中国全科医学 ›› 2023, Vol. 26 ›› Issue (30): 3772-3779.DOI: 10.12114/j.issn.1007-9572.2023.0202
闫可1, 魏菀怡2, 李曙光1, 么伟楠1, 董静1, 王晓斌1, 张雪原1, 杨洁1, 沈文斌1, 祝淑钗1,*( )
)
收稿日期:2023-03-08
修回日期:2023-05-23
出版日期:2023-10-20
发布日期:2023-05-31
通讯作者:
祝淑钗
基金资助:
YAN Ke1, WEI Wanyi2, LI Shuguang1, YAO Weinan1, DONG Jing1, WANG Xiaobin1, ZHANG Xueyuan1, YANG Jie1, SHEN Wenbin1, ZHU Shuchai1,*( )
)
Received:2023-03-08
Revised:2023-05-23
Published:2023-10-20
Online:2023-05-31
Contact:
ZHU Shuchai
摘要: 背景 根治性同步放化疗后行巩固化疗能否改善局部晚期食管癌患者预后存在较大争议。临床中缺乏能够稳定、准确判断食管癌患者生存的营养风险筛查工具。 目的 探讨巩固化疗对接受根治性同步放化疗的局部晚期食管鳞状细胞癌患者预后的影响。 方法 选取2013年1月—2018年12月于河北医科大学第四医院放疗科行根治性同步放化疗的食管鳞状细胞癌患者223例为研究对象,依据患者采用的放化疗方案,将患者分为单纯同步放化疗组(87例)和联合巩固化疗组(136例)。通过电子病历系统收集患者一般资料、美国东部肿瘤协作组(ECOG)评分、肿瘤部位、肿瘤长度、TNM分期、放疗剂量、照射方式、化疗方案等。应用营养风险筛查2002(NRS 2002)对患者放化疗前营养状况进行评分。患者同步放化疗结束1个月内进行疗效评价,包括完全缓解(CR)、部分缓解(PR)、疾病稳定(SD)及疾病进展(PD)。患者通过电话(本院随访中心完成)及门诊复查进行随访,收集患者的总生存期(OS)、无局部区域复发生存期(LRRFS)及无远转生存期(DMFS)情况,随访截至2022-09-30。采用Kaplan-Meier法绘制患者OS、LRRFS、DMFS的生存曲线,生存曲线的比较采用Log-rank检验。采用单因素及多因素Cox比例风险回归分析探讨患者预后的影响因素。 结果 单纯同步放化疗组和联合巩固化疗组患者基线资料比较,差异无统计学意义(P>0.05)。两组总生存率、无局部区域复发生存率、无远转生存率比较,差异均无统计学意义(χ2=1.942、0.743、1.272,P=0.163、0.389、0.259)。治疗前NRS 2002评分<3分患者172例,NRS 2002评分≥3分患者51例,两组总生存率、无局部区域复发生存率、无远转生存率比较,差异有统计学意义(χ2=6.585、4.858、7.814,P=0.010、0.028、0.005)。多因素Cox比例风险回归分析结果显示,TNM分期、NRS 2002评分为患者OS、DMFS的影响因素(P<0.05),照射方式为患者LRRFS、DMFS的影响因素(P<0.05),临床疗效为患者OS、LRRFS、DMFS的影响因素(P<0.05)。分层分析结果显示,在TNM分期Ⅱ期及临床疗效CR的患者中,联合巩固化疗组(74例、33例)总生存率高于单纯同步放化疗组(43例、28例)(χ2=4.811、3.932,P=0.028、0.047)。 结论 巩固化疗并未改善临床Ⅱ~Ⅲ期食管鳞状细胞癌患者根治性同步放化疗后的预后生存,但对于临床分期偏早、病变缓解良好、营养状况良好的患者,巩固化疗可能带来一定的生存获益。NRS 2002作为营养风险筛查工具对局部晚期食管癌患者放化疗后的长期生存有显著的预测价值。
| 组别 | 例数 | 性别(男/女) | 年龄〔例(%)〕 | ECOG评分〔例(%)〕 | 肿瘤部位〔例(%)〕 | 肿瘤长度〔例(%)〕 | T分期〔例(%)〕 | N分期〔例(%)〕 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <64岁 | ≥64岁 | 0分 | 1~2分 | 颈胸上段 | 胸中下段 | <6 cm | ≥6 cm | T1/T2期 | T3/T4期 | N0期 | N1/N2期 | |||
| 单纯同步放化疗组 | 87 | 60/27 | 39(44.8) | 48(55.2) | 29(33.3) | 58(66.7) | 28(32.2) | 59(67.8) | 43(49.4) | 44(50.6) | 26(29.9) | 61(80.1) | 16(18.4) | 71(81.6) |
| 联合巩固化疗组 | 136 | 96/40 | 68(50.0) | 68(50.0) | 53(39.0) | 83(61.0) | 54(39.7) | 82(60.3) | 72(52.9) | 64(47.1) | 41(30.1) | 95(69.9) | 28(20.6) | 108(79.4) |
| χ2值 | 0.066 | 0.569 | 0.725 | 1.044 | 0.263 | 0.002 | 0.162 | |||||||
| P值 | 0.797 | 0.451 | 0.394 | 0.307 | 0.608 | 0.967 | 0.688 | |||||||
| 组别 | TNM分期〔例(%)〕 | 放疗剂量〔例(%)〕 | 照射方式〔例(%)〕 | 化疗方案〔例(%)〕 | NRS 2002评分〔例(%)〕 | 临床疗效〔例(%)〕 | ||||||||
| Ⅱ期 | Ⅲ期 | <60.8 Gy | ≥60.8 Gy | ENI | IFI | TP | FP | <3分 | ≥3分 | CR | PR+SD | |||
| 单纯同步放化疗组 | 43(49.4) | 44(50.6) | 48(55.2) | 39(44.8) | 40(46.0) | 47(54.0) | 61(70.1) | 26(29.9) | 65(74.7) | 22(25.3) | 28(32.2) | 59(67.8) | ||
| 联合巩固化疗组 | 74(54.4) | 62(45.6) | 63(46.3) | 73(53.7) | 72(52.9) | 64(47.1) | 91(66.9) | 45(33.1) | 107(78.7) | 29(21.3) | 33(24.3) | 103(75.7) | ||
| χ2值 | 0.529 | 1.662 | 1.029 | 0.251 | 0.473 | 1.674 | ||||||||
| P值 | 0.467 | 0.197 | 0.310 | 0.616 | 0.492 | 0.196 | ||||||||
表1 两组患者临床资料比较
Table 1 Comparison of clinical data between the two groups of patients
| 组别 | 例数 | 性别(男/女) | 年龄〔例(%)〕 | ECOG评分〔例(%)〕 | 肿瘤部位〔例(%)〕 | 肿瘤长度〔例(%)〕 | T分期〔例(%)〕 | N分期〔例(%)〕 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <64岁 | ≥64岁 | 0分 | 1~2分 | 颈胸上段 | 胸中下段 | <6 cm | ≥6 cm | T1/T2期 | T3/T4期 | N0期 | N1/N2期 | |||
| 单纯同步放化疗组 | 87 | 60/27 | 39(44.8) | 48(55.2) | 29(33.3) | 58(66.7) | 28(32.2) | 59(67.8) | 43(49.4) | 44(50.6) | 26(29.9) | 61(80.1) | 16(18.4) | 71(81.6) |
| 联合巩固化疗组 | 136 | 96/40 | 68(50.0) | 68(50.0) | 53(39.0) | 83(61.0) | 54(39.7) | 82(60.3) | 72(52.9) | 64(47.1) | 41(30.1) | 95(69.9) | 28(20.6) | 108(79.4) |
| χ2值 | 0.066 | 0.569 | 0.725 | 1.044 | 0.263 | 0.002 | 0.162 | |||||||
| P值 | 0.797 | 0.451 | 0.394 | 0.307 | 0.608 | 0.967 | 0.688 | |||||||
| 组别 | TNM分期〔例(%)〕 | 放疗剂量〔例(%)〕 | 照射方式〔例(%)〕 | 化疗方案〔例(%)〕 | NRS 2002评分〔例(%)〕 | 临床疗效〔例(%)〕 | ||||||||
| Ⅱ期 | Ⅲ期 | <60.8 Gy | ≥60.8 Gy | ENI | IFI | TP | FP | <3分 | ≥3分 | CR | PR+SD | |||
| 单纯同步放化疗组 | 43(49.4) | 44(50.6) | 48(55.2) | 39(44.8) | 40(46.0) | 47(54.0) | 61(70.1) | 26(29.9) | 65(74.7) | 22(25.3) | 28(32.2) | 59(67.8) | ||
| 联合巩固化疗组 | 74(54.4) | 62(45.6) | 63(46.3) | 73(53.7) | 72(52.9) | 64(47.1) | 91(66.9) | 45(33.1) | 107(78.7) | 29(21.3) | 33(24.3) | 103(75.7) | ||
| χ2值 | 0.529 | 1.662 | 1.029 | 0.251 | 0.473 | 1.674 | ||||||||
| P值 | 0.467 | 0.197 | 0.310 | 0.616 | 0.492 | 0.196 | ||||||||
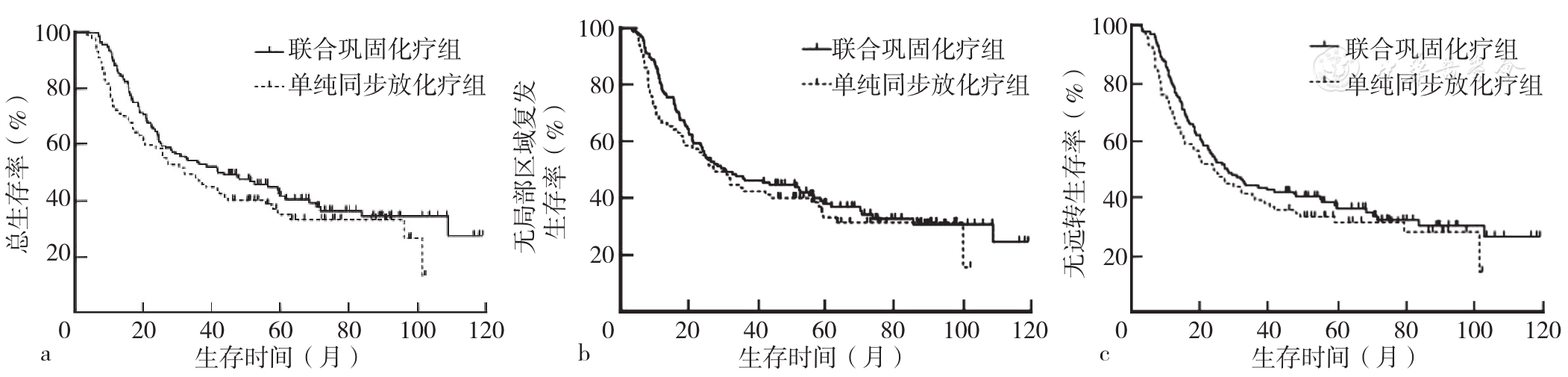
图1 联合巩固化疗组与单纯同步放化疗组患者OS、LRRFS、DMFS的Kaplan-Meier生存曲线注:a为两组患者OS生存曲线,b为两组患者LRRFS生存曲线,c为两组患者DMFS生存曲线。
Figure 1 Kaplan-Meier survival curves of OS,LRRFS and DMFS in combined consolidation chemotherapy group and simple CCRT group
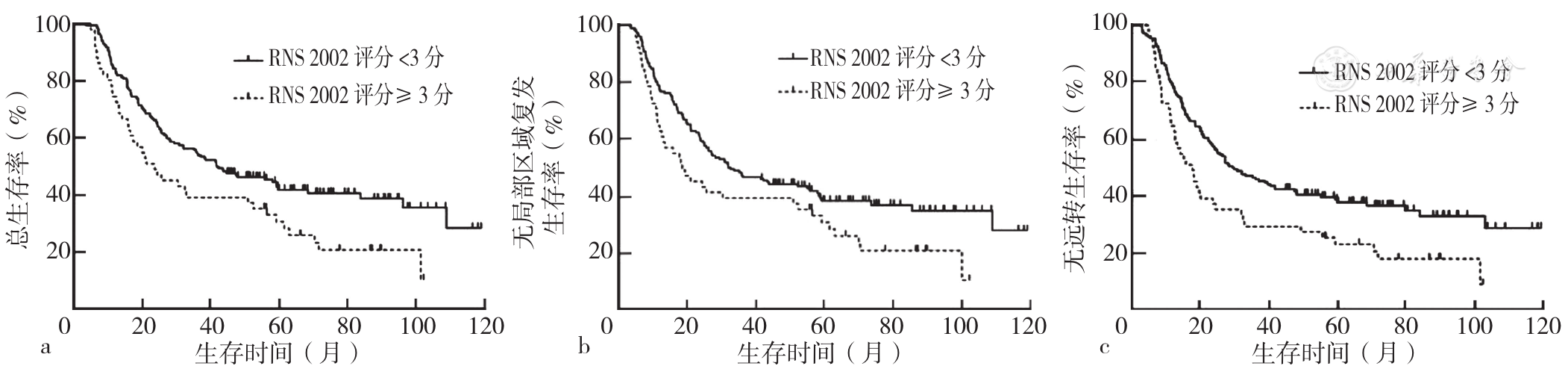
图2 NRS 2002评分<3分与NRS 2002评分≥3分患者OS、LRRFS、DMFS的Kaplan-Meier生存曲线注:NRS 2002=营养风险筛查2002;a为两组患者OS生存曲线,b为两组患者LRRFS生存曲线,c为两组患者DMFS生存曲线。
Figure 2 Kaplan-Meier survival curves of OS,LRRFS and DMFS in patients with NRS 2002 score<3 and NRS 2002 score≥3
| 变量 | 赋值 |
|---|---|
| 性别 | 男=0,女=1 |
| 年龄 | <64岁=0,≥64岁=1 |
| ECOG评分 | 0分=0,1~2分=1 |
| 肿瘤部位 | 颈胸上段=0,胸中下段=1 |
| 肿瘤长度 | <6 cm=0,≥6 cm=1 |
| T分期 | T1/T2期=0,T3/T4期=1 |
| N分期 | N0期=0,N1/N2期=1 |
| TNM分期 | Ⅱ期=0,Ⅲ期=1 |
| 放疗剂量 | <60.8 Gy=0,≥60.8 Gy=1 |
| 照射方式 | ENI=0,IFI=1 |
| 化疗方案 | TP=0,FP=1 |
| NRS 2002评分 | <3分=0,≥3分=1 |
| 临床疗效 | CR=0,PR+SD=1 |
| 治疗方式 | 单纯同步放化疗=0,联合巩固化疗=1 |
表2 临床Ⅱ~Ⅲ期食管鳞状细胞癌患者预后影响因素单因素和多因素Cox风险回归分析变量赋值
Table 2 Variable assignments for univariate and multivariate Cox hazard regression analysis of influencing factors for prognosis in patients with stage Ⅱ-Ⅲ ESCC
| 变量 | 赋值 |
|---|---|
| 性别 | 男=0,女=1 |
| 年龄 | <64岁=0,≥64岁=1 |
| ECOG评分 | 0分=0,1~2分=1 |
| 肿瘤部位 | 颈胸上段=0,胸中下段=1 |
| 肿瘤长度 | <6 cm=0,≥6 cm=1 |
| T分期 | T1/T2期=0,T3/T4期=1 |
| N分期 | N0期=0,N1/N2期=1 |
| TNM分期 | Ⅱ期=0,Ⅲ期=1 |
| 放疗剂量 | <60.8 Gy=0,≥60.8 Gy=1 |
| 照射方式 | ENI=0,IFI=1 |
| 化疗方案 | TP=0,FP=1 |
| NRS 2002评分 | <3分=0,≥3分=1 |
| 临床疗效 | CR=0,PR+SD=1 |
| 治疗方式 | 单纯同步放化疗=0,联合巩固化疗=1 |
| 项目 | OS | LRRFS | DMFS | |||
|---|---|---|---|---|---|---|
| HR(95%CI) | P值 | HR(95%CI) | P值 | HR(95%CI) | P值 | |
| 性别 | 0.712(0.491,1.034) | 0.074 | 0.694(0.481,1.002) | 0.050 | 0.719(0.502,1.030) | 0.072 |
| 年龄 | 0.771(0.553,1.074) | 0.123 | 0.733(0.529,1.015) | 0.061 | 0.798(0.579,1.098) | 0.166 |
| ECOG评分 | 1.224(0.879,1.703) | 0.231 | 1.266(0.915,1.752) | 0.155 | 1.316(0.957,1.811) | 0.092 |
| 肿瘤部位 | 2.004(1.387,2.896) | <0.001 | 1.839(1.288,2.624) | 0.001 | 1.953(1.372,2.780) | <0.001 |
| 肿瘤长度 | 1.637(1.173,2.286) | 0.004 | 1.593(1.148,2.211) | 0.005 | 1.586(1.150,2.187) | 0.005 |
| T分期 | 1.862(1.263,2.745) | 0.002 | 1.728(1.187,2.514) | 0.004 | 1.893(1.299,2.758) | 0.001 |
| N分期 | 1.873(1.176,2.984) | 0.008 | 1.642(1.058,2.547) | 0.027 | 1.943(1.244,3.035) | 0.004 |
| TNM分期 | 2.069(1.480,2.892) | <0.001 | 1.941(1.398,2.696) | <0.001 | 2.194(1.587,3.033) | <0.001 |
| 放疗剂量 | 0.866(0.622,1.206) | 0.395 | 0.876(0.632,1.213) | 0.425 | 0.846(0.615,1.165) | 0.307 |
| 照射方式 | 1.779(1.272,2.488) | 0.001 | 1.782(1.281,2.479) | 0.001 | 2.024(1.462,2.802) | <0.001 |
| 化疗方案 | 1.225(0.864,1.739) | 0.255 | 1.150(0.813,1.626) | 0.429 | 1.199(0.853,1.686) | 0.296 |
| NRS 2002评分 | 1.609(1.115,2.323) | 0.011 | 1.502(1.043,2.164) | 0.029 | 1.655(1.158,2.365) | 0.006 |
| 临床疗效 | 1.959(1.300,2.954) | 0.001 | 1.883(1.264,2.804) | 0.002 | 1.955(1.320,2.893) | 0.001 |
| 治疗方式 | 0.788(0.563,1.103) | 0.165 | 0.864(0.620,1.205) | 0.390 | 0.829(0.599,1.149) | 0.261 |
表3 临床Ⅱ~Ⅲ期食管鳞状细胞癌患者预后影响因素单因素Cox风险回归分析
Table 3 Univariate Cox hazard regression analysis of influencing factors for prognosis in patients with stage Ⅱ-Ⅲ ESCC
| 项目 | OS | LRRFS | DMFS | |||
|---|---|---|---|---|---|---|
| HR(95%CI) | P值 | HR(95%CI) | P值 | HR(95%CI) | P值 | |
| 性别 | 0.712(0.491,1.034) | 0.074 | 0.694(0.481,1.002) | 0.050 | 0.719(0.502,1.030) | 0.072 |
| 年龄 | 0.771(0.553,1.074) | 0.123 | 0.733(0.529,1.015) | 0.061 | 0.798(0.579,1.098) | 0.166 |
| ECOG评分 | 1.224(0.879,1.703) | 0.231 | 1.266(0.915,1.752) | 0.155 | 1.316(0.957,1.811) | 0.092 |
| 肿瘤部位 | 2.004(1.387,2.896) | <0.001 | 1.839(1.288,2.624) | 0.001 | 1.953(1.372,2.780) | <0.001 |
| 肿瘤长度 | 1.637(1.173,2.286) | 0.004 | 1.593(1.148,2.211) | 0.005 | 1.586(1.150,2.187) | 0.005 |
| T分期 | 1.862(1.263,2.745) | 0.002 | 1.728(1.187,2.514) | 0.004 | 1.893(1.299,2.758) | 0.001 |
| N分期 | 1.873(1.176,2.984) | 0.008 | 1.642(1.058,2.547) | 0.027 | 1.943(1.244,3.035) | 0.004 |
| TNM分期 | 2.069(1.480,2.892) | <0.001 | 1.941(1.398,2.696) | <0.001 | 2.194(1.587,3.033) | <0.001 |
| 放疗剂量 | 0.866(0.622,1.206) | 0.395 | 0.876(0.632,1.213) | 0.425 | 0.846(0.615,1.165) | 0.307 |
| 照射方式 | 1.779(1.272,2.488) | 0.001 | 1.782(1.281,2.479) | 0.001 | 2.024(1.462,2.802) | <0.001 |
| 化疗方案 | 1.225(0.864,1.739) | 0.255 | 1.150(0.813,1.626) | 0.429 | 1.199(0.853,1.686) | 0.296 |
| NRS 2002评分 | 1.609(1.115,2.323) | 0.011 | 1.502(1.043,2.164) | 0.029 | 1.655(1.158,2.365) | 0.006 |
| 临床疗效 | 1.959(1.300,2.954) | 0.001 | 1.883(1.264,2.804) | 0.002 | 1.955(1.320,2.893) | 0.001 |
| 治疗方式 | 0.788(0.563,1.103) | 0.165 | 0.864(0.620,1.205) | 0.390 | 0.829(0.599,1.149) | 0.261 |
| 项目 | OS | LRRFS | DMFS | |||
|---|---|---|---|---|---|---|
| HR(95%CI) | P值 | HR(95%CI) | P值 | HR(95%CI) | P值 | |
| 肿瘤部位 | 1.402(0.936,2.099) | 0.101 | 1.228(0.825,1.829) | 0.311 | 1.241(0.838,1.839) | 0.281 |
| 肿瘤长度 | 0.962(0.618,1.498) | 0.864 | 1.040(0.672,1.610) | 0.861 | 0.885(0.581,1.347) | 0.568 |
| T分期 | 1.264(0.768,2.080) | 0.356 | 1.111(0.677,1.823) | 0.677 | 1.280(0.790,2.072) | 0.316 |
| N分期 | 1.399(0.871,2.246) | 0.165 | 1.224(0.780,1.921) | 0.379 | 1.471(0.933,2.318) | 0.096 |
| TNM分期 | 1.480(1.008,2.174) | 0.046 | 1.439(0.985,2.103) | 0.060 | 1.606(1.113,2.317) | 0.011 |
| 照射方式 | 1.350(0.938,1.944) | 0.106 | 1.478(1.024,2.134) | 0.037 | 1.640(1.148,2.342) | 0.007 |
| NRS 2002评分 | 1.497(1.029,2.177) | 0.035 | 1.363(0.937,1.982) | 0.105 | 1.565(1.084,2.259) | 0.017 |
| 临床疗效 | 1.890(1.252,2.853) | 0.002 | 1.842(1.236,2.746) | 0.003 | 1.986(1.337,2.951) | 0.001 |
表4 临床Ⅱ~Ⅲ期食管鳞状细胞癌患者预后影响因素多因素Cox风险回归分析
Table 4 Multivariate Cox hazard regression analysis of influencing factors of prognosis in patients with stage Ⅱ-Ⅲ ESCC
| 项目 | OS | LRRFS | DMFS | |||
|---|---|---|---|---|---|---|
| HR(95%CI) | P值 | HR(95%CI) | P值 | HR(95%CI) | P值 | |
| 肿瘤部位 | 1.402(0.936,2.099) | 0.101 | 1.228(0.825,1.829) | 0.311 | 1.241(0.838,1.839) | 0.281 |
| 肿瘤长度 | 0.962(0.618,1.498) | 0.864 | 1.040(0.672,1.610) | 0.861 | 0.885(0.581,1.347) | 0.568 |
| T分期 | 1.264(0.768,2.080) | 0.356 | 1.111(0.677,1.823) | 0.677 | 1.280(0.790,2.072) | 0.316 |
| N分期 | 1.399(0.871,2.246) | 0.165 | 1.224(0.780,1.921) | 0.379 | 1.471(0.933,2.318) | 0.096 |
| TNM分期 | 1.480(1.008,2.174) | 0.046 | 1.439(0.985,2.103) | 0.060 | 1.606(1.113,2.317) | 0.011 |
| 照射方式 | 1.350(0.938,1.944) | 0.106 | 1.478(1.024,2.134) | 0.037 | 1.640(1.148,2.342) | 0.007 |
| NRS 2002评分 | 1.497(1.029,2.177) | 0.035 | 1.363(0.937,1.982) | 0.105 | 1.565(1.084,2.259) | 0.017 |
| 临床疗效 | 1.890(1.252,2.853) | 0.002 | 1.842(1.236,2.746) | 0.003 | 1.986(1.337,2.951) | 0.001 |
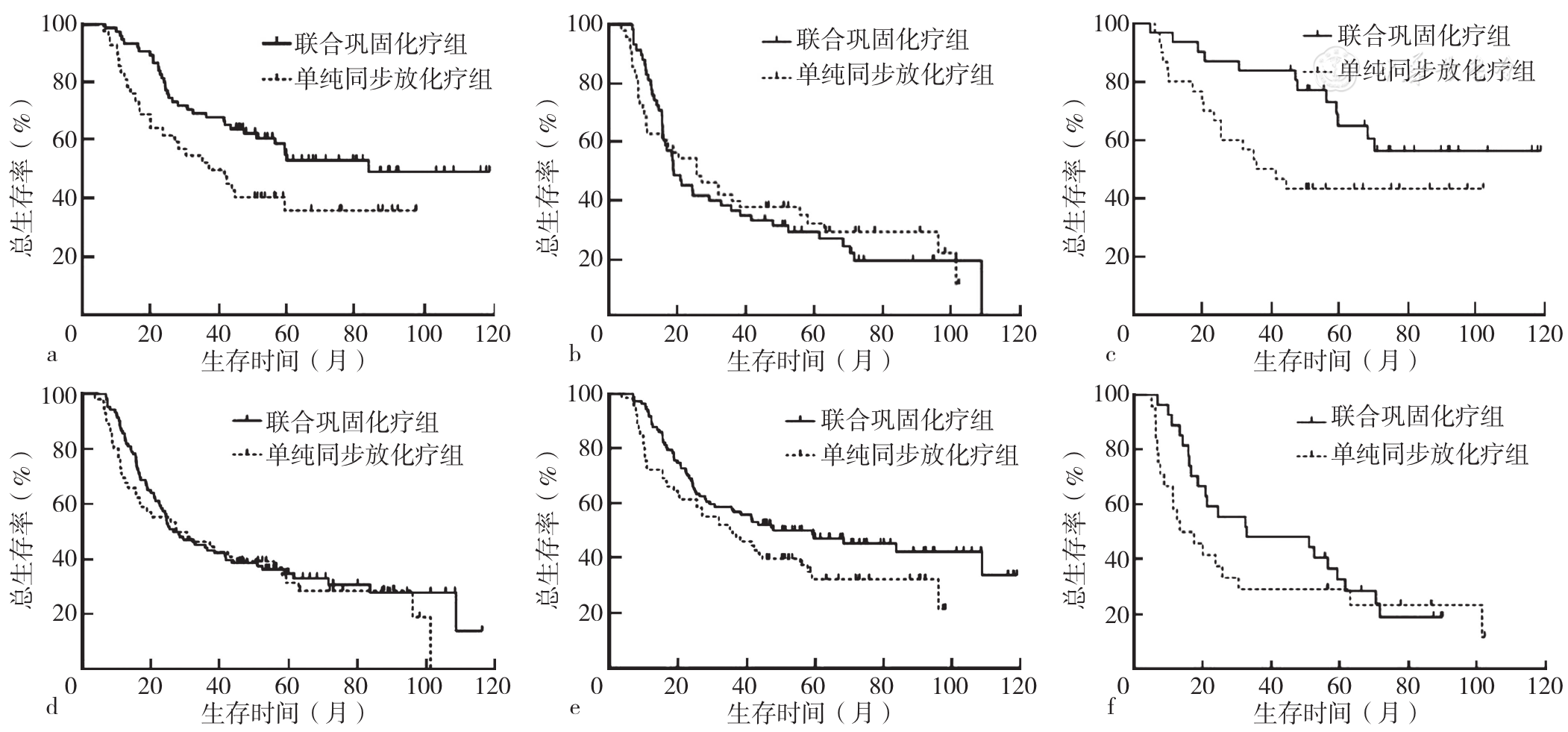
图3 不同分层的联合巩固化疗组与单纯同步放化疗组患者OS的Kaplan-Meier生存曲线注:a为TNM分期Ⅱ期,b为TNM分期临床Ⅲ期,c为临床疗效CR,d为临床疗效为PR+SD,e为NRS 2002评分<3分,f为NRS 2002评分≥3分。
Figure 3 Kaplan-Meier survival curves for OS in different stratified combined consolidation chemotherapy group and simple CCRT group
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
中国非手术治疗食管癌临床分期专家小组. 非手术治疗食管癌的临床分期标准草案[J]. 中华放射肿瘤学杂志,2010,19(3):179-180. DOI:10.3760/cma.j.issn.1004-4221.2010.03.001.
|
| [12] |
中国医师协会放射肿瘤治疗医师分会,中华医学会放射肿瘤治疗学分会,中国抗癌协会肿瘤放射治疗专业委员会. 中国食管癌放射治疗指南(2022年版)[J]. 国际肿瘤学杂志,2022,49(11):12-25. DOI:10.3760/cma.j.cn371439-20221011-00129.
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [21] |
|
| [22] |
|
| [23] |
|
| [24] |
|
| [25] |
|
| [26] |
|
| [27] |
|
| [28] |
|
| [29] |
|
| [30] |
|
| [31] |
|
| [32] |
|
| [33] |
|
| [1] | 薛崇祥, 鲁星妤, 刘哲宁, 董慧静, 郑玉敏, 崔慧娟. 动态监测肺癌患者基因变化规律及其预后意义[J]. 中国全科医学, 2023, 26(36): 4527-4534. |
| [2] | 白海威, 米小昆, 刘青蕊, 祝琳, 王英南, 刘俊艳, 韩颖. 血清尿酸对非小细胞肺癌患者围术期急性缺血性卒中的预测价值研究[J]. 中国全科医学, 2023, 26(36): 4545-4551. |
| [3] | 刘爱玲, 周静静, 李成程, 贺凯玥, 梁珊珊, 周尚成. 1990—2019年中国归因于烟草的食管癌疾病负担趋势和死亡预测分析[J]. 中国全科医学, 2023, 26(36): 4587-4594. |
| [4] | 崔晓娜, 冯瑞霞, 韩雨澎, 周瑶瑶, 刘小军, 李建朝. 静脉-动脉体外膜肺氧合和主动脉内球囊反搏联合辅助顺序对急性心肌梗死合并心源性休克患者的临床效果比较研究[J]. 中国全科医学, 2023, 26(35): 4439-4445. |
| [5] | 楚晓婧, 李俊, 付艳芹, 刘丹青, 刘爱萍, 张园园. 人体体质成分及血清生化指标对瞬感扫描式动态血糖监测仪准确性的影响研究[J]. 中国全科医学, 2023, 26(35): 4433-4438. |
| [6] | 谢雪梅, 高静, 柏丁兮, 卢贤英, 何佳丽, 李月. 老年人多重用药依从性现状及影响因素的Meta分析[J]. 中国全科医学, 2023, 26(35): 4394-4403. |
| [7] | 王越, 陈晴, 刘鲁蓉. 中国老年人抑郁检出率及影响因素的Meta分析[J]. 中国全科医学, 2023, 26(34): 4329-4335. |
| [8] | 李殿江, 潘恩春, 孙中明, 文进博, 王苗苗, 武鸣, 沈冲. 社区2型糖尿病患者临床惰性现状及其影响因素分析[J]. 中国全科医学, 2023, 26(34): 4296-4301. |
| [9] | 郝爱华, 曾韦霖, 李观海, 夏英华, 陈亮. 基于全科医生视角的家庭医生团队签约现状调查研究[J]. 中国全科医学, 2023, 26(34): 4261-4268. |
| [10] | 秦凤银, 张绮珊, 赖锦佳, 黄奕敏, 韩郭茵, 孙兴兰, 王芬, 谭益冰. 广东省社区居民脑卒中高危筛查意向的现状及影响因素研究[J]. 中国全科医学, 2023, 26(34): 4283-4289. |
| [11] | 王丽娜, 高鹏飞, 曹帆, 葛莹, 颜维, 何岱昆. 不同性别人群非酒精性脂肪性肝病患病现况及影响因素分析[J]. 中国全科医学, 2023, 26(33): 4143-4151. |
| [12] | 彰金, 丁治国, 祁烁, 李颖, 李伟强, 张媛媛, 周通. 血清甲状腺激素水平与心力衰竭患者住院期间预后的相关性研究[J]. 中国全科医学, 2023, 26(33): 4125-4129. |
| [13] | 周俞余, 高川, 崔埔安, 王亚平, 何仲. 更年期综合征患者绝经激素治疗中医患共同决策质量的影响因素研究[J]. 中国全科医学, 2023, 26(33): 4181-4186. |
| [14] | 张思宇, 周郁秋, 杜晓慧, 王正君. 精神病未治期及其早期干预的研究进展[J]. 中国全科医学, 2023, 26(33): 4110-4117. |
| [15] | 梁譞, 那飞扬, 秦梦瑶, 杨辉, 郭丽, 郭琪, 任蕾, 陈德, 刘东海, 张蓉芳. 儿童支气管哮喘合并阻塞性睡眠呼吸暂停低通气综合征的临床特征及影响因素研究[J]. 中国全科医学, 2023, 26(33): 4225-4230. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





