中国全科医学 ›› 2025, Vol. 28 ›› Issue (26): 3229-3239.DOI: 10.12114/j.issn.1007-9572.2024.0652
所属专题: 心血管最新文章合辑
向心月1, 张冰青1, 欧阳煜钦1, 汤文娟2, 冯文焕1,*( )
)
收稿日期:2024-09-10
修回日期:2025-02-20
出版日期:2025-09-15
发布日期:2025-07-22
通讯作者:
冯文焕
作者贡献:
向心月负责临床数据收集、整理、分析,并撰写论文初稿;张冰青负责绘制图表并协助统计分析;欧阳煜钦负责临床资料质量把控,协助初稿撰写;汤文娟完善论文的审校;冯文焕提出研究思路,设计研究方案,完善论文最终内容及审校,并对论文负责。
基金资助:
XIANG Xinyue1, ZHANG Bingqing1, OUYANG Yuqin1, TANG Wenjuan2, FENG Wenhuan1,*( )
)
Received:2024-09-10
Revised:2025-02-20
Published:2025-09-15
Online:2025-07-22
Contact:
FENG Wenhuan
摘要: 背景 肥胖患者存在更多动脉粥样硬化性心血管疾病(ASCVD)风险,肥胖多学科门诊短期内科门诊减重对肥胖患者ASCVD风险等级的影响有待明确。 目的 探讨短期内科门诊减重对肥胖患者ASCVD风险等级的影响。 方法 回顾性选取2019年7月—2024年5月在南京鼓楼医院内分泌科肥胖多学科就诊并完成3个月随访的172例肥胖患者为研究对象。记录患者一般资料、临床指标及ASCVD风险(应用中国成年人ASCVD总体风险评估流程图进行ASCVD风险评估)。基于患者治疗前ASCVD风险评级分为中高危组(n=58)和低危组(n=114),比较两组一般资料的差异。中高危组患者根据治疗3个月后ASCVD风险下降情况分为中高危降低亚组(n=36)和中高危不变亚组(n=22),比较两亚组治疗前后各指标差异及ASCVD风险,采用多因素Logistic回归分析探究中高危ASCVD风险肥胖患者风险下降的影响因素。分析不同用药组及以BMI、性别、年龄分层的患者治疗3个月后ASCVD风险等级及减重指标的差异。 结果 172例患者中男73例、女99例,平均年龄32(28,38)岁,平均体质量89.8(82.0,101.2)kg,平均BMI 31.6(30.0,33.9)kg/m2。治疗3个月后患者总体质量减少量为8.8%(5.6%,13.6%),BMI下降为28.8(27.0,30.7)kg/m2,腰围、腰高比、体脂肪、体脂百分比、脂肪质量指数(FMI)、四肢骨骼肌指数、总肌肉量、内脏脂肪面积(VFA)、收缩压、舒张压及糖脂代谢指标(空腹血糖、餐后2 h血糖、空腹胰岛素、餐后2 h胰岛素、胰岛素抵抗指数、三酰甘油、总胆固醇、低密度脂蛋白胆固醇、尿酸、丙氨酸氨基转移酶及天冬氨酸氨基转移酶)均较治疗前下降(P<0.05)。治疗前114例患者为ASCVD低危组,58例患者为ASCVD中高危组。与中高危组相比,低危组治疗前空腹血糖、餐后2 h血糖、餐后2 h胰岛素、胰岛素抵抗指数、三酰甘油、总胆固醇、低密度脂蛋白胆固醇、丙氨酸氨基转移酶及天冬氨酸氨基转移酶降低,高密度脂蛋白胆固醇升高(P<0.05)。58例治疗前中高危ASCVD风险患者治疗3个月后36例降为低风险(中高危降低亚组),22例患者仍为中高危(中高危不变亚组),治疗3个月后两亚组体质量、BMI、腰围、腰高比、体脂肪、体脂百分比、FMI、VFA、空腹胰岛素、餐后2 h胰岛素、胰岛素抵抗指数、三酰甘油、丙氨酸氨基转移酶及天冬氨酸氨基转移酶均较治疗前下降,中高危降低亚组收缩压、舒张压、空腹血糖、总胆固醇及低密度脂蛋白胆固醇较治疗前下降(P<0.05);中高危降低亚组BMI、体脂肪、体脂百分比、FMI及VFA较中高危不变亚组下降(P<0.05)。多因素Logistic回归分析显示BMI(OR=1.257,95%CI=1.034~1.528,P=0.022)是中高危ASCVD风险肥胖患者危险因素下降的独立危险因素,BMI每下降1个单位,ASCVD风险降低25.7%。利拉鲁肽组(n=51)、二甲双胍组(n=61)及未用药组(n=60)治疗3个月后ASCVD中高危患者占比均较治疗前下降(P<0.05),治疗3个月后三组间ASCVD风险等级及减重指标比较,差异无统计学意义(P>0.05)。治疗3个月后28.0 kg/m2≤BMI<32.5 kg/m2组和BMI≥32.5 kg/m2组ASCVD中高风险患者占比均较治疗前下降,28.0 kg/m2≤BMI<32.5 kg/m2组ASCVD中高风险患者占比低于BMI≥32.5 kg/m2组(P<0.05);治疗3个月后女性组和男性组ASCVD中高风险患者占比均下降(P<0.05),治疗3个月后两组ASCVD风险等级比较,差异无统计学意义(P>0.05)。治疗3个月后18~30岁组和≥30岁组ASCVD风险等级比较,差异无统计学意义(P>0.05)。 结论 肥胖患者经短期内科门诊减重,可有效减重、减脂,改善ASCVD危险因素,对于BMI≥32.5 kg/m2伴中高危ASCVD风险者,这种减重措施尚不足以短期内降低ASCVD风险等级,更强及持久减重措施是未来治疗的选择。
中图分类号:
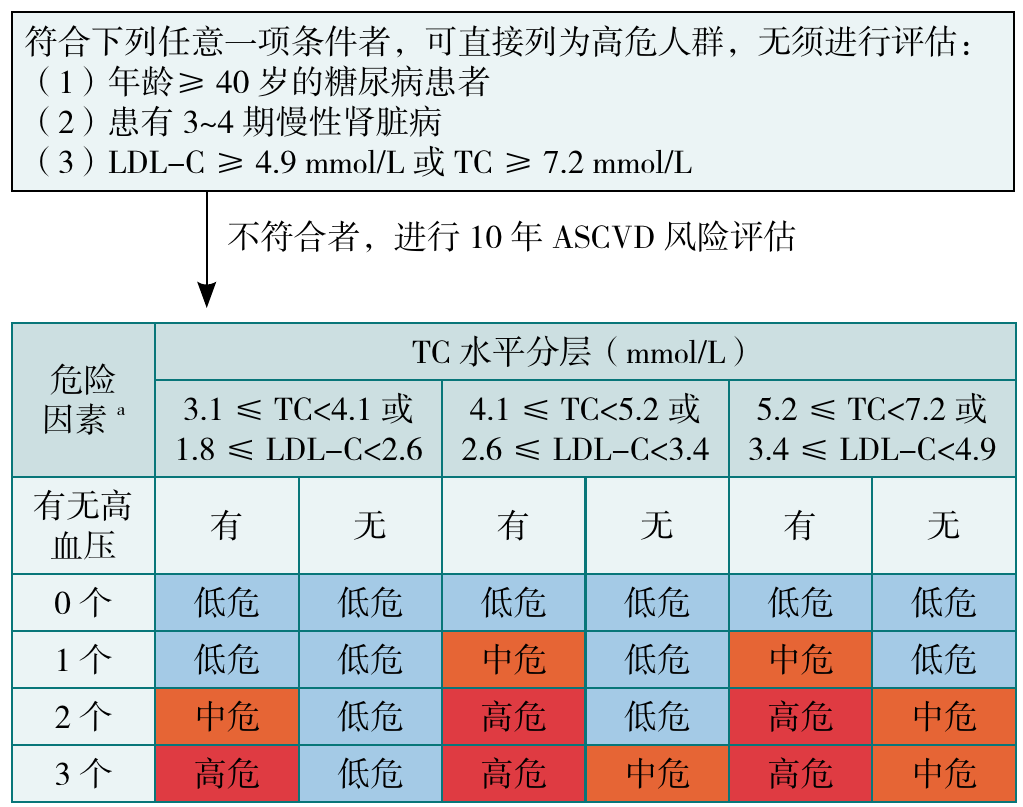
图1 中国成年人ASCVD总体风险评估流程图注:ASCVD=动脉粥样硬化性心血管疾病,LDL-C=低密度脂蛋白胆固醇,TC=总胆固醇;a表示危险因素的水平均为干预前水平,包括吸烟、LDL-C、年龄≥45/55岁(男性/女性);低危=风险度<5%,中危=风险度为5%~9%,高危=风险度≥10%。
Figure 1 Overall risk assessment process for ASCVD in Chinese adults
| 临床指标 | 治疗前 | 治疗3个月 | 检验统计量值 | P值 |
|---|---|---|---|---|
| ASCVD风险[例(%)] | 21.109a | <0.001 | ||
| 低危 | 114(66.3) | 150(87.2) | ||
| 中高危 | 58(33.7) | 22(12.8) | ||
| 体质量[M(P25,P75),kg] | 89.8(82.0,101.2) | 82.5(72.9,91.9) | -9.254 | <0.001 |
| BMI[M(P25,P75),kg/m2] | 31.6(30.0,33.9) | 28.8(27.0,30.7) | -10.238 | <0.001 |
| 腰围[M(P25,P75),cm] | 101.3(95.0,109.8) | 94(88.1,101.0) | -8.950 | <0.001 |
| 腰高比[M(P25,P75)] | 0.6(0.5,0.6) | 0.5(0.5,0.6) | -8.958 | <0.001 |
| 体脂肪[M(P25,P75),kg] | 34.3(29.9,39.5) | 28(22.8,32.7) | -9.565 | <0.001 |
| 体脂百分比[M(P25,P75),%] | 39.2(34.4,43.0) | 34.2(28.4,39.7) | -8.849 | <0.001 |
| FMI[M(P25,P75),kg/m2] | 12.2(10.5,13.8) | 10.0(7.9,11.4) | -8.923 | <0.001 |
| VFA[M(P25,P75),cm2] | 166.5(141.5,186.8) | 131.5(96.7,157.8) | -5.361 | <0.001 |
| ASMI[M(P25,P75),kg/m2] | 8.1(7.5,8.9) | 7.9(7.2,8.7) | -4.981 | <0.001 |
| 总肌肉量[M(P25,P75),kg] | 51.9(45.8,60.0) | 50.6(43.7,59.0) | -9.586 | <0.001 |
| 心率( | 89.5±12.4 | 88.9±12.5 | 0.487b | 0.627 |
| SBP( | 129±12 | 121±11 | 7.633b | <0.001 |
| DBP( | 83±10 | 78±9 | 5.093b | <0.001 |
| FBG [M(P25,P75),mmol/L] | 5.4(4.9,5.8) | 4.9(4.6,5.2) | -7.070 | <0.001 |
| 2 hFBG[M(P25,P75),mmol/L] | 7.9(6.6,9.8) | 6.4(5.4,7.1) | -7.157 | <0.001 |
| FINS[M(P25,P75),mU/L] | 17.5(13.3,26.9) | 13.3(8.8,17.1) | -7.075 | <0.001 |
| 2 hFINS[M(P25,P75),mU/L] | 126.8(88.5,202.7) | 87.7(56.3,118.7) | -5.556 | <0.001 |
| HOMA-IR [M(P25,P75)] | 4.1(3.1,6.4) | 2.4(1.0,3.5) | -8.600 | <0.001 |
| TG[M(P25,P75),mmol/L] | 1.8(1.3,2.3) | 1.3(0.9,1.7) | -6.489 | <0.001 |
| TC[M(P25,P75),mmol/L] | 4.8(4.4,5.5) | 4.5(3.9,4.9) | -4.716 | <0.001 |
| HDL-C[M(P25,P75),mmol/L] | 1.1(0.9,1.3) | 1.1(1.0,1.2) | -0.783 | 0.434 |
| LDL-C[M(P25,P75),mmol/L] | 3.1(2.6,3.5) | 2.6(2.2,3.0) | -6.787 | <0.001 |
| UA( | 428.4±122.9 | 383.3±95.0 | 3.497b | <0.001 |
| ALT[M(P25,P75),U/L] | 42.2(22.4,69.5) | 25.6(16.6,38.3) | -7.220 | <0.001 |
| AST[M(P25,P75),U/L] | 25.6(19.5,38.5) | 21.0(16.8,26.5) | -5.569 | <0.001 |
表1 研究对象治疗前与治疗3个月后各临床指标变化(n=172)
Table 1 Changes in various clinical indicators before treatment and after 3 months of treatment in the study subjects
| 临床指标 | 治疗前 | 治疗3个月 | 检验统计量值 | P值 |
|---|---|---|---|---|
| ASCVD风险[例(%)] | 21.109a | <0.001 | ||
| 低危 | 114(66.3) | 150(87.2) | ||
| 中高危 | 58(33.7) | 22(12.8) | ||
| 体质量[M(P25,P75),kg] | 89.8(82.0,101.2) | 82.5(72.9,91.9) | -9.254 | <0.001 |
| BMI[M(P25,P75),kg/m2] | 31.6(30.0,33.9) | 28.8(27.0,30.7) | -10.238 | <0.001 |
| 腰围[M(P25,P75),cm] | 101.3(95.0,109.8) | 94(88.1,101.0) | -8.950 | <0.001 |
| 腰高比[M(P25,P75)] | 0.6(0.5,0.6) | 0.5(0.5,0.6) | -8.958 | <0.001 |
| 体脂肪[M(P25,P75),kg] | 34.3(29.9,39.5) | 28(22.8,32.7) | -9.565 | <0.001 |
| 体脂百分比[M(P25,P75),%] | 39.2(34.4,43.0) | 34.2(28.4,39.7) | -8.849 | <0.001 |
| FMI[M(P25,P75),kg/m2] | 12.2(10.5,13.8) | 10.0(7.9,11.4) | -8.923 | <0.001 |
| VFA[M(P25,P75),cm2] | 166.5(141.5,186.8) | 131.5(96.7,157.8) | -5.361 | <0.001 |
| ASMI[M(P25,P75),kg/m2] | 8.1(7.5,8.9) | 7.9(7.2,8.7) | -4.981 | <0.001 |
| 总肌肉量[M(P25,P75),kg] | 51.9(45.8,60.0) | 50.6(43.7,59.0) | -9.586 | <0.001 |
| 心率( | 89.5±12.4 | 88.9±12.5 | 0.487b | 0.627 |
| SBP( | 129±12 | 121±11 | 7.633b | <0.001 |
| DBP( | 83±10 | 78±9 | 5.093b | <0.001 |
| FBG [M(P25,P75),mmol/L] | 5.4(4.9,5.8) | 4.9(4.6,5.2) | -7.070 | <0.001 |
| 2 hFBG[M(P25,P75),mmol/L] | 7.9(6.6,9.8) | 6.4(5.4,7.1) | -7.157 | <0.001 |
| FINS[M(P25,P75),mU/L] | 17.5(13.3,26.9) | 13.3(8.8,17.1) | -7.075 | <0.001 |
| 2 hFINS[M(P25,P75),mU/L] | 126.8(88.5,202.7) | 87.7(56.3,118.7) | -5.556 | <0.001 |
| HOMA-IR [M(P25,P75)] | 4.1(3.1,6.4) | 2.4(1.0,3.5) | -8.600 | <0.001 |
| TG[M(P25,P75),mmol/L] | 1.8(1.3,2.3) | 1.3(0.9,1.7) | -6.489 | <0.001 |
| TC[M(P25,P75),mmol/L] | 4.8(4.4,5.5) | 4.5(3.9,4.9) | -4.716 | <0.001 |
| HDL-C[M(P25,P75),mmol/L] | 1.1(0.9,1.3) | 1.1(1.0,1.2) | -0.783 | 0.434 |
| LDL-C[M(P25,P75),mmol/L] | 3.1(2.6,3.5) | 2.6(2.2,3.0) | -6.787 | <0.001 |
| UA( | 428.4±122.9 | 383.3±95.0 | 3.497b | <0.001 |
| ALT[M(P25,P75),U/L] | 42.2(22.4,69.5) | 25.6(16.6,38.3) | -7.220 | <0.001 |
| AST[M(P25,P75),U/L] | 25.6(19.5,38.5) | 21.0(16.8,26.5) | -5.569 | <0.001 |
| 指标 | 低危组(n=114) | 中高危组(n=58) | 检验统计量值 | P值 |
|---|---|---|---|---|
| 性别[例(%)] | 0.726a | 0.079 | ||
| 男 | 43(37.7) | 30(51.7) | ||
| 女 | 71(62.3) | 28(48.3) | ||
| 年龄[M(P25,P75),岁] | 31.0(27.0,37.3) | 34.0(28.0,39.3) | -1.261 | 0.207 |
| 身高[M(P25,P75),cm] | 166.0(162.0,174.3) | 170.0(164.5,178.0) | -1.912 | 0.056 |
| 体质量[M(P25,P75),kg] | 89.6(80.0,99.1) | 91.4(83.7,105.2) | -1.817 | 0.069 |
| BMI[M(P25,P75),kg/m2] | 31.5(29.9,33.5) | 31.85(29.9,34.3) | -1.119 | 0.263 |
| 腰围[M(P25,P75),cm] | 100(94,109) | 102(96,110) | -1.152 | 0.249 |
| 腰高比[M(P25,P75)] | 0.6(0.6,0.6) | 0.6(0.6,0.7) | -0.321 | 0.748 |
| 体脂肪[M(P25,P75),kg] | 34.1(28.7,38.7) | 34.6(31.2,40.5) | -1.485 | 0.266 |
| 体脂百分比[M(P25,P75),%] | 39.7(33.7,43.0) | 37.8(34.8,43.0) | -0.117 | 0.952 |
| FMI[M(P25,P75),kg/m2] | 12.2(10.4,13.7) | 12.2(10.6,14.0) | -0.536 | 0.642 |
| VFA[M(P25,P75),cm2] | 165.5(133.3,186.0) | 168.9(147.0,190.9) | -0.943 | 0.485 |
| ASMI[M(P25,P75),kg/m2] | 8.1(7.5,8.9) | 8.3(7.7,9.2) | -0.913 | 0.361 |
| 总肌肉量[M(P25,P75),kg] | 50.1(45.1,59.2) | 54.5(46.5,62.8) | -1.527 | 0.144 |
| 心率( | 89.6±13.4 | 89.5±10.4 | 0.055b | 0.959 |
| SBP( | 129±12 | 129±12 | -0.233b | 0.816 |
| DBP( | 82±11 | 84±9 | -0.752b | 0.453 |
| FBG [M(P25,P75),mmol/L] | 5.2(4.9,5.6) | 5.5(4.9,6.2) | -2.034 | 0.019 |
| 2 hFBG[M(P25,P75),mmol/L] | 7.4(6.5,8.7) | 8.4(6.9,11.4) | -2.541 | 0.011 |
| FINS[M(P25,P75),mU/L] | 16.8(13.2,26.8) | 21.7(13.2,33.2) | -1.769 | 0.242 |
| 2 hFINS[M(P25,P75),mU/L] | 115.5(84.7,208.3) | 156.1(109.0,237.5) | -2.476 | 0.041 |
| HOMA-IR [M(P25,P75)] | 4.1(3.1,6.2) | 5.3(3.2,8.6) | -2.471 | 0.004 |
| TG[M(P25,P75),mmol/L] | 1.6(1.3,2.2) | 2.1(1.5,3.4) | -3.276 | 0.001 |
| TC[M(P25,P75),mmol/L] | 4.8(4.2,5.2) | 5.2(4.6,5.9) | -3.252 | 0.001 |
| HDL-C[M(P25,P75),mmol/L] | 1.1(1.1,1.3) | 1.0(0.8,1.2) | -3.524 | <0.001 |
| LDL-C[M(P25,P75),mmol/L] | 3.1(2.5,3.4) | 3.4(2.9,3.7) | -2.946 | 0.003 |
| UA[M(P25,P75),mU/L] | 425.0(342.5,465.5) | 430.9(334.5,511.5) | -0.763 | 0.359 |
| ALT[M(P25,P75),U/L] | 38.4(21.0,62.6) | 50.0(28.0,89.7) | -2.350 | 0.022 |
| AST[M(P25,P75),U/L] | 24.6(18.4,36.8) | 29.3(20.3,54.5) | -2.411 | 0.022 |
表2 ASCVD低危组与中高危组患者治疗前临床指标比较
Table 2 Comparison of clinical indicators before treatment between low-risk group and moderate-high risk group ASCVD patients
| 指标 | 低危组(n=114) | 中高危组(n=58) | 检验统计量值 | P值 |
|---|---|---|---|---|
| 性别[例(%)] | 0.726a | 0.079 | ||
| 男 | 43(37.7) | 30(51.7) | ||
| 女 | 71(62.3) | 28(48.3) | ||
| 年龄[M(P25,P75),岁] | 31.0(27.0,37.3) | 34.0(28.0,39.3) | -1.261 | 0.207 |
| 身高[M(P25,P75),cm] | 166.0(162.0,174.3) | 170.0(164.5,178.0) | -1.912 | 0.056 |
| 体质量[M(P25,P75),kg] | 89.6(80.0,99.1) | 91.4(83.7,105.2) | -1.817 | 0.069 |
| BMI[M(P25,P75),kg/m2] | 31.5(29.9,33.5) | 31.85(29.9,34.3) | -1.119 | 0.263 |
| 腰围[M(P25,P75),cm] | 100(94,109) | 102(96,110) | -1.152 | 0.249 |
| 腰高比[M(P25,P75)] | 0.6(0.6,0.6) | 0.6(0.6,0.7) | -0.321 | 0.748 |
| 体脂肪[M(P25,P75),kg] | 34.1(28.7,38.7) | 34.6(31.2,40.5) | -1.485 | 0.266 |
| 体脂百分比[M(P25,P75),%] | 39.7(33.7,43.0) | 37.8(34.8,43.0) | -0.117 | 0.952 |
| FMI[M(P25,P75),kg/m2] | 12.2(10.4,13.7) | 12.2(10.6,14.0) | -0.536 | 0.642 |
| VFA[M(P25,P75),cm2] | 165.5(133.3,186.0) | 168.9(147.0,190.9) | -0.943 | 0.485 |
| ASMI[M(P25,P75),kg/m2] | 8.1(7.5,8.9) | 8.3(7.7,9.2) | -0.913 | 0.361 |
| 总肌肉量[M(P25,P75),kg] | 50.1(45.1,59.2) | 54.5(46.5,62.8) | -1.527 | 0.144 |
| 心率( | 89.6±13.4 | 89.5±10.4 | 0.055b | 0.959 |
| SBP( | 129±12 | 129±12 | -0.233b | 0.816 |
| DBP( | 82±11 | 84±9 | -0.752b | 0.453 |
| FBG [M(P25,P75),mmol/L] | 5.2(4.9,5.6) | 5.5(4.9,6.2) | -2.034 | 0.019 |
| 2 hFBG[M(P25,P75),mmol/L] | 7.4(6.5,8.7) | 8.4(6.9,11.4) | -2.541 | 0.011 |
| FINS[M(P25,P75),mU/L] | 16.8(13.2,26.8) | 21.7(13.2,33.2) | -1.769 | 0.242 |
| 2 hFINS[M(P25,P75),mU/L] | 115.5(84.7,208.3) | 156.1(109.0,237.5) | -2.476 | 0.041 |
| HOMA-IR [M(P25,P75)] | 4.1(3.1,6.2) | 5.3(3.2,8.6) | -2.471 | 0.004 |
| TG[M(P25,P75),mmol/L] | 1.6(1.3,2.2) | 2.1(1.5,3.4) | -3.276 | 0.001 |
| TC[M(P25,P75),mmol/L] | 4.8(4.2,5.2) | 5.2(4.6,5.9) | -3.252 | 0.001 |
| HDL-C[M(P25,P75),mmol/L] | 1.1(1.1,1.3) | 1.0(0.8,1.2) | -3.524 | <0.001 |
| LDL-C[M(P25,P75),mmol/L] | 3.1(2.5,3.4) | 3.4(2.9,3.7) | -2.946 | 0.003 |
| UA[M(P25,P75),mU/L] | 425.0(342.5,465.5) | 430.9(334.5,511.5) | -0.763 | 0.359 |
| ALT[M(P25,P75),U/L] | 38.4(21.0,62.6) | 50.0(28.0,89.7) | -2.350 | 0.022 |
| AST[M(P25,P75),U/L] | 24.6(18.4,36.8) | 29.3(20.3,54.5) | -2.411 | 0.022 |
| 临床指标 | 治疗前 | 治疗3个月 | 组间评估平均差异(95%CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 中高危降低亚组(n=36) | 中高危不变亚组(n=22) | 检验统计量值 | P值 | 中高危降低亚组(n=36) | 中高危不变亚组(n=22) | 检验统计量值 | P值 | ||
| 体质量[M(P25,P75),kg] | 91.4(83.8,102.1) | 95.8(83.7,113.4) | -1.034b | 0.301 | 83.9(73.1,93.9)a | 84.6(76.8,102.7)a | -1.178b | 0.239 | 0.277(-9.573 ~10.127) |
| TWL( | 8.9±3.4 | 8.7±2.8 | 0.147 | 0.055 | |||||
| TWL≥5%[例(%)] | 22(61.1) | 12(54.5) | 0.243c | 0.622 | |||||
| TWL≥10%[例(%)] | 17(47.2) | 9(40.9) | 0.220c | 0.639 | |||||
| BMI( | 31.9±3.1 | 33.9±3.5 | -2.312 | 0.024 | 28.8±2.9a | 30.9±3.3a | -2.574 | 0.037 | 0.127(-2.114~2.367) |
| 腰围( | 102.6±9.9 | 105.9±12.3 | -1.134 | 0.262 | 96.7±10.1a | 98.4±12.3a | -0.575 | 0.568 | -1.630(-8.619~5.359) |
| 腰高比( | 0.6±0.1 | 0.6±0.1 | -1.125 | 0.186 | 0.6±0.1a | 0.6±0.1a | -0.621 | 0.389 | -0.009(-0.050~0.032) |
| 体脂肪( | 33.4±8.3 | 39.9±8.1 | -3.016 | 0.004 | 27.7±7.8a | 32.6±6.9a | -2.440 | 0.043 | -0.998(-6.461~4.464) |
| 体脂百分比( | 38.0±7.8 | 40.6±5.4 | -2.604 | 0.012 | 32.6±5.8a | 36.5±6.1* | -2.388 | 0.020 | 0.206(-4.218~4.629) |
| FMI( | 11.4±2.9 | 13.9±2.9 | -3.379 | 0.001 | 9.5±2.6a | 11.3±2.5a | -2.660 | 0.017 | -0.371(-2.299~1.557) |
| VFA( | 155.9±43.6 | 185.9±32.5 | -2.834 | 0.006 | 126.1±38.6a | 151.5±33.9a | -2.540 | 0.021 | -0.770(-28.099~26.558) |
| ASMI[M(P25,P75),kg/m2] | 8.2(7.3,9.0) | 8.5(7.7,9.5) | -1.194b | 0.233 | 8.1(7.4,8.8) | 8.1(7.4,9.2) | -0.288b | 0.868 | -0.497(-1.234~0.239) |
| 总肌肉量( | 54.7±10.4 | 55.3±10.8 | -0.118 | 0.906 | 54.2±10.1 | 53.9±11.7 | 0.064 | 0.949 | -0.516(-6.832~5.799) |
| 心率( | 88.7±10.0 | 90.7±11.0 | -0.711 | 0.480 | 87.3±13.0 | 89.7±12.0 | -0.725 | 0.471 | 0.391(-8.012~8.794) |
| SBP( | 128.9±12.8 | 128.8 ±9.6 | 0.041 | 0.968 | 119.1±12.1a | 124.9±10.3 | -1.889 | 0.064 | 5.976(-1.869~13.822) |
| DBP( | 84.2±9.0 | 82.5±9.6 | 0.682 | 0.498 | 78.0±10.7a | 79.8±9.2 | -0.655 | 0.515 | 3.504(-4.098~11.106) |
| FBG [M(P25,P75),mmol/L] | 5.5(5.0,6.7) | 5.5(4.7,6.5) | -0.687b | 0.575 | 5.0(4.7,5.4)a | 5.0(4.7,5.5) | -0.096b | 0.923 | 0.083(-1.412~1.577) |
| 2 hFBG[M(P25,P75),mmol/L] | 8.2(6.5,12.0) | 9.0(7.6,11.4) | -0.874b | 0.382 | 5.9(5.1,8.3) | 6.5(5.9,7.2)a | -0.849b | 0.396 | 0.186(-3.367~3.739) |
| FINS[M(P25,P75),mU/L] | 17.3(11.4,27.2) | 25.3(15.9,37.1) | -2.067b | 0.039 | 12.5(8.1,18.0)a | 15.9(11.2,22.3)a | -0.860b | 0.410 | -0.612(-13.812~12.588) |
| 2 hFINS( | 178.8±143.7 | 189.7±86.6 | -0.222 | 0.259 | 97.8±105.6a | 102.0±58.0a | -0.144 | 0.196 | 2.139(-85.107~89.384) |
| HOMA-IR [M(P25,P75)] | 4.8(3.2,7.5) | 6.2(3.4,10.9) | -0.902b | 0.178 | 2.9(1.6,4.0)a | 3.6(2.6,4.9)a | -0.578b | 0.088 | -0.207(-4.633~4.219) |
| TG[M(P25,P75),mmol/L] | 2.3(1.8,4.0) | 1.9(1.4,2.4) | -1.547b | 0.122 | 1.3(1.1,2.1)a | 1.5(1.0,1.9)a | -0.289b | 0.773 | 0.047(-1.257~1.351) |
| TC( | 5.2±1.7 | 5.1±0.8 | 0.066 | 0.466 | 4.5±1.0a | 4.9±0.6 | -1.591 | 0.074 | 0.408(-0.289~1.105) |
| HDL-C[M(P25,P75),mmol/L] | 1.1(0.8,1.4) | 0.9(0.8,1.1) | -2.052b | 0.040 | 1.1(0.9,1.2) | 1.0(0.9,1.1) | -1.515b | 0.990 | 0.278(0.010~0.545) |
| LDL-C( | 3.5±1.2 | 3.2±0.7 | 1.240 | 0.248 | 2.7±0.9a | 2.8±0.6 | -0.720 | 0.475 | 0.497(-0.109~1.105) |
| UA( | 444.5±115.5 | 443.2±159.1 | 0.072 | 0.973 | 404.2±124.0 | 392.4±101.6 | 0.387 | 0.974 | -16.362(-101.797~69.073) |
| ALT [M(P25,P75),U/L] | 48.5(23.5,118.1) | 48.5(32.2,88.8) | -0.706b | 0.841 | 26.0(17.6,40.8)a | 29.4(20.2,51.7)a | -0.215b | 0.654 | -3.427(-46.702~39.845) |
| AST[M(P25,P75),U/L] | 29.1(20.5,63.2) | 25.4(20.3,48.6) | -0.045b | 0.537 | 21.6(17.7,30.2)a | 21.9(17.8,31.8)a | -0.127b | 0.847 | 10.278(-24.631~45.189) |
表3 中高危ASCVD风险患者治疗3个月后ASCVD风险降低组与不变组各指标比较
Table 3 Comparison of indicators between the risk decreased group and the risk stable group after 3 months treatment in patients with moderate-high ASCVD risk
| 临床指标 | 治疗前 | 治疗3个月 | 组间评估平均差异(95%CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 中高危降低亚组(n=36) | 中高危不变亚组(n=22) | 检验统计量值 | P值 | 中高危降低亚组(n=36) | 中高危不变亚组(n=22) | 检验统计量值 | P值 | ||
| 体质量[M(P25,P75),kg] | 91.4(83.8,102.1) | 95.8(83.7,113.4) | -1.034b | 0.301 | 83.9(73.1,93.9)a | 84.6(76.8,102.7)a | -1.178b | 0.239 | 0.277(-9.573 ~10.127) |
| TWL( | 8.9±3.4 | 8.7±2.8 | 0.147 | 0.055 | |||||
| TWL≥5%[例(%)] | 22(61.1) | 12(54.5) | 0.243c | 0.622 | |||||
| TWL≥10%[例(%)] | 17(47.2) | 9(40.9) | 0.220c | 0.639 | |||||
| BMI( | 31.9±3.1 | 33.9±3.5 | -2.312 | 0.024 | 28.8±2.9a | 30.9±3.3a | -2.574 | 0.037 | 0.127(-2.114~2.367) |
| 腰围( | 102.6±9.9 | 105.9±12.3 | -1.134 | 0.262 | 96.7±10.1a | 98.4±12.3a | -0.575 | 0.568 | -1.630(-8.619~5.359) |
| 腰高比( | 0.6±0.1 | 0.6±0.1 | -1.125 | 0.186 | 0.6±0.1a | 0.6±0.1a | -0.621 | 0.389 | -0.009(-0.050~0.032) |
| 体脂肪( | 33.4±8.3 | 39.9±8.1 | -3.016 | 0.004 | 27.7±7.8a | 32.6±6.9a | -2.440 | 0.043 | -0.998(-6.461~4.464) |
| 体脂百分比( | 38.0±7.8 | 40.6±5.4 | -2.604 | 0.012 | 32.6±5.8a | 36.5±6.1* | -2.388 | 0.020 | 0.206(-4.218~4.629) |
| FMI( | 11.4±2.9 | 13.9±2.9 | -3.379 | 0.001 | 9.5±2.6a | 11.3±2.5a | -2.660 | 0.017 | -0.371(-2.299~1.557) |
| VFA( | 155.9±43.6 | 185.9±32.5 | -2.834 | 0.006 | 126.1±38.6a | 151.5±33.9a | -2.540 | 0.021 | -0.770(-28.099~26.558) |
| ASMI[M(P25,P75),kg/m2] | 8.2(7.3,9.0) | 8.5(7.7,9.5) | -1.194b | 0.233 | 8.1(7.4,8.8) | 8.1(7.4,9.2) | -0.288b | 0.868 | -0.497(-1.234~0.239) |
| 总肌肉量( | 54.7±10.4 | 55.3±10.8 | -0.118 | 0.906 | 54.2±10.1 | 53.9±11.7 | 0.064 | 0.949 | -0.516(-6.832~5.799) |
| 心率( | 88.7±10.0 | 90.7±11.0 | -0.711 | 0.480 | 87.3±13.0 | 89.7±12.0 | -0.725 | 0.471 | 0.391(-8.012~8.794) |
| SBP( | 128.9±12.8 | 128.8 ±9.6 | 0.041 | 0.968 | 119.1±12.1a | 124.9±10.3 | -1.889 | 0.064 | 5.976(-1.869~13.822) |
| DBP( | 84.2±9.0 | 82.5±9.6 | 0.682 | 0.498 | 78.0±10.7a | 79.8±9.2 | -0.655 | 0.515 | 3.504(-4.098~11.106) |
| FBG [M(P25,P75),mmol/L] | 5.5(5.0,6.7) | 5.5(4.7,6.5) | -0.687b | 0.575 | 5.0(4.7,5.4)a | 5.0(4.7,5.5) | -0.096b | 0.923 | 0.083(-1.412~1.577) |
| 2 hFBG[M(P25,P75),mmol/L] | 8.2(6.5,12.0) | 9.0(7.6,11.4) | -0.874b | 0.382 | 5.9(5.1,8.3) | 6.5(5.9,7.2)a | -0.849b | 0.396 | 0.186(-3.367~3.739) |
| FINS[M(P25,P75),mU/L] | 17.3(11.4,27.2) | 25.3(15.9,37.1) | -2.067b | 0.039 | 12.5(8.1,18.0)a | 15.9(11.2,22.3)a | -0.860b | 0.410 | -0.612(-13.812~12.588) |
| 2 hFINS( | 178.8±143.7 | 189.7±86.6 | -0.222 | 0.259 | 97.8±105.6a | 102.0±58.0a | -0.144 | 0.196 | 2.139(-85.107~89.384) |
| HOMA-IR [M(P25,P75)] | 4.8(3.2,7.5) | 6.2(3.4,10.9) | -0.902b | 0.178 | 2.9(1.6,4.0)a | 3.6(2.6,4.9)a | -0.578b | 0.088 | -0.207(-4.633~4.219) |
| TG[M(P25,P75),mmol/L] | 2.3(1.8,4.0) | 1.9(1.4,2.4) | -1.547b | 0.122 | 1.3(1.1,2.1)a | 1.5(1.0,1.9)a | -0.289b | 0.773 | 0.047(-1.257~1.351) |
| TC( | 5.2±1.7 | 5.1±0.8 | 0.066 | 0.466 | 4.5±1.0a | 4.9±0.6 | -1.591 | 0.074 | 0.408(-0.289~1.105) |
| HDL-C[M(P25,P75),mmol/L] | 1.1(0.8,1.4) | 0.9(0.8,1.1) | -2.052b | 0.040 | 1.1(0.9,1.2) | 1.0(0.9,1.1) | -1.515b | 0.990 | 0.278(0.010~0.545) |
| LDL-C( | 3.5±1.2 | 3.2±0.7 | 1.240 | 0.248 | 2.7±0.9a | 2.8±0.6 | -0.720 | 0.475 | 0.497(-0.109~1.105) |
| UA( | 444.5±115.5 | 443.2±159.1 | 0.072 | 0.973 | 404.2±124.0 | 392.4±101.6 | 0.387 | 0.974 | -16.362(-101.797~69.073) |
| ALT [M(P25,P75),U/L] | 48.5(23.5,118.1) | 48.5(32.2,88.8) | -0.706b | 0.841 | 26.0(17.6,40.8)a | 29.4(20.2,51.7)a | -0.215b | 0.654 | -3.427(-46.702~39.845) |
| AST[M(P25,P75),U/L] | 29.1(20.5,63.2) | 25.4(20.3,48.6) | -0.045b | 0.537 | 21.6(17.7,30.2)a | 21.9(17.8,31.8)a | -0.127b | 0.847 | 10.278(-24.631~45.189) |
| 变量 | 单因素Logistic回归分析 | 多因素Logistic回归分析 | ||
|---|---|---|---|---|
| OR(95%CI) | P值 | OR(95%CI) | P值 | |
| 年龄 | 0.949(0.888~1.014) | 0.118 | ||
| 身高 | 0.988(0.929~1.063) | 0.712 | ||
| 体质量 | 1.022(0.987~1.058) | 0.218 | ||
| BMI | 1.257(1.034~1.528) | 0.022 | 1.257(1.034~1.528) | 0.022 |
| 腰围 | 1.015(0.966~1.066) | 0.561 | ||
| 腰高比 | 0.707(1.582~3.542) | 0.265 | ||
| 体脂肪 | 1.094(1.011~1.184) | 0.026 | ||
| 体脂百分比 | 1.117(1.013~1.231) | 0.026 | ||
| FMI | 1.324(1.055~1.661) | 0.016 | ||
| ASMI | 1.047(0.618~1.775) | 0.865 | ||
| 总肌肉量 | 0.998(0.949~1.050) | 0.948 | ||
| VFA | 1.019(1.003~1.035) | 0.020 | ||
| 心率 | 1.017(0.973~1.063) | 0.464 | ||
| 高血压 | 3.235(0.689~15.187) | 0.137 | ||
| FBG | 0.798(0.386~1.653) | 0.544 | ||
| 2 hFBG | 0.980(0.797~1.205) | 0.849 | ||
| FINS | 1.040(0.953~1.133) | 0.380 | ||
| 2 hFINS | 1.000(0.994~1.007) | 0.883 | ||
| HOMA-IR | 1.027(0.802~1.315) | 0.832 | ||
| TG | 0.946(0.445~2.011) | 0.885 | ||
| TC | 1.696(0.856~3.361) | 0.130 | ||
| HDL-C | 0.587(0.070~4.947) | 0.625 | ||
| LDL-C | 1.533(0.700~3.355) | 0.285 | ||
| UA | 0.999(0.994~1.004) | 0.694 | ||
| ALT | 0.993(0.973~1.014) | 0.521 | ||
| AST | 0.996(0.958~1.036) | 0.852 | ||
| 吸烟史 | 0.524(0.051~5.375) | 0.586 | ||
表4 肥胖中高危ASCVD患者转为低风险患者影响因素的单因素和多因素Logistic回归分析
Table 4 Univariate and multivariate Logistic regression analysis of patients with medium-high ASCVD risk converted into low ASCVD risk
| 变量 | 单因素Logistic回归分析 | 多因素Logistic回归分析 | ||
|---|---|---|---|---|
| OR(95%CI) | P值 | OR(95%CI) | P值 | |
| 年龄 | 0.949(0.888~1.014) | 0.118 | ||
| 身高 | 0.988(0.929~1.063) | 0.712 | ||
| 体质量 | 1.022(0.987~1.058) | 0.218 | ||
| BMI | 1.257(1.034~1.528) | 0.022 | 1.257(1.034~1.528) | 0.022 |
| 腰围 | 1.015(0.966~1.066) | 0.561 | ||
| 腰高比 | 0.707(1.582~3.542) | 0.265 | ||
| 体脂肪 | 1.094(1.011~1.184) | 0.026 | ||
| 体脂百分比 | 1.117(1.013~1.231) | 0.026 | ||
| FMI | 1.324(1.055~1.661) | 0.016 | ||
| ASMI | 1.047(0.618~1.775) | 0.865 | ||
| 总肌肉量 | 0.998(0.949~1.050) | 0.948 | ||
| VFA | 1.019(1.003~1.035) | 0.020 | ||
| 心率 | 1.017(0.973~1.063) | 0.464 | ||
| 高血压 | 3.235(0.689~15.187) | 0.137 | ||
| FBG | 0.798(0.386~1.653) | 0.544 | ||
| 2 hFBG | 0.980(0.797~1.205) | 0.849 | ||
| FINS | 1.040(0.953~1.133) | 0.380 | ||
| 2 hFINS | 1.000(0.994~1.007) | 0.883 | ||
| HOMA-IR | 1.027(0.802~1.315) | 0.832 | ||
| TG | 0.946(0.445~2.011) | 0.885 | ||
| TC | 1.696(0.856~3.361) | 0.130 | ||
| HDL-C | 0.587(0.070~4.947) | 0.625 | ||
| LDL-C | 1.533(0.700~3.355) | 0.285 | ||
| UA | 0.999(0.994~1.004) | 0.694 | ||
| ALT | 0.993(0.973~1.014) | 0.521 | ||
| AST | 0.996(0.958~1.036) | 0.852 | ||
| 吸烟史 | 0.524(0.051~5.375) | 0.586 | ||
| 变量 | 治疗前 | 治疗3个月 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 利拉鲁肽组(n=51) | 二甲双胍组(n=61) | 未用药组(n=60) | 检验统计量值 | P值 | 利拉鲁肽组(n=51) | 二甲双胍组(n=61) | 未用药组(n=60) | 检验统计量值 | P值 | |
| 性别(男/女) | 24/27 | 26/35 | 22/38 | 1.246c | 0.536 | |||||
| ASCVD风险(低危/中高危) | 34/17 | 41/20 | 42/18 | 0.169c | 0.919 | 46/5a | 53/8a | 53/7a | 0.296c | 0.862 |
| 年龄[M(P25,P75),岁] | 31(26,37) | 31(28,39) | 32(29,40) | 1.931 | 0.292 | |||||
| 身高[M(P25,P75),cm] | 170(165,177) | 167(163,174) | 168(163,177) | 0.976 | 0.602 | |||||
| 体质量[M(P25,P75),kg] | 93.3(84.1,102.6) | 91.1(82.6,101.3) | 89.3(81.4,102.7) | 0.988 | 0.505 | 85.6(73.4,96.1)a | 82.7(72.4,92.2)a | 81(73.3,87.7)a | 2.103 | 0.519 |
| TWL[M(P25,P75),%] | 9.4(4.6,12.9) | 9.9(1.1,21.7) | 7.4(7.8,21.8) | 0.041 | 0.960 | |||||
| TWL≥5%[例(%)] | 36.0(70.5) | 37.0(60.7) | 41.0(68.3) | 1.400c | 0.497 | |||||
| TWL≥10%[例(%)] | 24.0(47.1) | 29.0(47.5) | 31.0(51.7) | 0.298c | 0.862 | |||||
| BMI[M(P25,P75),kg/m2] | 32.1(30.5,34.1) | 31.3(29.6,33.8) | 31.1(30.1,34.3) | 2.745 | 0.626 | 28.8(27.5,30.8)a | 28.8(26.4,30.8)* | 28.6(26.9,30.5)a | 1.285 | 0.519 |
| 腰围[M(P25,P75),cm] | 104.5(98.3,112.3) | 102.5(95.5,109.8) | 101.0(95.0,110.0) | 2.223 | 0.179 | 95.5(90.0,103.8)a | 93.0(88.3,97.8)a | 93.0(86.0,100.0)a | 4.073 | 0.161 |
| 腰高比[M(P25,P75)] | 0.6(0.6,0.6) | 0.6(0.6,0.6) | 0.6(0.6,0.6) | 0.570 | 0.251 | 0.6(0.5,0.6)a | 0.6(0.5,0.6)* | 0.5(0.5,0.6)a | 3.772 | 0.359 |
| 体脂肪[M(P25,P75),kg] | 34.2(31.3,40.0) | 34.2(29.8,38.5) | 33.8(29.9,39.6) | 0.052 | 0.524 | 28.4(24.3,33.7)a | 27.9(21.9,33.6)a | 28(21.3,32.3)a | 1.455 | 0.432 |
| 体脂百分比( | 38.3±5.8 | 38.2±5.9 | 38.0±5.9 | 0.033b | 0.974 | 34.8±5.7a | 34.3±7.6a | 33.3±7.4a | 0.728b | 0.485 |
| FMI[M(P25,P75),kg/m2] | 12.3(10.7,13.7) | 11.9(10.4,13.9) | 12.2(10.6,13.4) | 0.191 | 0.887 | 10.3(8.5,11.0)* | 9.7(7.7,12.5)* | 9.8(7.7,11.4)* | 0.588 | 0.711 |
| VFA( | 167.3±39.3 | 165.4±35.9 | 163.2±41.5 | 0.106b | 0.986 | 135.9±36.3a | 131.8±45.1a | 130.1±44.8a | 0.609b | |
| ASMI( | 8.1±0.9 | 8.0±1.7 | 7.9±2.0 | 0.029b | 0.575 | 7.5±0.9a | 7.9±0.9a | 7.9±1.1a | 0.399b | 0.656 |
| 总肌肉量( | 55.0±9.3 | 53.4±9.6 | 53.6±9.8 | 0.237b | 0.850 | 52.4±8.8 | 50.8±8.8 | 51.8±10.5 | 0.422b | 0.545 |
表5 利拉鲁肽、二甲双胍与未用药患者治疗3个月后ASCVD风险及减重指标比较
Table 5 Comparison of ASCVD risk and weight loss indicators between liraglutide,metformin,and untreated patients after 3 months of treatment
| 变量 | 治疗前 | 治疗3个月 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 利拉鲁肽组(n=51) | 二甲双胍组(n=61) | 未用药组(n=60) | 检验统计量值 | P值 | 利拉鲁肽组(n=51) | 二甲双胍组(n=61) | 未用药组(n=60) | 检验统计量值 | P值 | |
| 性别(男/女) | 24/27 | 26/35 | 22/38 | 1.246c | 0.536 | |||||
| ASCVD风险(低危/中高危) | 34/17 | 41/20 | 42/18 | 0.169c | 0.919 | 46/5a | 53/8a | 53/7a | 0.296c | 0.862 |
| 年龄[M(P25,P75),岁] | 31(26,37) | 31(28,39) | 32(29,40) | 1.931 | 0.292 | |||||
| 身高[M(P25,P75),cm] | 170(165,177) | 167(163,174) | 168(163,177) | 0.976 | 0.602 | |||||
| 体质量[M(P25,P75),kg] | 93.3(84.1,102.6) | 91.1(82.6,101.3) | 89.3(81.4,102.7) | 0.988 | 0.505 | 85.6(73.4,96.1)a | 82.7(72.4,92.2)a | 81(73.3,87.7)a | 2.103 | 0.519 |
| TWL[M(P25,P75),%] | 9.4(4.6,12.9) | 9.9(1.1,21.7) | 7.4(7.8,21.8) | 0.041 | 0.960 | |||||
| TWL≥5%[例(%)] | 36.0(70.5) | 37.0(60.7) | 41.0(68.3) | 1.400c | 0.497 | |||||
| TWL≥10%[例(%)] | 24.0(47.1) | 29.0(47.5) | 31.0(51.7) | 0.298c | 0.862 | |||||
| BMI[M(P25,P75),kg/m2] | 32.1(30.5,34.1) | 31.3(29.6,33.8) | 31.1(30.1,34.3) | 2.745 | 0.626 | 28.8(27.5,30.8)a | 28.8(26.4,30.8)* | 28.6(26.9,30.5)a | 1.285 | 0.519 |
| 腰围[M(P25,P75),cm] | 104.5(98.3,112.3) | 102.5(95.5,109.8) | 101.0(95.0,110.0) | 2.223 | 0.179 | 95.5(90.0,103.8)a | 93.0(88.3,97.8)a | 93.0(86.0,100.0)a | 4.073 | 0.161 |
| 腰高比[M(P25,P75)] | 0.6(0.6,0.6) | 0.6(0.6,0.6) | 0.6(0.6,0.6) | 0.570 | 0.251 | 0.6(0.5,0.6)a | 0.6(0.5,0.6)* | 0.5(0.5,0.6)a | 3.772 | 0.359 |
| 体脂肪[M(P25,P75),kg] | 34.2(31.3,40.0) | 34.2(29.8,38.5) | 33.8(29.9,39.6) | 0.052 | 0.524 | 28.4(24.3,33.7)a | 27.9(21.9,33.6)a | 28(21.3,32.3)a | 1.455 | 0.432 |
| 体脂百分比( | 38.3±5.8 | 38.2±5.9 | 38.0±5.9 | 0.033b | 0.974 | 34.8±5.7a | 34.3±7.6a | 33.3±7.4a | 0.728b | 0.485 |
| FMI[M(P25,P75),kg/m2] | 12.3(10.7,13.7) | 11.9(10.4,13.9) | 12.2(10.6,13.4) | 0.191 | 0.887 | 10.3(8.5,11.0)* | 9.7(7.7,12.5)* | 9.8(7.7,11.4)* | 0.588 | 0.711 |
| VFA( | 167.3±39.3 | 165.4±35.9 | 163.2±41.5 | 0.106b | 0.986 | 135.9±36.3a | 131.8±45.1a | 130.1±44.8a | 0.609b | |
| ASMI( | 8.1±0.9 | 8.0±1.7 | 7.9±2.0 | 0.029b | 0.575 | 7.5±0.9a | 7.9±0.9a | 7.9±1.1a | 0.399b | 0.656 |
| 总肌肉量( | 55.0±9.3 | 53.4±9.6 | 53.6±9.8 | 0.237b | 0.850 | 52.4±8.8 | 50.8±8.8 | 51.8±10.5 | 0.422b | 0.545 |
| 指标 | 治疗前 | 治疗3个月 | 组间评估平均差异(95%CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 28.0 kg/m2<BMI<32.5 kg/m2组(n=105) | BMI≥32.5 kg/m2组(n=67) | Z(χ2)值 | P值 | 28.0 kg/m2<BMI<32.5 kg/m2组(n=105) | BMI ≥32.5 kg/m2组(n=67) | Z(χ2)值 | P值 | ||
| ASCVD风险(低危/中高危) | 73/32 | 41/26 | 1.270b | 0.260 | 97/8a | 52/15a | 7.702b | 0.006 | |
| TWL[M(P25,P75),%] | 8.4(4.8,12.9) | 9.9(5.8,13.9) | -1.217 | 0.224 | |||||
| TWL≥5%[例(%)] | 78.0(74.3) | 55.0(82.1) | 1.421b | 0.233 | |||||
| TWL≥10%[例(%)] | 44.0(38.1) | 34.0(50.7) | 1.290b | 0.256 | |||||
| 体质量[M(P25,P75),kg] | 84.9(78.7,91.4) | 101.9(91.0,113.2) | -7.842 | <0.001 | 77.6(70.2,85.5)a | 89.3(82.3,98.6)a | -5.726 | <0.001 | -4.555(-9.334~0.223) |
| BMI[M(P25,P75),kg/m2] | 30.4(29.5,31.4) | 34.4(33.4,36.5) | -11.047 | <0.001 | 27.8(26.4,29.0)a | 30.8(29.2,33.1)a | -6.989 | <0.001 | -1.179(-2.327~-0.031) |
| 腰围[M(P25,P75),cm] | 99.1(93.2,105.3) | 106.2(99.4,112.2) | -3.989 | <0.001 | 91.2(85.9,97.2)a | 95.8(89.7,106.3)a | -3.890 | <0.001 | 1.298(-3.123~5.721) |
| 腰高比[M(P25,P75)] | 0.6(0.6,0.6) | 0.6(0.6,0.7) | -3.515 | <0.001 | 0.5(0.5,0.6)a | 0.6(0.5,0.6)a | -2.916 | 0.004 | 0.008(-0.016~0.033) |
| 体脂肪[M(P25,P75),kg] | 31.2(28.1,34.3) | 40.5(35.8,46.9) | -8.308 | <0.001 | 26.4(21.1,29.2)a | 32.3(26.8,38.5)a | -5.351 | <0.001 | -3.232(-6.142~-0.323) |
| 体脂百分比[M(P25,P75),%] | 37.1(33.2,41.2) | 40.8(35.7,45.3) | -3.751 | <0.001 | 33.8(28.0,37.9)a | 35.7(30.3,42.5)a | -2.629 | <0.001 | -1.240(-3.951~1.470) |
| FMI[M(P25,P75),kg/m2] | 11.2(9.4,12.4) | 13.9(12.2,15.8) | -7.164 | <0.001 | 9.3(7.4,10.8)a | 10.9(8.8,13.7)a | -4.570 | <0.001 | -0.951(-1.980~0.078) |
| VFA[M(P25,P75),cm2] | 149.8(125.8,174.1) | 186.8(167.4,29.8) | -6.550 | 0.001 | 120.5(90.5,146.4)a | 151.1(112.3,175.6)a | -4.197 | <0.001 | -9.499(-24.690~5.691) |
| ASMI[M(P25,P75),kg/m2] | 7.8(7.2,8.4) | 8.9(8.0,9.4) | -5.830 | <0.001 | 7.6(6.9,8.3) | 8.3(7.6,9.1)a | -3.892 | 0.012 | -0.232(-0.763~0.298) |
| 总肌肉量[M(P25,P75),kg] | 48.9(44.1,57.8) | 56.8(49.2,65.0) | -4.255 | <0.001 | 47.7(42.9,56.8) | 54.5(46.4,61.3) | -3.012 | 0.010 | -2.321(-6.341~1.698) |
表6 以BMI分层比较治疗3个月后ASCVD风险及减重指标
Table 6 Comparing ASCVD risk and weight loss indicators after 3 months of treatment based on BMI stratification
| 指标 | 治疗前 | 治疗3个月 | 组间评估平均差异(95%CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 28.0 kg/m2<BMI<32.5 kg/m2组(n=105) | BMI≥32.5 kg/m2组(n=67) | Z(χ2)值 | P值 | 28.0 kg/m2<BMI<32.5 kg/m2组(n=105) | BMI ≥32.5 kg/m2组(n=67) | Z(χ2)值 | P值 | ||
| ASCVD风险(低危/中高危) | 73/32 | 41/26 | 1.270b | 0.260 | 97/8a | 52/15a | 7.702b | 0.006 | |
| TWL[M(P25,P75),%] | 8.4(4.8,12.9) | 9.9(5.8,13.9) | -1.217 | 0.224 | |||||
| TWL≥5%[例(%)] | 78.0(74.3) | 55.0(82.1) | 1.421b | 0.233 | |||||
| TWL≥10%[例(%)] | 44.0(38.1) | 34.0(50.7) | 1.290b | 0.256 | |||||
| 体质量[M(P25,P75),kg] | 84.9(78.7,91.4) | 101.9(91.0,113.2) | -7.842 | <0.001 | 77.6(70.2,85.5)a | 89.3(82.3,98.6)a | -5.726 | <0.001 | -4.555(-9.334~0.223) |
| BMI[M(P25,P75),kg/m2] | 30.4(29.5,31.4) | 34.4(33.4,36.5) | -11.047 | <0.001 | 27.8(26.4,29.0)a | 30.8(29.2,33.1)a | -6.989 | <0.001 | -1.179(-2.327~-0.031) |
| 腰围[M(P25,P75),cm] | 99.1(93.2,105.3) | 106.2(99.4,112.2) | -3.989 | <0.001 | 91.2(85.9,97.2)a | 95.8(89.7,106.3)a | -3.890 | <0.001 | 1.298(-3.123~5.721) |
| 腰高比[M(P25,P75)] | 0.6(0.6,0.6) | 0.6(0.6,0.7) | -3.515 | <0.001 | 0.5(0.5,0.6)a | 0.6(0.5,0.6)a | -2.916 | 0.004 | 0.008(-0.016~0.033) |
| 体脂肪[M(P25,P75),kg] | 31.2(28.1,34.3) | 40.5(35.8,46.9) | -8.308 | <0.001 | 26.4(21.1,29.2)a | 32.3(26.8,38.5)a | -5.351 | <0.001 | -3.232(-6.142~-0.323) |
| 体脂百分比[M(P25,P75),%] | 37.1(33.2,41.2) | 40.8(35.7,45.3) | -3.751 | <0.001 | 33.8(28.0,37.9)a | 35.7(30.3,42.5)a | -2.629 | <0.001 | -1.240(-3.951~1.470) |
| FMI[M(P25,P75),kg/m2] | 11.2(9.4,12.4) | 13.9(12.2,15.8) | -7.164 | <0.001 | 9.3(7.4,10.8)a | 10.9(8.8,13.7)a | -4.570 | <0.001 | -0.951(-1.980~0.078) |
| VFA[M(P25,P75),cm2] | 149.8(125.8,174.1) | 186.8(167.4,29.8) | -6.550 | 0.001 | 120.5(90.5,146.4)a | 151.1(112.3,175.6)a | -4.197 | <0.001 | -9.499(-24.690~5.691) |
| ASMI[M(P25,P75),kg/m2] | 7.8(7.2,8.4) | 8.9(8.0,9.4) | -5.830 | <0.001 | 7.6(6.9,8.3) | 8.3(7.6,9.1)a | -3.892 | 0.012 | -0.232(-0.763~0.298) |
| 总肌肉量[M(P25,P75),kg] | 48.9(44.1,57.8) | 56.8(49.2,65.0) | -4.255 | <0.001 | 47.7(42.9,56.8) | 54.5(46.4,61.3) | -3.012 | 0.010 | -2.321(-6.341~1.698) |
| 指标 | 治疗前 | 治疗3个月 | 组间评估平均差异(95%CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 男性组(n=73) | 女性组(n=99) | 检验统计量值 | P值 | 男性组(n=73) | 女性组(n=99) | 检验统计量值 | P值 | ||
| ASCVD风险(低危/中高危) | 43/30 | 71/28 | 3.086c | 0.079 | 63/10a | 87/11a | 0.238c | 0.626 | |
| TWL[M(P25,P75),%] | 8.1(2.9,13.0) | 9.8(5.9,13.7) | -1.190 | 0.234 | |||||
| TWL≥5%[例(%)] | 52.0(71.2) | 81.0(81.8) | 2.685c | 0.101 | |||||
| TWL≥10%[例(%)] | 31.0(42.4) | 47.0(47.5) | 0.425c | 0.514 | |||||
| 体质量[M(P25,P75),kg] | 98.4(87.8,109.2) | 83.8(79.5,92.5) | -5.126 | <0.001 | 87.2(82.2,97.3)a | 75.1(68.6,83.1)a | -6.190 | <0.001 | -1.495(-4.956~1.964) |
| BMI[M(P25,P75),kg/m2] | 31.6(30.2,34.1) | 31.5(30.0,33.9) | -0.469 | <0.001 | 29.1(27.2,30.9)a | 28.5(26.4,30.2)a | -0.970 | 0.821 | -0.227(-1.089~0.633) |
| 腰围( | 106.7±10.5 | 99.3±11.0 | 4.377b | <0.001 | 98.2±10.3a | 91.6±7.8a | 4.762b | <0.001 | 0.748(-2.643~4.139) |
| 腰高比[M(P25,P75)] | 0.6(0.6,0.6) | 0.6(0.6,0.6) | -1.070 | 0.284 | 0.6(0.5,0.6)a | 0.6(0.5,0.6)a | -0.685 | 0.494 | 0.001(-0.018~0.021) |
| 体脂肪[M(P25,P75),kg] | 33.2(27.4,39.6) | 34.7(30.7,39.6) | -0.837 | 0.403 | 25.5(21.1,32.2)a | 28.4(23.7,32.0)a | -2.004 | 0.045 | 1.471(-1.117~4.061) |
| 体脂百分比( | 35.2±4.9 | 41.4±6.3 | -7.084b | <0.001 | 29.4±5.8a | 37.4±5.8a | -8.956b | <0.001 | 1.735(-0.551~4.022) |
| FMI[M(P25,P75),kg/m2] | 10.9(9.5,12.8) | 12.7(11.7,14.7) | -4.077 | <0.001 | 8.3(7.2,10.2)a | 10.5(9.0,11.8)a | -4.799 | <0.001 | 0.475(-0.456~1.406) |
| VFA( | 156.3±38.4 | 171.8±41.6 | -2.444b | 0.016 | 117.3±39.7a | 140.3±42.2a | -3.744b | <0.001 | 8.754(-3.931~21.440) |
| ASMI[M(P25,P75),kg/m2] | 8.9(8.3,9.4) | 7.7(7.2,8.2) | -6.585 | <0.001 | 8.7(8.2,9.1) | 7.3(6.8,7.7)a | -9.212 | <0.001 | -0.436(-0.871~-0.001) |
| 总肌肉量[M(P25,P75),kg] | 60.8(53.8,66.4) | 46.7(42.9,50.8) | -7.920 | <0.001 | 58.8(55.3,63.2) | 43.8(40.9,48.1)a | -9.813 | <0.001 | -2.407(-5.388~0.573) |
表7 以性别分层比较治疗3个月后ASCVD风险及减重指标
Table 7 Comparing ASCVD risk and weight loss indicators after 3 months of treatment based on gender stratification
| 指标 | 治疗前 | 治疗3个月 | 组间评估平均差异(95%CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 男性组(n=73) | 女性组(n=99) | 检验统计量值 | P值 | 男性组(n=73) | 女性组(n=99) | 检验统计量值 | P值 | ||
| ASCVD风险(低危/中高危) | 43/30 | 71/28 | 3.086c | 0.079 | 63/10a | 87/11a | 0.238c | 0.626 | |
| TWL[M(P25,P75),%] | 8.1(2.9,13.0) | 9.8(5.9,13.7) | -1.190 | 0.234 | |||||
| TWL≥5%[例(%)] | 52.0(71.2) | 81.0(81.8) | 2.685c | 0.101 | |||||
| TWL≥10%[例(%)] | 31.0(42.4) | 47.0(47.5) | 0.425c | 0.514 | |||||
| 体质量[M(P25,P75),kg] | 98.4(87.8,109.2) | 83.8(79.5,92.5) | -5.126 | <0.001 | 87.2(82.2,97.3)a | 75.1(68.6,83.1)a | -6.190 | <0.001 | -1.495(-4.956~1.964) |
| BMI[M(P25,P75),kg/m2] | 31.6(30.2,34.1) | 31.5(30.0,33.9) | -0.469 | <0.001 | 29.1(27.2,30.9)a | 28.5(26.4,30.2)a | -0.970 | 0.821 | -0.227(-1.089~0.633) |
| 腰围( | 106.7±10.5 | 99.3±11.0 | 4.377b | <0.001 | 98.2±10.3a | 91.6±7.8a | 4.762b | <0.001 | 0.748(-2.643~4.139) |
| 腰高比[M(P25,P75)] | 0.6(0.6,0.6) | 0.6(0.6,0.6) | -1.070 | 0.284 | 0.6(0.5,0.6)a | 0.6(0.5,0.6)a | -0.685 | 0.494 | 0.001(-0.018~0.021) |
| 体脂肪[M(P25,P75),kg] | 33.2(27.4,39.6) | 34.7(30.7,39.6) | -0.837 | 0.403 | 25.5(21.1,32.2)a | 28.4(23.7,32.0)a | -2.004 | 0.045 | 1.471(-1.117~4.061) |
| 体脂百分比( | 35.2±4.9 | 41.4±6.3 | -7.084b | <0.001 | 29.4±5.8a | 37.4±5.8a | -8.956b | <0.001 | 1.735(-0.551~4.022) |
| FMI[M(P25,P75),kg/m2] | 10.9(9.5,12.8) | 12.7(11.7,14.7) | -4.077 | <0.001 | 8.3(7.2,10.2)a | 10.5(9.0,11.8)a | -4.799 | <0.001 | 0.475(-0.456~1.406) |
| VFA( | 156.3±38.4 | 171.8±41.6 | -2.444b | 0.016 | 117.3±39.7a | 140.3±42.2a | -3.744b | <0.001 | 8.754(-3.931~21.440) |
| ASMI[M(P25,P75),kg/m2] | 8.9(8.3,9.4) | 7.7(7.2,8.2) | -6.585 | <0.001 | 8.7(8.2,9.1) | 7.3(6.8,7.7)a | -9.212 | <0.001 | -0.436(-0.871~-0.001) |
| 总肌肉量[M(P25,P75),kg] | 60.8(53.8,66.4) | 46.7(42.9,50.8) | -7.920 | <0.001 | 58.8(55.3,63.2) | 43.8(40.9,48.1)a | -9.813 | <0.001 | -2.407(-5.388~0.573) |
| 指标 | 治疗前 | 治疗3个月 | 组间评估平均差异(95%CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 18~30岁组(n=58) | ≥30岁组(n=114) | 检验统计量值 | P值 | 18~30岁组(n=58) | ≥30岁组(n=114) | 检验统计量值 | P值 | ||
| ASCVD风险(低危/中高危) | 41/17 | 73/41 | 0.515c | 0.473 | 48/10 | 102/12a | 2.223c | 0.136 | |
| TWL[M(P25,P75),%] | 9.5(5.7,14.3) | 8.7(5.5,13.3) | -0.397 | 0.692 | |||||
| TWL≥5%[例(%)] | 46.0(79.3) | 87.0(76.3) | 0.197c | 0.657 | |||||
| TWL≥10%[例(%)] | 26.0(44.8) | 52.0(45.6) | 0.010c | 0.922 | |||||
| 体质量( | 97.3±13.1 | 89.6±13.6 | 3.562b | <0.001 | 87.7±13.2a | 80.8±12.6a | 3.328b | 0.176 | 0.841(-2.781~4.464) |
| BMI[M(P25,P75),kg/m2] | 32.9(30.7,35.1) | 31(29.9,33.4) | -3.487 | <0.001 | 29.0(26.5,31.1)a | 28.6(26.9,30.4)a | -2.558 | 0.535 | 0.344(-0.555~1.244) |
| 腰围[M(P25,P75),cm] | 103.8(97.1,109.8) | 100.4(94.5,106.1) | -2.624 | 0.003 | 94.4(89.1,102.3)a | 93.1(86.4,100.5)a | -2.749 | 0.103 | 1.167(-2.376~4.710) |
| 腰高比[M(P25,P75)] | 0.6(0.6,0.6) | 0.6(0.6,0.6) | -1.560 | 0.119 | 0.6(0.5,0.6)a | 0.6(0.5,0.6)a | -1.581 | 0.114 | 0.006(-0.014~0.027) |
| 体脂肪[M(P25,P75),kg] | 37.7(29.8,43.5) | 33.7(30.5,38.2) | -3.249 | 0.001 | 29.0(22.3,33.7)a | 26.5(21.6,31.8)a | -3.011 | 0.119 | 1.120(-1.592~3.832) |
| 体脂百分比( | 39.4±6.8 | 38.3±6.3 | 1.079b | 0.226 | 35.3±7.5a | 33.4±6.7a | 1.679b | 0.170 | -0.233(-2.640~2.172) |
| FMI[M(P25,P75),kg/m2] | 12.4(10.4,15.5) | 12.1(10.8,13.2) | -1.943 | 0.052 | 10.1(8.2,12.6)a | 9.7(7.8,10.9)a | -1.598 | 0.099 | 0.434(-0.539~1.409) |
| VFA( | 175.8±43.2 | 159.5±38.3 | 2.493b | 0.014 | 142.9±45.3a | 124.9±40.3a | 2.643b | 0.136 | -0.062(-13.397~13.272) |
| ASMI( | 8.2±1.8 | 7.8±1.7 | 1.193b | 0.024 | 7.8±1.8 | 7.8±0.9 | 0.056b | 0.434 | 0.321(-0.134~0.778) |
| 总肌肉量[M(P25,P75),kg] | 54.5(48.9,63.3) | 49.6(44.6,60.9) | -2.320 | 0.020 | 48.7(44.2,61.5) | 50.8(42.3,57.4) | -1.940 | 0.449 | 1.164(-1.970~4.299) |
表8 以年龄分层比较治疗3个月后ASCVD风险及减重指标
Table 8 Comparing ASCVD risk and weight loss indicators after 3 months of treatment based on age stratification
| 指标 | 治疗前 | 治疗3个月 | 组间评估平均差异(95%CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 18~30岁组(n=58) | ≥30岁组(n=114) | 检验统计量值 | P值 | 18~30岁组(n=58) | ≥30岁组(n=114) | 检验统计量值 | P值 | ||
| ASCVD风险(低危/中高危) | 41/17 | 73/41 | 0.515c | 0.473 | 48/10 | 102/12a | 2.223c | 0.136 | |
| TWL[M(P25,P75),%] | 9.5(5.7,14.3) | 8.7(5.5,13.3) | -0.397 | 0.692 | |||||
| TWL≥5%[例(%)] | 46.0(79.3) | 87.0(76.3) | 0.197c | 0.657 | |||||
| TWL≥10%[例(%)] | 26.0(44.8) | 52.0(45.6) | 0.010c | 0.922 | |||||
| 体质量( | 97.3±13.1 | 89.6±13.6 | 3.562b | <0.001 | 87.7±13.2a | 80.8±12.6a | 3.328b | 0.176 | 0.841(-2.781~4.464) |
| BMI[M(P25,P75),kg/m2] | 32.9(30.7,35.1) | 31(29.9,33.4) | -3.487 | <0.001 | 29.0(26.5,31.1)a | 28.6(26.9,30.4)a | -2.558 | 0.535 | 0.344(-0.555~1.244) |
| 腰围[M(P25,P75),cm] | 103.8(97.1,109.8) | 100.4(94.5,106.1) | -2.624 | 0.003 | 94.4(89.1,102.3)a | 93.1(86.4,100.5)a | -2.749 | 0.103 | 1.167(-2.376~4.710) |
| 腰高比[M(P25,P75)] | 0.6(0.6,0.6) | 0.6(0.6,0.6) | -1.560 | 0.119 | 0.6(0.5,0.6)a | 0.6(0.5,0.6)a | -1.581 | 0.114 | 0.006(-0.014~0.027) |
| 体脂肪[M(P25,P75),kg] | 37.7(29.8,43.5) | 33.7(30.5,38.2) | -3.249 | 0.001 | 29.0(22.3,33.7)a | 26.5(21.6,31.8)a | -3.011 | 0.119 | 1.120(-1.592~3.832) |
| 体脂百分比( | 39.4±6.8 | 38.3±6.3 | 1.079b | 0.226 | 35.3±7.5a | 33.4±6.7a | 1.679b | 0.170 | -0.233(-2.640~2.172) |
| FMI[M(P25,P75),kg/m2] | 12.4(10.4,15.5) | 12.1(10.8,13.2) | -1.943 | 0.052 | 10.1(8.2,12.6)a | 9.7(7.8,10.9)a | -1.598 | 0.099 | 0.434(-0.539~1.409) |
| VFA( | 175.8±43.2 | 159.5±38.3 | 2.493b | 0.014 | 142.9±45.3a | 124.9±40.3a | 2.643b | 0.136 | -0.062(-13.397~13.272) |
| ASMI( | 8.2±1.8 | 7.8±1.7 | 1.193b | 0.024 | 7.8±1.8 | 7.8±0.9 | 0.056b | 0.434 | 0.321(-0.134~0.778) |
| 总肌肉量[M(P25,P75),kg] | 54.5(48.9,63.3) | 49.6(44.6,60.9) | -2.320 | 0.020 | 48.7(44.2,61.5) | 50.8(42.3,57.4) | -1.940 | 0.449 | 1.164(-1.970~4.299) |
| [1] |
World Obesity Federation. World Obesity Atlas 2024[EB/OL]. [2025-02-20].
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
曲伸,陆灏,宋勇峰. 基于临床的肥胖症多学科诊疗共识(2021年版)[J]. 中华肥胖与代谢病电子杂志,2021,7(4):211-226.
|
| [6] |
|
| [7] |
|
| [8] |
中国血脂管理指南修订联合专家委员会,王增武,李建军,等. 中国血脂管理指南(基层版2024年)[J]. 中国全科医学,2024,27(20):2429-2436. DOI: 10.12114/j.issn.1007-9572.2024.0005.
|
| [9] |
陆菊明. 《中国2型糖尿病防治指南(2020年版)》读后感[J]. 中华糖尿病杂志,2021,13(4):301-304. DOI:10.3760/cma.j.cn115791-20210307-00135.
|
| [10] |
中华医学会,中华医学杂志社,中华医学会全科医学分会,等. 高血压基层诊疗指南(2019年)[J]. 中华全科医师杂志,2019,18(4):301-313. DOI:10.3760/cma.j.issn.1671-7368.2019.04.002.
|
| [11] |
范建高,徐小元,南月敏,等. 代谢相关(非酒精性)脂肪性肝病防治指南(2024年版)[J]. 实用肝脏病杂志,2024,27(4):494-510.
|
| [12] |
《混合型高脂血症基层诊疗中国专家共识(年)》编写专家组. 混合型高脂血症基层诊疗中国专家共识(2024年)[J]. 中华全科医师杂志,2024,23(9):907-917. DOI:10.3760/cma.j.cn114798-20240523-00476.
|
| [13] |
中华医学会内分泌学分会. 中国高尿酸血症与痛风诊疗指南(2019)[J]. 中华内分泌代谢杂志,2020,36(1):1-13. DOI:10.3760/cma.j.issn.1000-6699.2020.01.001.
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
中华医学会内分泌学分会. 肥胖患者的长期体质量管理及药物临床应用指南(2024版)[J]. 中华内分泌代谢杂志,2024,40(7):545-564. DOI:10.3760/cma.j.cn311282-20240412-00149.
|
| [18] |
|
| [19] |
中华医学会心血管病学分会高血压学组,中华心血管病杂志编辑委员会. 中国高血压患者血压血脂综合管理的专家共识[J]. 中华心血管病杂志,2021,49(6):554-563. DOI:10.3760/cma.j.cn112148-20210202-00128.
|
| [20] |
|
| [21] |
|
| [22] |
|
| [23] |
|
| [1] | 周晟, 邓长生, 邹冠炀, 宋健平. 疟疾心血管疾病并发症发病机制的研究进展[J]. 中国全科医学, 2025, 28(27): 3466-3472. |
| [2] | 韩笑, 李奇遇, 葛蒲, 范思园, 刘迪玥, 吴一波, 张清霜. 高血压患者行为生活方式对生命质量的影响研究[J]. 中国全科医学, 2025, 28(26): 3248-3258. |
| [3] | 刘银银, 隋鸿平, 李婷婷, 姜桐桐, 史铁英, 夏云龙. 乳腺癌治疗相关心脏毒性风险预测模型的研究进展[J]. 中国全科医学, 2025, 28(24): 3072-3078. |
| [4] | 魏云鸿, 杨莉, 王玉路, 叶秋芳, 代安妮, 何燕. 肥胖相关性高血压患者不同运动阶段心肺功能的研究[J]. 中国全科医学, 2025, 28(24): 2972-2978. |
| [5] | 石小天, 王珊, 杨华昱, 杨一帆, 李旭, 马清. 中国老年人体重指数和死亡的相关性:一项队列研究[J]. 中国全科医学, 2025, 28(22): 2791-2797. |
| [6] | 王爽, 吴树法, 令垚, 谭茜蔚, 曹汝岱, 曾慧婷, 孔丹莉, 丁元林, 于海兵. 基于代谢组学探究非脂质代谢物在肥胖与糖尿病视网膜病变间的中介作用:孟德尔随机化研究[J]. 中国全科医学, 2025, 28(21): 2625-2634. |
| [7] | 高海钧, 任佳禹, 王若琳, 周慧亚, 曲鹏. 内皮细胞损伤及其功能障碍在动脉粥样硬化中作用的研究进展[J]. 中国全科医学, 2025, 28(21): 2697-2704. |
| [8] | 金彦, 杨洋, 王璐璐, 郑清婉, 李新艳, 张宁. 减重代谢手术后运动训练对2型糖尿病合并肥胖患者心肺功能的影响:一项随机对照试验[J]. 中国全科医学, 2025, 28(21): 2611-2617. |
| [9] | 李春贤, 刘安诺. 成年人肥胖和脂质相关指标对代谢综合征的影响及预测价值研究[J]. 中国全科医学, 2025, 28(21): 2595-2603. |
| [10] | 褚田雨, 顾艳. 颈动脉钙化特征在评估斑块稳定性及临床事件中的作用[J]. 中国全科医学, 2025, 28(18): 2247-2252. |
| [11] | 潘姚佳, 傅方琳, 韩正, 孙梦, 顾怀聪, 王为强. 肥胖类型与心血管代谢性共病的关系:基于不同性别的中年居民[J]. 中国全科医学, 2025, 28(18): 2285-2293. |
| [12] | 吕露露, 祝万洁, 肖明洋, 李祎珂, 张娟. 原发性高血压患者血压昼夜节律与血浆氧化的低密度脂蛋白/β2-糖蛋白I复合物及颈动脉粥样硬化的相关性研究[J]. 中国全科医学, 2025, 28(18): 2228-2233. |
| [13] | 韩正, 孙梦, 傅方琳, 潘姚佳, 王为强. 50岁及以上人群三酰甘油葡萄糖指数与心血管代谢性共病关系的研究[J]. 中国全科医学, 2025, 28(18): 2278-2284. |
| [14] | 张冰清, 王忠凯, 吴长勇, 孙煌, 李锐洁, 刘文洁, 骆怡哗, 郑丽慧, 彭云珠. 1990—2021年全球先天性心脏缺陷疾病负担变化及未来趋势预测研究[J]. 中国全科医学, 2025, 28(18): 2253-2261. |
| [15] | 安芹彧, 王艺颖, 张小丹, 张畑霖, 詹清清, 张福艳, 刘涛, 吴延莉. 社会经济地位、健康生活方式对心血管疾病影响的前瞻性队列研究[J]. 中国全科医学, 2025, 28(16): 2017-2024. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





