||
| 血脂异常 | 363(25.7) | 1 273(18.0) | 44.277 | <0.001 |
| 高总胆固醇血症 | 66(4.7) | 440(6.2) | 5.116 | 0.024 |
| 高甘油三酯血症 | 204(14.4) | 406(5.7) | 132.919 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 136(9.6) | 288(4.1) | 76.136 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 76(5.4) | 620(8.8) | 18.095 | <0.001 |
| 妊娠晚期 | ||||
| 血脂异常 | 270(19.1) | 1 270(18.0) | 0.987 | 0.320 |
| 高总胆固醇血症 | 66(4.7) | 491(6.9) | 10.004 | 0.002 |
| 高甘油三酯血症 | 156(11.0) | 520(7.4) | 21.639 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 79(5.6) | 206(2.9) | 25.869 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 58(4.1) | 558(7.9) | 25.213 | <0.001 |
表4 GDM组与非GDM组孕妇妊娠早、中、晚期血脂异常患病情况比较[名(%)]
Table 4 Comparison of the prevalence of dyslipidemia in the first,second and third trimesters of pregnancy between the GDM and non-GDM pregnant women
| 类别 | GDM组(n=1 415) | 非GDM组(n=7 069) | χ2值 | P值 |
|---|---|---|---|---|
| 妊娠早期 | ||||
| 血脂异常 | 498(35.2) | 1 481(21.0) | 133.742 | <0.001 |
| 高总胆固醇血症 | 131(9.3) | 416(5.9) | 22.240 | <0.001 |
| 高甘油三酯血症 | 245(17.3) | 484(6.8) | 164.478 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 194(13.7) | 608(8.6) | 35.958 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 199(14.1) | 535(7.6) | 62.939 | <0.001 |
| 妊娠中期 | ||||
| 血脂异常 | 363(25.7) | 1 273(18.0) | 44.277 | <0.001 |
| 高总胆固醇血症 | 66(4.7) | 440(6.2) | 5.116 | 0.024 |
| 高甘油三酯血症 | 204(14.4) | 406(5.7) | 132.919 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 136(9.6) | 288(4.1) | 76.136 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 76(5.4) | 620(8.8) | 18.095 | <0.001 |
| 妊娠晚期 | ||||
| 血脂异常 | 270(19.1) | 1 270(18.0) | 0.987 | 0.320 |
| 高总胆固醇血症 | 66(4.7) | 491(6.9) | 10.004 | 0.002 |
| 高甘油三酯血症 | 156(11.0) | 520(7.4) | 21.639 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 79(5.6) | 206(2.9) | 25.869 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 58(4.1) | 558(7.9) | 25.213 | <0.001 |
| 血脂异常分类 | HDP组(n=650) | 非HDP组(n=7 861) | χ2值 | P值 |
|---|---|---|---|---|
| 妊娠早期 | ||||
| 血脂异常 | 239(36.8) | 1 751(22.3) | 70.408 | <0.001 |
| 高总胆固醇血症 | 69(10.6) | 487(6.2) | 19.211 | <0.001 |
| 高甘油三酯血症 | 106(16.3) | 624(7.9) | 53.634 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 99(15.2) | 703(8.9) | 27.810 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 98(15.1) | 646(8.2) | 35.407 | <0.001 |
| 妊娠中期 | ||||
| 血脂异常 | 209(32.2) | 1 450(18.4) | 71.892 | <0.001 |
| 高总胆固醇血症 | 60(9.2) | 466(5.9) | 11.295 | 0.001 |
| 高甘油三酯血症 | 102(15.7) | 510(6.5) | 76.218 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 59(9.1) | 366(4.7) | 24.734 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 71(10.9) | 645(8.2) | 5.756 | 0.016 |
| 妊娠晚期 | ||||
| 血脂异常 | 180(27.7) | 1 378(17.5) | 41.462 | <0.001 |
| 高总胆固醇血症 | 56(8.6) | 515(6.6) | 4.087 | 0.043 |
| 高甘油三酯血症 | 101(15.5) | 577(7.3) | 55.040 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 35(5.4) | 250(3.2) | 9.014 | 0.003 |
| 高低密度脂蛋白胆固醇血症 | 56(8.6) | 573(7.3) | 1.543 | 0.214 |
表5 HDP组与非HDP组孕妇妊娠早、中、晚期血脂异常患病情况比较[名(%)]
Table 5 Comparison of the prevalence of dyslipidemia in the first,second and third trimesters of pregnancy between HDP and non-HDP pregnant women
| 血脂异常分类 | HDP组(n=650) | 非HDP组(n=7 861) | χ2值 | P值 |
|---|---|---|---|---|
| 妊娠早期 | ||||
| 血脂异常 | 239(36.8) | 1 751(22.3) | 70.408 | <0.001 |
| 高总胆固醇血症 | 69(10.6) | 487(6.2) | 19.211 | <0.001 |
| 高甘油三酯血症 | 106(16.3) | 624(7.9) | 53.634 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 99(15.2) | 703(8.9) | 27.810 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 98(15.1) | 646(8.2) | 35.407 | <0.001 |
| 妊娠中期 | ||||
| 血脂异常 | 209(32.2) | 1 450(18.4) | 71.892 | <0.001 |
| 高总胆固醇血症 | 60(9.2) | 466(5.9) | 11.295 | 0.001 |
| 高甘油三酯血症 | 102(15.7) | 510(6.5) | 76.218 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 59(9.1) | 366(4.7) | 24.734 | <0.001 |
| 高低密度脂蛋白胆固醇血症 | 71(10.9) | 645(8.2) | 5.756 | 0.016 |
| 妊娠晚期 | ||||
| 血脂异常 | 180(27.7) | 1 378(17.5) | 41.462 | <0.001 |
| 高总胆固醇血症 | 56(8.6) | 515(6.6) | 4.087 | 0.043 |
| 高甘油三酯血症 | 101(15.5) | 577(7.3) | 55.040 | <0.001 |
| 低高密度脂蛋白胆固醇血症 | 35(5.4) | 250(3.2) | 9.014 | 0.003 |
| 高低密度脂蛋白胆固醇血症 | 56(8.6) | 573(7.3) | 1.543 | 0.214 |
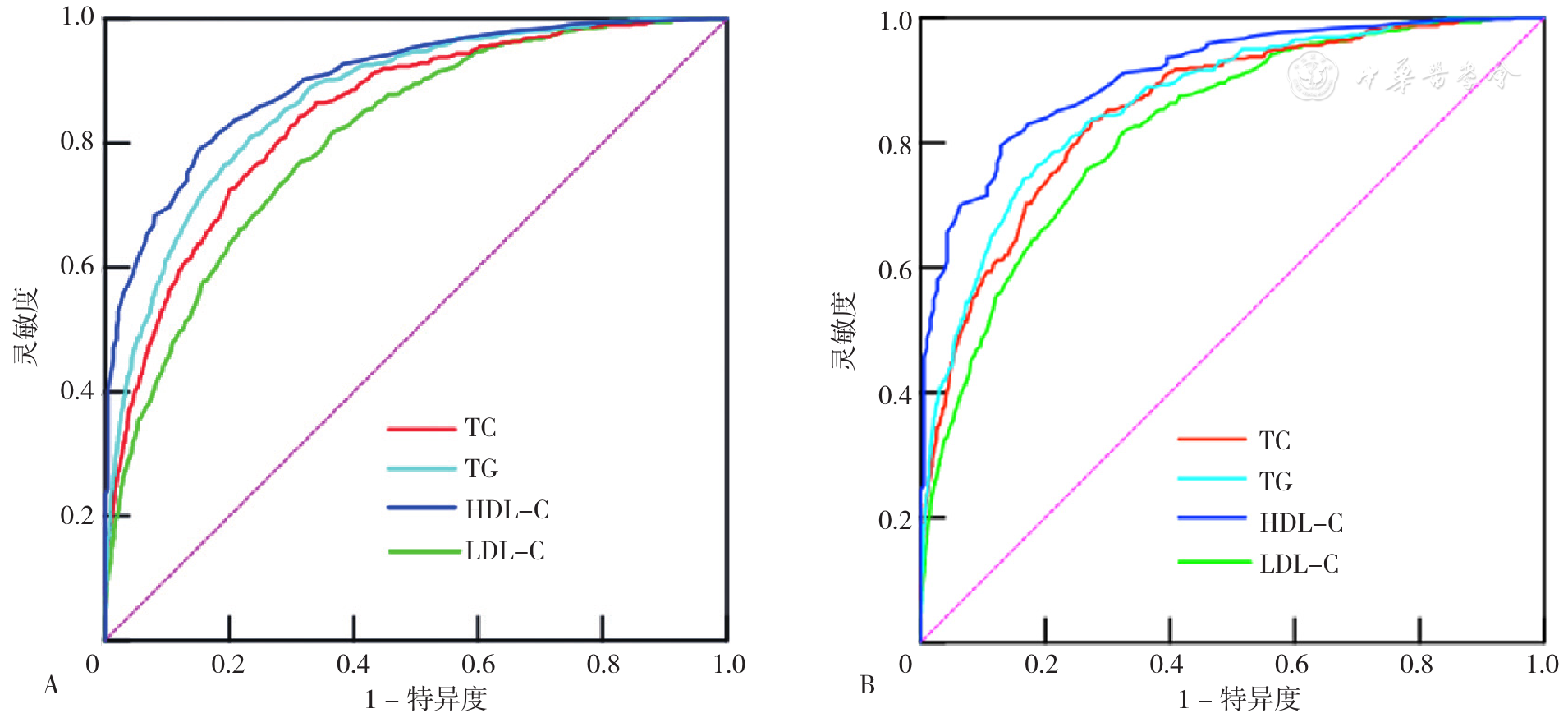
图1 妊娠早期血脂水平预测妊娠中期血脂异常的ROC曲线注:A图为未排除妊娠合并症及并发症的ROC曲线,B图为排除妊娠合并症及并发症后的ROC曲线;TC=总胆固醇,TG=三酰甘油,HDL-C=高密度脂蛋白胆固醇,LDL-C=低密度脂蛋白胆固醇。
Figure 1 ROC curves of blood lipid level in the first trimester of pregnancy to predict dyslipidemia in the second trimester of pregnancy
| 血脂 | 最佳截断值(mmol/L) | AUC | 灵敏度 | 特异度 |
|---|---|---|---|---|
| 未排除妊娠合并症及并发症 | ||||
| TC | 4.485 | 0.844 | 0.686 | 0.844 |
| TG | 1.275 | 0.870 | 0.765 | 0.810 |
| HDL-C | 1.285 | 0.899 | 0.791 | 0.847 |
| LDL-C | 2.355 | 0.804 | 0.685 | 0.765 |
| 排除妊娠合并症及并发症后 | ||||
| TC | 4.485 | 0.854 | 0.724 | 0.838 |
| TG | 1.325 | 0.864 | 0.835 | 0.740 |
| HDL-C | 1.275 | 0.908 | 0.795 | 0.872 |
| LDL-C | 2.265 | 0.823 | 0.673 | 0.819 |
表6 妊娠早期血脂水平预测妊娠中期血脂异常的临床价值
Table 6 Clinical values of blood lipid level in the first trimester of pregnancy to predict dyslipidemia in the second trimester of pregnancy
| 血脂 | 最佳截断值(mmol/L) | AUC | 灵敏度 | 特异度 |
|---|---|---|---|---|
| 未排除妊娠合并症及并发症 | ||||
| TC | 4.485 | 0.844 | 0.686 | 0.844 |
| TG | 1.275 | 0.870 | 0.765 | 0.810 |
| HDL-C | 1.285 | 0.899 | 0.791 | 0.847 |
| LDL-C | 2.355 | 0.804 | 0.685 | 0.765 |
| 排除妊娠合并症及并发症后 | ||||
| TC | 4.485 | 0.854 | 0.724 | 0.838 |
| TG | 1.325 | 0.864 | 0.835 | 0.740 |
| HDL-C | 1.275 | 0.908 | 0.795 | 0.872 |
| LDL-C | 2.265 | 0.823 | 0.673 | 0.819 |
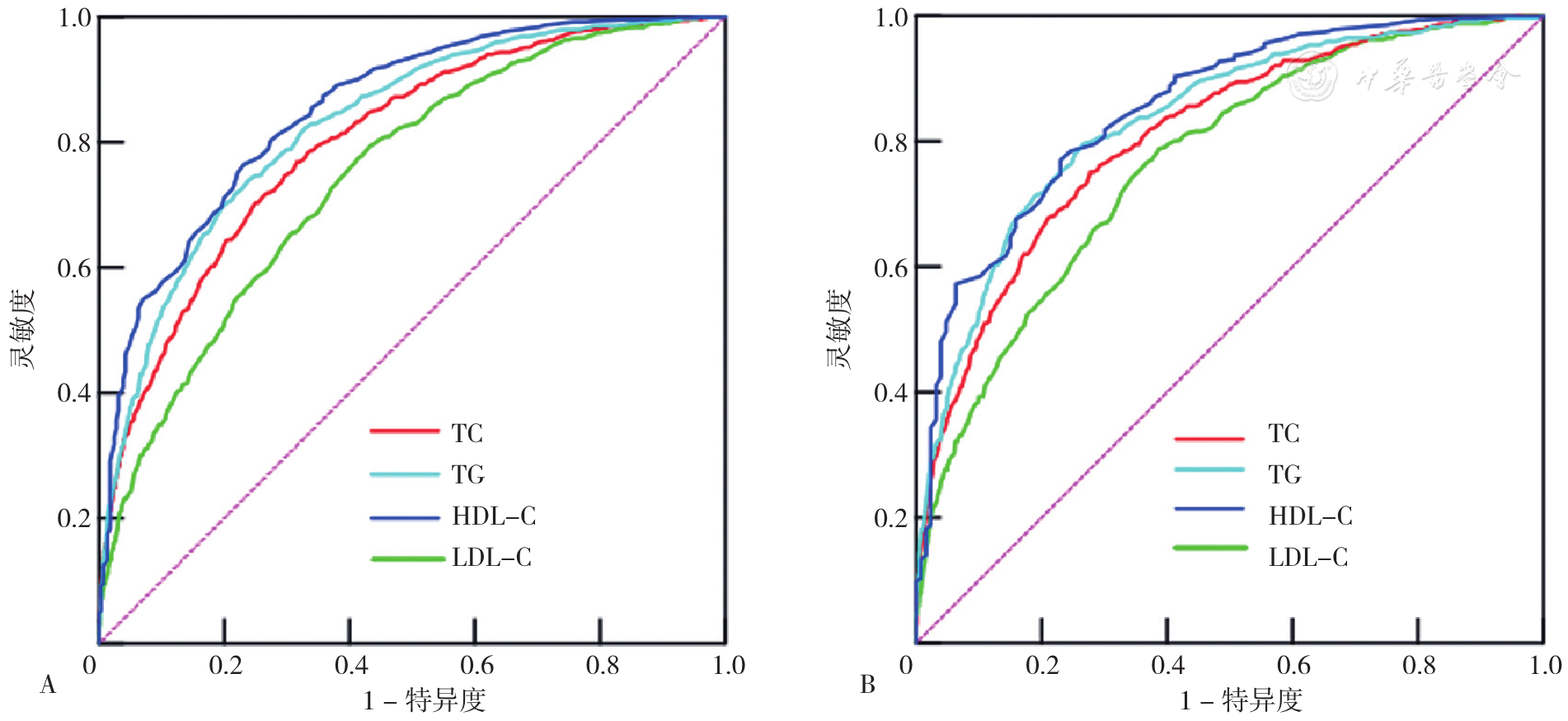
图2 妊娠早期血脂水平预测妊娠晚期血脂异常的ROC曲线注:A图为未排除妊娠合并症及并发症的ROC曲线,B图为排除妊娠合并症及并发症后的ROC曲线。
Figure 2 ROC curves of blood lipid level in the first trimester of pregnancy to predict dyslipidemia in the third trimester of pregnancy
| 血脂 | 最佳截断值(mmol/L) | AUC | 灵敏度 | 特异度 |
|---|---|---|---|---|
| 未排除妊娠合并症及并发症 | ||||
| TC | 4.635 | 0.802 | 0.750 | 0.704 |
| TG | 1.335 | 0.828 | 0.800 | 0.701 |
| HDL-C | 1.275 | 0.852 | 0.765 | 0.768 |
| LDL-C | 2.195 | 0.747 | 0.567 | 0.795 |
| 排除妊娠合并症及并发症后 | ||||
| TC | 4.485 | 0.809 | 0.722 | 0.751 |
| TG | 1.145 | 0.833 | 0.733 | 0.796 |
| HDL-C | 1.285 | 0.851 | 0.771 | 0.770 |
| LDL-C | 2.195 | 0.766 | 0.612 | 0.789 |
表7 妊娠早期血脂水平预测妊娠晚期血脂异常的临床价值
Table 7 Clinical values of blood lipid level in the first trimester of pregnancy to predict dyslipidemia in the third trimester of pregnancy
| 血脂 | 最佳截断值(mmol/L) | AUC | 灵敏度 | 特异度 |
|---|---|---|---|---|
| 未排除妊娠合并症及并发症 | ||||
| TC | 4.635 | 0.802 | 0.750 | 0.704 |
| TG | 1.335 | 0.828 | 0.800 | 0.701 |
| HDL-C | 1.275 | 0.852 | 0.765 | 0.768 |
| LDL-C | 2.195 | 0.747 | 0.567 | 0.795 |
| 排除妊娠合并症及并发症后 | ||||
| TC | 4.485 | 0.809 | 0.722 | 0.751 |
| TG | 1.145 | 0.833 | 0.733 | 0.796 |
| HDL-C | 1.285 | 0.851 | 0.771 | 0.770 |
| LDL-C | 2.195 | 0.766 | 0.612 | 0.789 |
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
中国心血管健康与疾病报告编写组. 中国心血管健康与疾病报告2020概要[J]. 中国循环杂志,2021,36(6):521-545. DOI:10.3969/j.issn.1000-3614.2021.06.001.
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
张一帆,李根霞,王蕊杰,等. 妊娠期血脂变化情况及血脂参考范围的建立[J]. 医药论坛杂志,2021,42(14):1-4.
|
| [14] | |
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [21] |
|
| [22] |
|
| [23] |
|
| [24] |
|
| [25] |
International Weight Management in Pregnancy(I-WIP) Collaborative Group. Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes:meta-analysis of individual participant data from randomised trials[J]. BMJ,2017,358:j3119. DOI:10.1136/bmj.j3119.
|
| [26] |
|
| [27] |
|
| [28] |
|
| [29] |
|
| [30] |
|
| [1] | 陈俊屿, 韩广莉, 李春宏, 陈衣迪, 杨娜娜, 罗小茜. 基于聚类分析的农村女性妊娠期自我管理类型及特征研究[J]. 中国全科医学, 2025, 28(26): 3289-3293. |
| [2] | 顾小林, 陈俊屿, 陈丹, 韩广莉, 陈衣迪, 李春宏, 罗小茜. 农村女性妊娠期负性情绪体验的质性研究[J]. 中国全科医学, 2025, 28(26): 3283-3288. |
| [3] | 罗新宇, 刘瑾, 陈海龙. 1990—2021年中国和全球胰腺炎疾病负担趋势分析及2022—2031年预测研究[J]. 中国全科医学, 2025, 28(26): 3321-3327. |
| [4] | 余孜孜, 刘杜丽, 李熙敏, 阮春怡, 尹向阳, 蔡乐. 农村高血压患病和自我管理现状及影响因素研究[J]. 中国全科医学, 2025, 28(25): 3137-3143. |
| [5] | 蒋世华, 朱政, 任盈盈, 朱垚磊, 王越, 高希彬. 中国儿童青少年近视患病率及影响因素的Meta分析[J]. 中国全科医学, 2025, 28(24): 3043-3052. |
| [6] | 王碧晴, 张萍, 杨红霞, 王倩, 鞠春晓, 赵俊男, 梅俊, 张颖, 徐凤芹. 中国老年高血压患者轻度认知障碍患病率及发展趋势的Meta分析[J]. 中国全科医学, 2025, 28(17): 2186-2192. |
| [7] | 陈兴超, 高振华, 徐生刚, 邹永刚, 钱军, 魏建仝. 1990—2021年全球和中国及不同社会人口学指数地区骨关节炎疾病负担趋势分析[J]. 中国全科医学, 2025, 28(17): 2172-2178. |
| [8] | 黄志杰, 麦志华, 王皓翔, 何煜明, 邓巧妍, 戴燃然, 周志衡. 老年"三高"共患情况和家庭功能的现状及影响因素研究[J]. 中国全科医学, 2025, 28(16): 2001-2010. |
| [9] | 令垚, 张文滨, 王仕鸿, 陈永泽, 董文娇, 邓星妤, 丁元林. 1990—2021年中国类风湿关节炎疾病负担变化趋势分析及预测研究[J]. 中国全科医学, 2025, 28(15): 1914-1922. |
| [10] | 汪蝶, 吴帮云, 谭存瑶, 谌世晖, 李游, 蒙玥, 王大珊, 胡瑾, 王子云, 汪俊华. 40~65岁人群睡眠效率与血脂异常关联性研究[J]. 中国全科医学, 2025, 28(13): 1601-1606. |
| [11] | 张滢, 姜欣彤, 王萍玉. 基于健康生态学模型的中国女性老年人群抑郁症状影响因素研究[J]. 中国全科医学, 2025, 28(13): 1595-1600. |
| [12] | 孙清, 吴玉霄, 崔立敏. 中国2型糖尿病患者肌少-骨质疏松症患病率的Meta分析[J]. 中国全科医学, 2025, 28(12): 1520-1526. |
| [13] | 陈鸿旭, 王登兰, 陈媛媛, 沈娟娟, 宋春, 王帆, 孔田甜. 残余胆固醇与妊娠中期孕妇抑郁和妊娠压力的关系研究[J]. 中国全科医学, 2025, 28(11): 1347-1353. |
| [14] | 朱先尚, 曾泓钰, 吕凤丽, 王建成. 甘肃省60岁及以上老年人慢性病共病现状及影响因素研究[J]. 中国全科医学, 2025, 28(10): 1193-1199. |
| [15] | 赵新蕊, 黄丽, 曹立春, 屈会超, 张美琳, 刘欢. 社区老年人可逆与潜在可逆性认知衰弱情况及影响因素研究[J]. 中国全科医学, 2025, 28(07): 824-830. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





