| [30] |
CELLI B R, FABBRI L M, AARON S D, et al. Differential diagnosis of suspected chronic obstructive pulmonary disease exacerbations in the acute care setting:best practice[J]. Am J Respir Crit Care Med, 2023, 207(9):1134-1144. DOI: 10.1164/rccm.202209-1795ci.
|
| [31] |
|
| [32] |
VESTBO J, EDWARDS L D, SCANLON P D, et al. Changes in forced expiratory volume in 1 second over time in COPD[J]. N Engl J Med,2011,365(13):1184-1192.
|
| [33] |
MARTÍNEZ-GARCÍA M Á, DE LA ROSA-CARRILLO D, SOLER-CATALUÑA J J, et al. Bronchial infection and temporal evolution of bronchiectasis in patients with chronic obstructive pulmonary disease[J]. Clin Infect Dis, 2021, 72(3):403-410. DOI: 10.1093/cid/ciaa069.
|
| [34] |
DIAZ A A, OREJAS J L, GRUMLEY S, et al. Airway-occluding mucus plugs and mortality in patients with chronic obstructive pulmonary disease[J]. JAMA, 2023, 329(21):1832. DOI: 10.1001/jama.2023.2065.
|
| [35] |
EZPONDA A, CASANOVA C, DIVO M, et al. Chest CT-assessed comorbidities and all-cause mortality risk in COPD patients in the BODE cohort[J]. Respirology, 2022, 27(4):286-293. DOI: 10.1111/resp.14223.
|
| [36] |
DAVIE G S, BAKER M G, HALES S, et al. Trends and determinants of excess winter mortality in New Zealand:1980 to 2000[J]. BMC Public Health,2007,7:263.
|
| [37] |
BURKART K G, BRAUER M, ARAVKIN A Y, et al. Estimating the cause-specific relative risks of non-optimal temperature on daily mortality:a two-part modelling approach applied to the Global Burden of Disease Study[J]. Lancet, 2021, 398(10301):685-697. DOI: 10.1016/S0140-6736(21)01700-1.
|
| [38] |
TSENG C M, CHEN Y T, OU S M, et al. The effect of cold temperature on increased exacerbation of chronic obstructive pulmonary disease:a nationwide study[J]. PLoS One, 2013, 8(3):e57066. DOI: 10.1371/journal.pone.0057066.
|
| [39] |
SCHEERENS C, NURHUSSIEN L, AGLAN A, et al. The impact of personal and outdoor temperature exposure during cold and warm seasons on lung function and respiratory symptoms in COPD[J]. ERJ Open Res, 2022, 8(1):00574-02021. DOI: 10.1183/23120541.00574-2021.
|
| [40] |
MCCORMACK M C, PAULIN L M, GUMMERSON C E, et al. Colder temperature is associated with increased COPD morbidity[J]. Eur Respir J, 2017, 49(6):1601501. DOI: 10.1183/13993003.01501-2016.
|
| [41] |
MU Z, CHEN P L, GENG F H, et al. Synergistic effects of temperature and humidity on the symptoms of COPD patients[J]. Int J Biometeorol, 2017, 61(11):1919-1925. DOI: 10.1007/s00484-017-1379-0.
|
| [42] |
OSMAN L M, AYRES J G, GARDEN C, et al. Home warmth and health status of COPD patients[J]. Eur J Public Health, 2008, 18(4):399-405. DOI: 10.1093/eurpub/ckn015.
|
| [43] |
DE SARIO M, KATSOUYANNI K, MICHELOZZI P. Climate change,extreme weather events,air pollution and respiratory health in Europe[J]. Eur Respir J, 2013, 42(3):826-843. DOI: 10.1183/09031936.00074712.
|
| [44] |
ANENBERG S C, HAINES S, WANG E, et al. Synergistic health effects of air pollution,temperature,and pollen exposure:a systematic review of epidemiological evidence[J]. Environ Health,2020,19(1):130.
|
| [45] |
QIU H, TAN K, LONG F Y, et al. The burden of COPD morbidity attributable to the interaction between ambient air pollution and temperature in Chengdu,China[J]. Int J Environ Res Public Health, 2018, 15(3):492. DOI: 10.3390/ijerph15030492.
|
| [46] |
MCCORMACK M C, BELLI A J, WAUGH D, et al. Respiratory effects of indoor heat and the interaction with air pollution in chronic obstructive pulmonary disease[J]. Ann Am Thorac Soc, 2016, 13(12):2125-2131. DOI: 10.1513/annalsats.201605-329oc.
|
| [47] |
PLATT H, OMOLE T, CARDONA J, et al. Safety,tolerability,and immunogenicity of a 21-valent pneumococcal conjugate vaccine,V116,in healthy adults:phase 1/2,randomised,double-blind,active comparator-controlled,multicentre,US-based trial[J]. Lancet Infect Dis,2023,23(2):233-246.
|
| [1] |
Global strategy for prevention,diagnosis and management of COPD:2025[EB/OL].[2024-12-16].
|
| [2] |
|
| [3] |
|
| [4] |
KOHANSAL R, MARTINEZ-CAMBLOR P, MARTINEZ-CAMBLOR P, et al. The natural history of chronic airflow obstruction revisited:an analysis of the Framingham offspring cohort[J]. Am J Respir Crit Care Med,2009,180(1):3-10.
|
| [5] |
|
| [6] |
ÇOLAK Y, NORDESTGAARD B G, VESTBO J, et al. Relationship between supernormal lung function and long-term risk of hospitalisations and mortality:a population-based cohort study[J]. Eur Respir J, 2021, 57(4):2004055. DOI: 10.1183/13993003.04055-2020.
|
| [7] |
AGUSTI A, FABBRI L M, BARALDI E, et al. Spirometry:a practical lifespan predictor of global health and chronic respiratory and non-respiratory diseases[J]. Eur J Intern Med, 2021, 89:3-9. DOI: 10.1016/j.ejim.2021.04.027.
|
| [8] |
MELÉN E, FANER R, ALLINSON J P, et al. Lung-function trajectories:relevance and implementation in clinical practice[J]. Lancet, 2024, 403(10435):1494-1503. DOI: 10.1016/s0140-6736(24)00016-3.
|
| [9] |
COLLABORATION E C. Lungtracker website:lung function tracker[EB/OL].[2024-12-16].
|
| [10] |
SONG Z, MENG Y F, FRICKER M, et al. The role of gut-lung axis in COPD:pathogenesis,immune response,and prospective treatment[J]. Heliyon, 2024, 10(9):e30612. DOI: 10.1016/j.heliyon.2024.e30612.
|
| [11] |
DICKER A J, HUANG J T J, LONERGAN M, et al. The sputum microbiome,airway inflammation,and mortality in chronic obstructive pulmonary disease[J]. J Allergy Clin Immunol, 2021, 147(1):158-167. DOI: 10.1016/j.jaci.2020.02.040.
|
| [48] |
WISEMAN D J, THWAITES R S, RITCHIE A I, et al. Respiratory syncytial virus-related community chronic obstructive pulmonary disease exacerbations and novel diagnostics:a binational prospective cohort study[J]. Am J Respir Crit Care Med, 2024, 210(8):994-1001. DOI: 10.1164/rccm.202308-1320oc.
|
| [49] |
THOMPSON M G, STENEHJEM E, GRANNIS S, et al. Effectiveness of covid-19 vaccines in ambulatory and inpatient care settings[J]. N Engl J Med, 2021, 385(15):1355-1371. DOI: 10.1056/nejmoa2110362.
|
| [50] |
KARNER C, CATES C J. Long-acting beta(2)-agonist in addition to tiotropium versus either tiotropium or long-acting beta(2)-agonist alone for chronic obstructive pulmonary disease[J]. Cochrane Database Syst Rev, 2012, 4(4):CD008989. DOI: 10.1002/14651858.CD008989.pub2.
|
| [51] |
LIPSON D A, BARNHART F, BREALEY N, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD[J]. N Engl J Med,2018,378(18):1671-1680.
|
| [52] |
Azithromycin for prevention of exacerbations of COPD[J]. N Engl J Med, 2011, 365(23):2234-2237. DOI: 10.1056/nejmc1111248. |
| [53] |
HAN M K, TAYOB N, MURRAY S, et al. Predictors of chronic obstructive pulmonary disease exacerbation reduction in response to daily azithromycin therapy[J]. Am J Respir Crit Care Med,2014,189(12):1503-1508.
|
| [54] |
MARTINEZ F J, CALVERLEY P M, GOEHRING U M, et al. Effect of roflumilast on exacerbations in patients with severe chronic obstructive pulmonary disease uncontrolled by combination therapy(REACT):a multicentre randomised controlled trial[J]. Lancet,2015,385(9971):857-866.
|
| [55] |
BHATT S P, RABE K F, HANANIA N A, et al. Dupilumab for COPD with blood eosinophil evidence of type 2 inflammation[J]. N Engl J Med, 2024, 390(24):2274-2283. DOI: 10.1056/nejmoa2401304.
|
| [56] |
CHAPMAN K R, HURST J R, FRENT S M, et al. Long-term triple therapy de-escalation to indacaterol/glycopyrronium in patients with chronic obstructive pulmonary disease(SUNSET):a randomized,double-blind,triple-dummy clinical trial[J]. Am J Respir Crit Care Med, 2018, 198(3):329-339. DOI: 10.1164/rccm.201803-0405oc.
|
| [12] |
KAYONGO A, ROBERTSON N M, SIDDHARTHAN T, et al. Airway microbiome-immune crosstalk in chronic obstructive pulmonary disease[J]. Front Immunol,2022,13:1085551.
|
| [13] |
SULAIMAN I, WU B G, CHUNG M, et al. Lower airway dysbiosis augments lung inflammatory injury in mild-to-moderate chronic obstructive pulmonary disease[J]. Am J Respir Crit Care Med, 2023, 208(10):1101-1114. DOI: 10.1164/rccm.202210-1865oc.
|
| [14] |
LEA S, HIGHAM A, BEECH A, et al. How inhaled corticosteroids target inflammation in COPD[J]. Eur Respir Rev, 2023, 32(170):230084. DOI: 10.1183/16000617.0084-2023.
|
| [15] |
WANG Z, BAFADHEL M, HALDAR K, et al. Lung microbiome dynamics in COPD exacerbations[J]. Eur Respir J, 2016, 47(4):1082-1092. DOI: 10.1183/13993003.01406-2015.
|
| [16] |
WANG Z, LOCANTORE N, HALDAR K, et al. Inflammatory endotype-associated airway microbiome in chronic obstructive pulmonary disease clinical stability and exacerbations:a multicohort longitudinal analysis[J]. Am J Respir Crit Care Med, 2021, 203(12):1488-1502. DOI: 10.1164/rccm.202009-3448oc.
|
| [17] |
OPRON K, BEGLEY L A, ERB-DOWNWARD J R, et al. Loss of airway phylogenetic diversity is associated with clinical and pathobiological markers of disease development in chronic obstructive pulmonary disease[J]. Am J Respir Crit Care Med, 2024, 210(2):186-200. DOI: 10.1164/rccm.202303-0489oc.
|
| [18] |
BUHR R G, BARJAKTAREVIC I Z, QUIBRERA P M, et al. Reversible airflow obstruction predicts future chronic obstructive pulmonary disease development in the SPIROMICS cohort:an observational cohort study[J]. Am J Respir Crit Care Med, 2022, 206(5):554-562. DOI: 10.1164/rccm.202201-0094oc.
|
| [19] |
AARON S D, TAN W C, BOURBEAU J, et al. Diagnostic instability and reversals of chronic obstructive pulmonary disease diagnosis in individuals with mild to moderate airflow obstruction[J]. Am J Respir Crit Care Med,2017,196(3):306-314.
|
| [20] |
GÜDER G, BRENNER S, ANGERMANN C E, et al. GOLD or lower limit of normal definition? A comparison with expert-based diagnosis of chronic obstructive pulmonary disease in a prospective cohort-study[J]. Respir Res,2012,13(1):13.
|
| [57] |
ROCHESTER C L, ALISON J A, CARLIN B, et al. Pulmonary rehabilitation for adults with chronic respiratory disease:an official American thoracic society clinical practice guideline[J]. Am J Respir Crit Care Med, 2023, 208(4):e7-26. DOI: 10.1164/rccm.202306-1066ST.
|
| [58] |
SCHRIJVER J, LENFERINK A, BRUSSE-KEIZER M, et al. Self-management interventions for people with chronic obstructive pulmonary disease[J]. Cochrane Database Syst Rev, 2022, 1(1):CD002990. DOI: 10.1002/14651858.CD002990.pub4.
|
| [59] |
OSHAGBEMI O A, FRANSSEN F M E, VAN KRAAIJ S, et al. Blood eosinophil counts,withdrawal of inhaled corticosteroids and risk of COPD exacerbations and mortality in the clinical practice research datalink(CPRD)[J]. COPD, 2019, 16(2):152-159. DOI: 10.1080/15412555.2019.1608172.
|
| [60] |
SUISSA S, DELL’ANIELLO S, ERNST P. Discontinuation of inhaled corticosteroids from triple therapy in COPD:effects on major outcomes in real world clinical practice[J]. COPD, 2022, 19(1):133-141. DOI: 10.1080/15412555.2022.2045265.
|
| [61] |
VOGELMEIER C F, WORTH H, BUHL R, et al. Impact of switching from triple therapy to dual bronchodilation in COPD:the DACCORD 'real world’ study[J]. Respir Res, 2022, 23(1):109. DOI: 10.1186/s12931-022-02037-2.
|
| [62] |
NECHES GARCÍA V, VALLEJO-APARICIO L A, ISMAILA A S, et al. Clinical and economic impact of long-term inhaled corticosteroid withdrawal in patients with chronic obstructive pulmonary disease treated with triple therapy in Spain[J]. Int J Chron Obstruct Pulmon Dis, 2022, 17:2161-2174. DOI: 10.2147/COPD.S367708.
|
| [63] |
ANZUETO A, BARJAKTAREVIC I Z, SILER T M, et al. Ensifentrine,a novel phosphodiesterase 3 and 4 inhibitor for the treatment of chronic obstructive pulmonary disease:randomized,double-blind,placebo-controlled,multicenter phase III trials(the ENHANCE trials)[J]. Am J Respir Crit Care Med, 2023, 208(4):406-416. DOI: 10.1164/rccm.202306-0944oc.
|
| [64] |
SINGH D, AGUSTI A, MARTINEZ F J, et al. Blood eosinophils and chronic obstructive pulmonary disease:a global initiative for chronic obstructive lung disease science committee 2022 review[J]. Am J Respir Crit Care Med, 2022, 206(1):17-24. DOI: 10.1164/rccm.202201-0209pp.
|
| [21] |
VAZ FRAGOSO C A, MCAVAY G, VAN NESS P H, et al. Phenotype of spirometric impairment in an aging population[J]. Am J Respir Crit Care Med, 2016, 193(7):727-735. DOI: 10.1164/rccm.201508-1603oc.
|
| [22] |
MALINOVSCHI A, ZHOU X, ANDERSSON A, et al. Consequences of using post- or prebronchodilator reference values in interpreting spirometry[J]. Am J Respir Crit Care Med, 2023, 208(4):461-471. DOI: 10.1164/rccm.202212-2341oc.
|
| [23] |
DUONG M, ISLAM S, RANGARAJAN S, et al. Global differences in lung function by region(PURE):an international,community-based prospective study[J]. Lancet Respir Med, 2013, 1(8):599-609. DOI: 10.1016/s2213-2600(13)70164-4.
|
| [24] |
DIAO J A, HE Y, KHAZANCHI R, et al. Implications of race adjustment in lung-function equations[J]. N Engl J Med, 2024, 390(22):2083-2097. DOI: 10.1056/nejmsa2311809.
|
| [25] |
BACKMAN H, BLOMBERG A, LUNDQUIST A, et al. Lung function trajectories and associated mortality among adults with and without airway obstruction[J]. Am J Respir Crit Care Med,2023,208(10):1063-1074.
|
| [26] |
SIN D D, ANTHONISEN N R, SORIANO J B, et al. Mortality in COPD:role of comorbidities[J]. Eur Respir J, 2006, 28(6):1245-1257. DOI: 10.1183/09031936.00133805.
|
| [27] |
AGUSTÍ A, EDWARDS L D, RENNARD S I, et al. Persistent systemic inflammation is associated with poor clinical outcomes in COPD:a novel phenotype[J]. PLoS One, 2012, 7(5):e37483. DOI: 10.1371/journal.pone.0037483.
|
| [28] |
HURST J R, GALE C P, Global Working Group on Cardiopulmonary Risk. MACE in COPD:addressing cardiopulmonary risk[J]. Lancet Respir Med, 2024, 12(5):345-348. DOI: 10.1016/s2213-2600(24)00038-9.
|
| [29] |
GRAUL E L, NORDON C, RHODES K, et al. Temporal risk of nonfatal cardiovascular events after chronic obstructive pulmonary disease exacerbation:a population-based study[J]. Am J Respir Crit Care Med, 2024, 209(8):960-972. DOI: 10.1164/rccm.202307-1122oc.
|
| [65] |
SINGH D, LEA S, MATHIOUDAKIS A G. Inhaled phosphodiesterase inhibitors for the treatment of chronic obstructive pulmonary disease[J]. Drugs, 2021, 81(16):1821-1830. DOI: 10.1007/s40265-021-01616-9.
|
| [66] |
BHATT S P, RABE K F, HANANIA N A, et al. Dupilumab for COPD with type 2 inflammation indicated by eosinophil counts[J]. N Engl J Med, 2023, 389(3):205-214. DOI: 10.1056/nejmoa2303951.
|
| [67] |
KOVACS G, AGUSTI A, BARBERÀ J A, et al. Pulmonary vascular involvement in chronic obstructive pulmonary disease. is there a pulmonary vascular phenotype?[J]. Am J Respir Crit Care Med, 2018, 198(8):1000-1011. DOI: 10.1164/rccm.201801-0095pp.
|
| [68] |
PEPKE-ZABA J, DELCROIX M, LANG I, et al. Chronic thromboembolic pulmonary hypertension(CTEPH):results from an international prospective registry[J]. Circulation, 2011, 124(18):1973-1981. DOI: 10.1161/CIRCULATIONAHA.110.015008.
|
| [69] |
KOVACS G, AVIAN A, BACHMAIER G, et al. Severe pulmonary hypertension in COPD impact on survival and diagnostic approach[J]. Chest, 2022, 162(1):202-212. DOI: 10.1016/j.chest.2022.01.031.
|
| [70] |
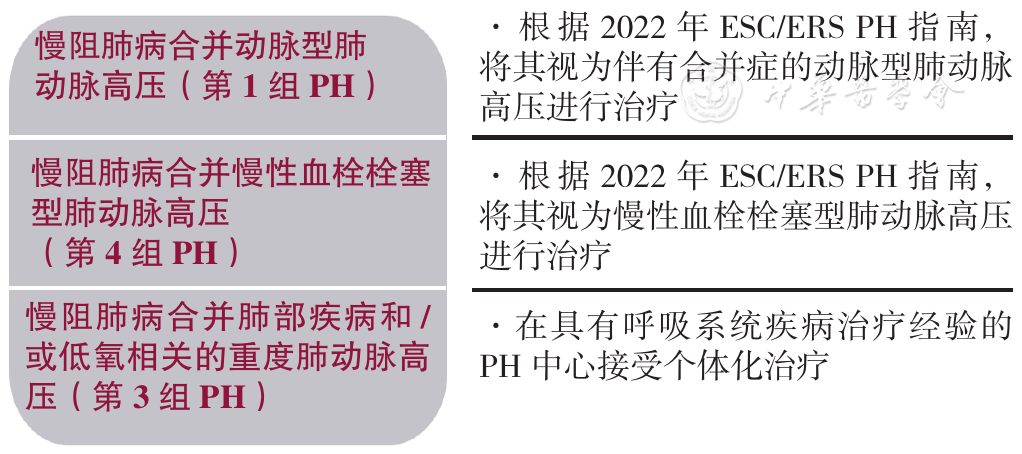
HUMBERT M, KOVACS G, HOEPER M M, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension[J]. Eur Heart J, 2022, 43(38):3618-3731. DOI: 10.1093/eurheartj/ehac237.
|
| [71] |
DAURIAT G, REYNAUD-GAUBERT M, COTTIN V, et al. Severe pulmonary hypertension associated with chronic obstructive pulmonary disease:a prospective French multicenter cohort[J]. J Heart Lung Transplant, 2021, 40(9):1009-1018. DOI: 10.1016/j.healun.2021.04.021.
|
| [72] |
DOCHERTY A B, HARRISON E M, GREEN C A, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol:prospective observational cohort study[J]. BMJ, 2020, 369:m1985. DOI: 10.1136/bmj.m1985.
|
| [73] |
TAL-SINGER R, CRAPO J D. COPD at the time of COVID-19:a COPD foundation perspective[J]. Chronic Obstr Pulm Dis, 2020, 7(2):73-75. DOI: 10.15326/jcopdf.7.2.2020.0149.
|
| [74] |
CHEN X, ZHOU C W, FU Y Y, et al. Global,regional,and national burden of chronic respiratory diseases and associated risk factors,1990-2019:Results from the Global Burden of Disease Study 2019[J]. Front Med, 2023, 10:1066804. DOI: 10.3389/fmed.2023.1066804.
|
| [75] |
YU Y, XIAO W, DU L Y, et al. Acupuncture for dyspnea and breathing physiology in chronic respiratory diseases:a systematic review and meta-analysis of randomized controlled trials[J]. Heliyon, 2024, 10(10):e31176. DOI: 10.1016/j.heliyon.2024.e31176.
|
| [76] |
ZHOU L, YANG H, ZHANG Y, et al. Predictive value of lung function measures for cardiovascular risk:a large prospective cohort study[J]. Thorax, 2024, 79(3):250-258. DOI: 10.1136/thorax-2023-220703.
|
| [77] |
BAI J J, CUI J X, YU C H. Burden of chronic obstructive pulmonary disease attributable to non-optimal temperature from 1990 to 2019:a systematic analysis from the Global Burden of Disease Study 2019[J]. Environ Sci Pollut Res, 2023, 30(26):68836-68847. DOI: 10.1007/s11356-023-27325-2.
|
| [78] |
FANG Y C, CHENG W H, LU H I, et al. Double lung transplantation is better than single lung transplantation for end-stage chronic obstructive pulmonary disease:a meta-analysis[J]. J Cardiothorac Surg, 2024, 19(1):162. DOI: 10.1186/s13019-024-02654-6.
|
 )
)
 )
)