中国全科医学 ›› 2026, Vol. 29 ›› Issue (08): 997-1007.DOI: 10.12114/j.issn.1007-9572.2025.0364
• 论著 • 上一篇
曹磊1, 刘学春2, 江伟1, 陈炎1, 严孙宏1, 杜静1,*( )
)
收稿日期:2025-10-10
修回日期:2025-11-30
出版日期:2026-03-15
发布日期:2026-02-03
通讯作者:
杜静
作者贡献:
曹磊提出研究思路,设计研究方案,负责论文写作和英文修订;刘学春、江伟负责调查对象的选取、现场问卷调查、数据录入和核对、统计学处理等;陈炎、严孙宏负责影像资料的质控;杜静负责文章质量控制、审查、修订和监督管理,对论文整体负责。
基金资助:
CAO Lei1, LIU Xuechun2, JIANG Wei1, CHEN Yan1, YAN Sunhong1, DU Jing1,*( )
)
Received:2025-10-10
Revised:2025-11-30
Published:2026-03-15
Online:2026-02-03
Contact:
DU Jing
摘要: 背景 急性缺血性脑卒中(AIS)患者合并肌肉衰减状态与临床不良预后显著相关,因此,发掘简便易行且可操作性强的临床指标辅助筛查高危人群,已成为当前卒中康复与临床营养领域的交叉研究热点。 目的 探讨颞肌横截面积(TMA)和颞肌厚度(TMT)评估AIS患者肌肉衰减状态的可行性及临床价值。 方法 纳入2022年1月—2025年8月安徽医科大学第二附属医院收治的531例AIS患者(男347例,女184例),通过颅脑CT或MRI测量双侧TMA和TMT,并根据亚洲肌肉衰减症工作组(AWGS 2019)标准诊断肌肉衰减症。采用单因素及多因素Logistic回归分析筛选独立预测因素,构建预测模型并通过受试者工作特征曲线(ROC曲线)、校准曲线及临床决策曲线分析评估其效能。 结果 AIS患者肌肉衰减症患病率为19.96%(106/531),根据诊断标准将患者分为肌肉衰减组(n=106)与无肌肉衰减组(n=425)。肌肉衰减组患者TMA、TMT均低于无肌肉衰减组(P<0.001)。多因素Logistic回归分析结果显示,年龄(OR=1.717,95%CI=1.223~2.410)、美国国立卫生研究院卒中量表(NIHSS)评分(OR=3.213,95%CI=1.829~5.643)、营养风险筛查量表(NRS 2002)评分(OR=1.337,95%CI=1.045~1.711)及TMA(OR=0.781,95%CI=0.639~0.955)为AIS出现肌肉衰减症的独立影响因素(P<0.05)。为构建并验证肌肉衰减症风险预测模型,将所有研究对象按3∶1的比例随机分为训练集(n=398)与验证集(n=133)。基于多因素Logistic回归分析构建的最终模型公式为:Logit(P)=46.221 22+0.082 11×年龄+2.078 56×(NRS 2002=1)-0.144 80×TMA+18.327 80×(NIHSS=1),并生成预测肌肉衰减症风险的列线图。预测模型在训练集中的ROC曲线下面积(AUC)为0.884(95%CI=0.782~0.947),在验证集中的AUC为0.808(95%CI=0.679~0.882)。校准曲线显示模型预测概率与实际概率一致性良好,临床决策曲线表明模型在广泛阈值概率范围内具有临床净获益。 结论 颞肌测量是评估AIS患者肌肉衰减状态的有效方法,基于年龄、NIHSS评分、NRS 2002评分和TMA构建的预测模型具有良好的判别效能与临床适用性,可作为AIS患者肌肉衰减症的早期识别的实用工具。
中图分类号:
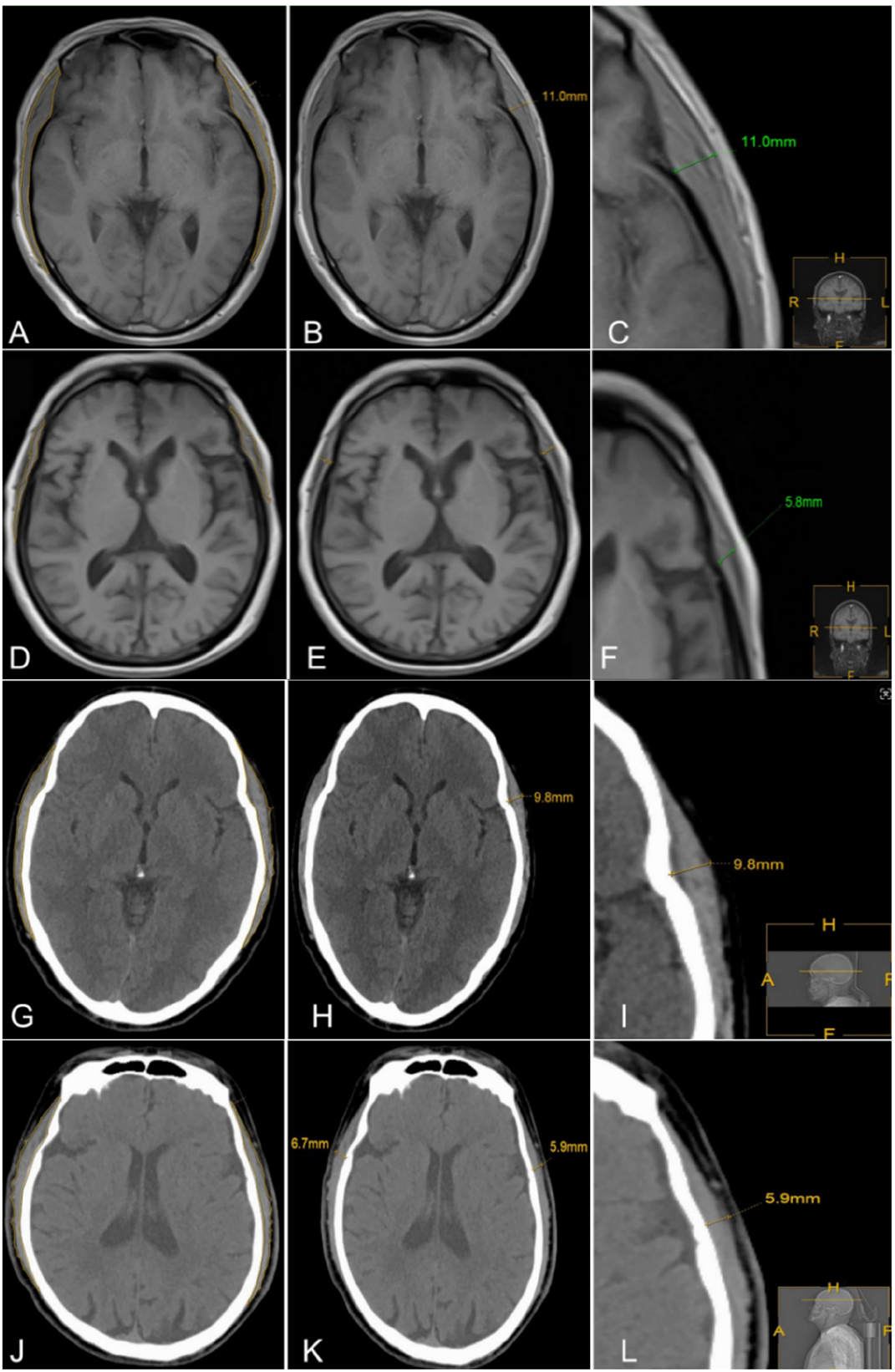
图1 颞肌横截面积和厚度的MRI、CT检查示意图注:A、B、C分别为无肌肉衰减症患者MRI T1加权成像(T1WI)影像的颞肌面积勾画示意图、左侧颞肌厚度及左侧颞肌厚度放大图;D、E、F分别为存在肌肉衰减症患者MRI T1WI影像的颞肌面积勾画示意图、左侧颞肌厚度及左侧颞肌厚度放大图;G、H、I分别为无肌肉衰减症患者CT影像的颞肌面积勾画示意图、左侧颞肌厚度及左侧颞肌厚度放大图;J、K、L分别为存在肌肉衰减症患者CT影像的颞肌面积勾画示意图、左侧颞肌厚度及左侧颞肌厚度放大图。
Figure 1 Sketch diagram of cross-sectional area and thickness of temporal muscle in patients with different muscle states
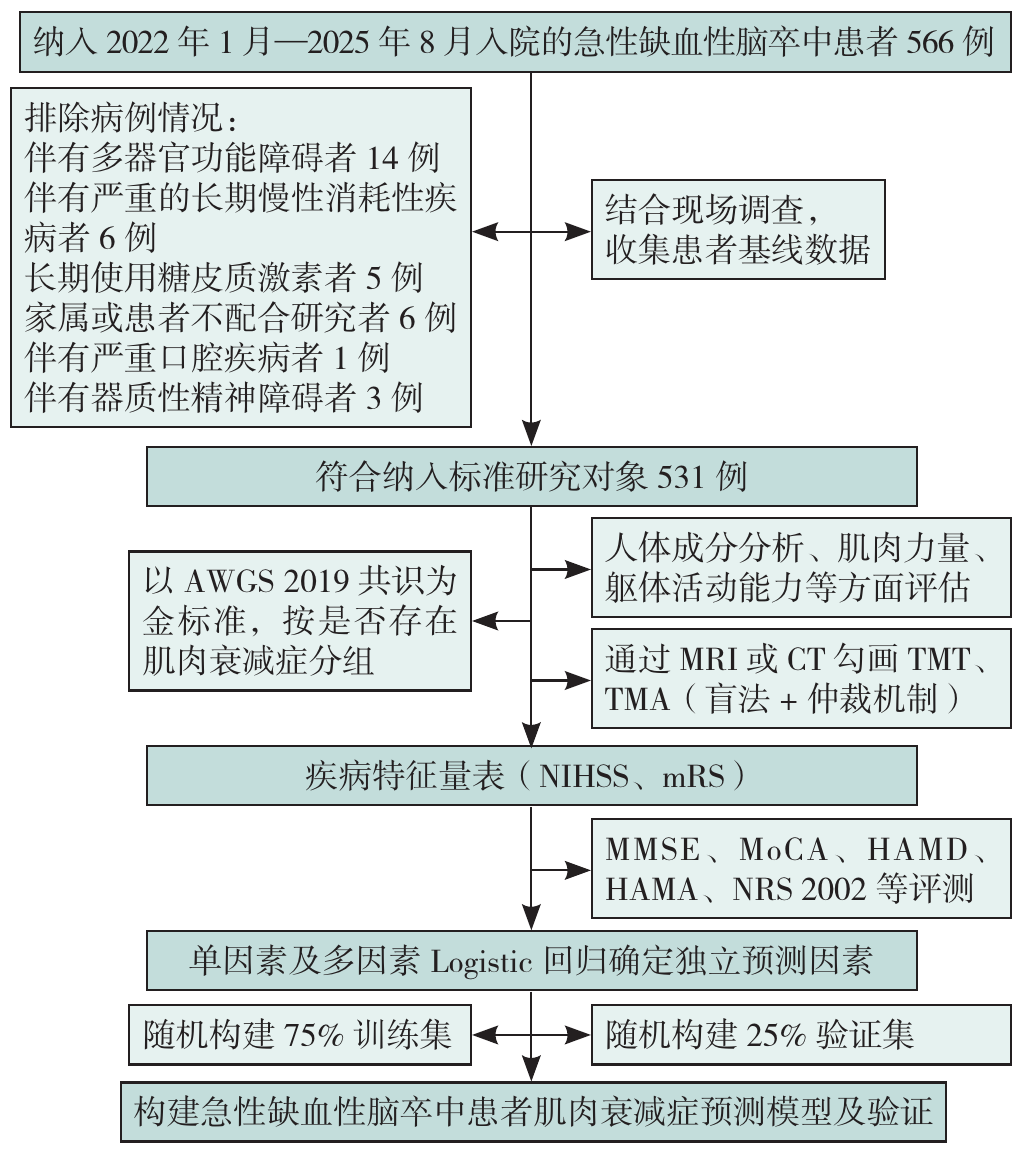
图2 研究流程图注:AWGS=亚洲肌肉减少症工作组,TMA=颞肌横截面积,TMT=颞肌厚度,NIHSS=美国国立卫生研究院卒中量表,mRS=改良RANKIN量表,NRS 2002=营养风险筛查量表,MMSE=简易精神状态检查量表,MoCA=蒙特利尔认知评估量表,HAMA=汉密尔顿焦虑量表,HAMD=汉密尔顿抑郁量表。
Figure 2 Research flow chart
| 组别 | 例数 | 性别[例(%)] | 糖尿病[例(%)] | NRS 2002评分[例(%)] | mRS评分[例(%)] | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | 否 | 是 | <3分 | ≥3分 | ≤2分 | >2分 | ||||
| 无肌肉衰减组 | 425 | 133(31.3) | 292(68.7) | 377(88.7) | 48(11.3) | 176(41.4) | 249(58.6) | 290(68.2) | 135(31.8) | ||
| 肌肉衰减组 | 106 | 33(31.1) | 73(68.9) | 101(95.3) | 5(4.7) | 0 | 106(100.0) | 16(15.1) | 90(84.9) | ||
| χ2(t)值 | 0.01 | 4.08 | 268.12 | 98.11 | |||||||
| P值 | 0.974 | 0.043 | <0.001 | <0.001 | |||||||
| 组别 | 婚姻状况[例(%)] | 吸烟状况[例(%)] | 饮酒状况[例(%)] | 高脂血症[例(%)] | 高血压[例(%)] | ||||||
| 未婚 | 已婚 | 离婚或丧偶 | 从不吸烟 | 现在吸烟 | 现在饮酒 | 现在不饮 | 否 | 是 | 否 | 是 | |
| 无肌肉衰减组 | 4(1.0) | 355(83.5) | 66(15.5) | 275(64.7) | 150(35.3) | 298(70.1) | 127(29.9) | 353(83.1) | 72(16.9) | 230(54.1) | 195(45.9) |
| 肌肉衰减组 | 1(1.0) | 79(74.5) | 26(24.5) | 65(61.3) | 41(38.7) | 75(70.8) | 31(29.2) | 99(93.4) | 7(6.6) | 67(63.2) | 39(36.8) |
| χ2(t)值 | 5.10 | 0.42 | 0.01 | 7.15 | 0.01 | ||||||
| P值 | 0.090 | 0.516 | 0.898 | 0.007 | 0.974 | ||||||
| 组别 | 卒中类型[例(%)] | 年龄( | 血清白蛋白( | TMT( | TMA( | MMSE评分( | |||||
| 大动脉粥样硬化型 | 小动脉闭塞型 | 心源性梗死型 | 其他类型 | ||||||||
| 无肌肉衰减组 | 290(68.2) | 71(16.7) | 36(8.5) | 28(6.6) | 59.5±11.2 | 40.62±3.11 | 4.62±0.53 | 525.22±27.85 | 26.25±2.79 | ||
| 肌肉衰减组 | 58(54.7) | 20(18.9) | 8(7.5) | 20(18.9) | 68.2±8.3 | 37.73±3.17 | 3.11±0.47 | 463.41±35.23 | 21.32±5.31 | ||
| χ2(t)值 | 16.83 | -9.10a | 8.52a | 16.79a | 33.43a | 9.29a | |||||
| P值 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| 组别 | MoCA评分( | HAMA评分( | HAMD评分( | BMI( | 肌肉质量( | 骨骼肌质量( | 体脂质量( | NIHSS评分[例(%)] | 全身相位角( | ||
| ≤5分 | >5分 | ||||||||||
| 无肌肉衰减组 | 24.91±3.25 | 10.12±2.11 | 4.12±2.31 | 26.8±2.0 | 46.13±8.41 | 45.01±8.27 | 16.16±6.63 | 356(83.8) | 69(16.2) | 7.10°±1.03° | |
| 肌肉衰减组 | 19.26±6.28 | 13.25±3.66 | 7.03±2.76 | 20.3±2.2 | 26.11±4.35 | 22.58±3.75 | 8.32±5.36 | 59(55.7) | 47(44.3) | 3.82°±1.11° | |
| χ2(t)值 | 9.27a | -8.46a | -10.33a | 27.77a | 34.03a | 41.93a | 12.97a | 64.13 | 30.43a | ||
| P值 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
表1 不同肌肉状态组患者的一般资料比较
Table 1 Comparison of general demographics between AIS patients with different muscle states
| 组别 | 例数 | 性别[例(%)] | 糖尿病[例(%)] | NRS 2002评分[例(%)] | mRS评分[例(%)] | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | 否 | 是 | <3分 | ≥3分 | ≤2分 | >2分 | ||||
| 无肌肉衰减组 | 425 | 133(31.3) | 292(68.7) | 377(88.7) | 48(11.3) | 176(41.4) | 249(58.6) | 290(68.2) | 135(31.8) | ||
| 肌肉衰减组 | 106 | 33(31.1) | 73(68.9) | 101(95.3) | 5(4.7) | 0 | 106(100.0) | 16(15.1) | 90(84.9) | ||
| χ2(t)值 | 0.01 | 4.08 | 268.12 | 98.11 | |||||||
| P值 | 0.974 | 0.043 | <0.001 | <0.001 | |||||||
| 组别 | 婚姻状况[例(%)] | 吸烟状况[例(%)] | 饮酒状况[例(%)] | 高脂血症[例(%)] | 高血压[例(%)] | ||||||
| 未婚 | 已婚 | 离婚或丧偶 | 从不吸烟 | 现在吸烟 | 现在饮酒 | 现在不饮 | 否 | 是 | 否 | 是 | |
| 无肌肉衰减组 | 4(1.0) | 355(83.5) | 66(15.5) | 275(64.7) | 150(35.3) | 298(70.1) | 127(29.9) | 353(83.1) | 72(16.9) | 230(54.1) | 195(45.9) |
| 肌肉衰减组 | 1(1.0) | 79(74.5) | 26(24.5) | 65(61.3) | 41(38.7) | 75(70.8) | 31(29.2) | 99(93.4) | 7(6.6) | 67(63.2) | 39(36.8) |
| χ2(t)值 | 5.10 | 0.42 | 0.01 | 7.15 | 0.01 | ||||||
| P值 | 0.090 | 0.516 | 0.898 | 0.007 | 0.974 | ||||||
| 组别 | 卒中类型[例(%)] | 年龄( | 血清白蛋白( | TMT( | TMA( | MMSE评分( | |||||
| 大动脉粥样硬化型 | 小动脉闭塞型 | 心源性梗死型 | 其他类型 | ||||||||
| 无肌肉衰减组 | 290(68.2) | 71(16.7) | 36(8.5) | 28(6.6) | 59.5±11.2 | 40.62±3.11 | 4.62±0.53 | 525.22±27.85 | 26.25±2.79 | ||
| 肌肉衰减组 | 58(54.7) | 20(18.9) | 8(7.5) | 20(18.9) | 68.2±8.3 | 37.73±3.17 | 3.11±0.47 | 463.41±35.23 | 21.32±5.31 | ||
| χ2(t)值 | 16.83 | -9.10a | 8.52a | 16.79a | 33.43a | 9.29a | |||||
| P值 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| 组别 | MoCA评分( | HAMA评分( | HAMD评分( | BMI( | 肌肉质量( | 骨骼肌质量( | 体脂质量( | NIHSS评分[例(%)] | 全身相位角( | ||
| ≤5分 | >5分 | ||||||||||
| 无肌肉衰减组 | 24.91±3.25 | 10.12±2.11 | 4.12±2.31 | 26.8±2.0 | 46.13±8.41 | 45.01±8.27 | 16.16±6.63 | 356(83.8) | 69(16.2) | 7.10°±1.03° | |
| 肌肉衰减组 | 19.26±6.28 | 13.25±3.66 | 7.03±2.76 | 20.3±2.2 | 26.11±4.35 | 22.58±3.75 | 8.32±5.36 | 59(55.7) | 47(44.3) | 3.82°±1.11° | |
| χ2(t)值 | 9.27a | -8.46a | -10.33a | 27.77a | 34.03a | 41.93a | 12.97a | 64.13 | 30.43a | ||
| P值 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
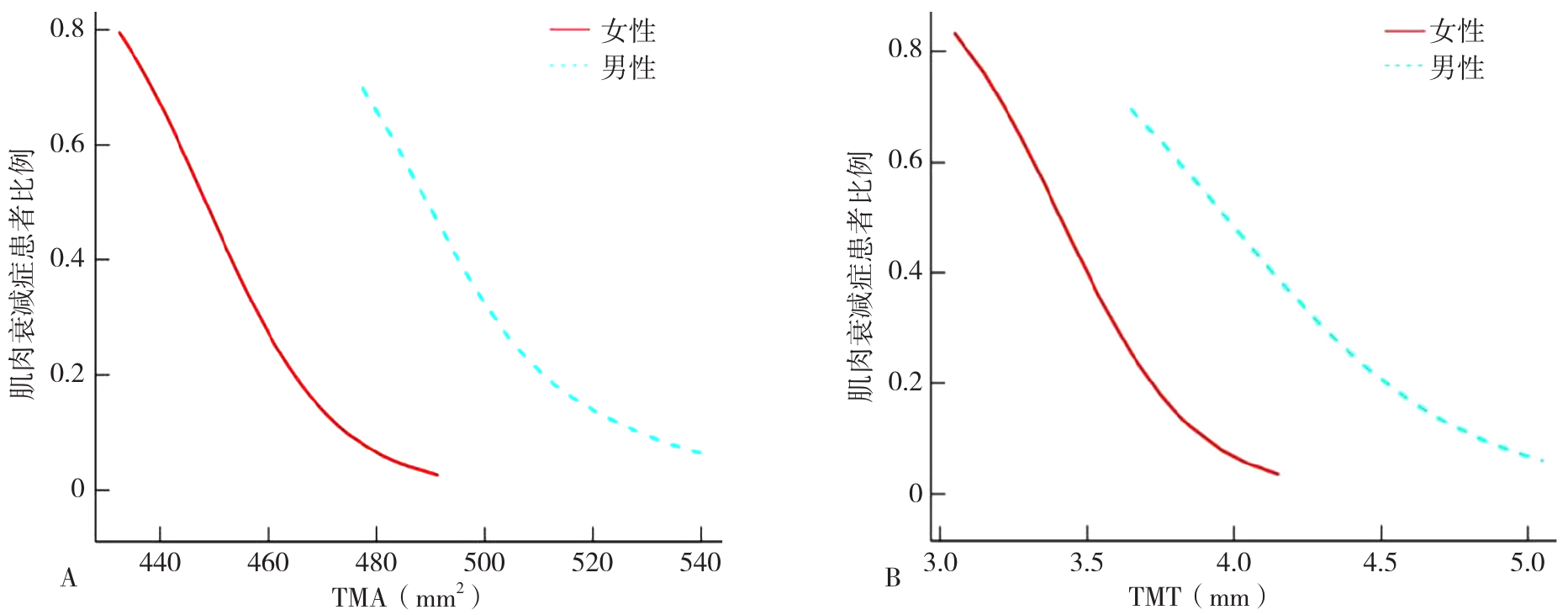
图3 不同性别急性缺血性脑卒中患者颞肌测量指标和肌肉衰减症的平滑曲线注:A为TMA指标,B为TMT指标。
Figure 3 The smooth curve of TMT and TMA and sarcopenia in patients with acute ischemic stroke of different genders
| 变量 | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| OR(95%CI) | P值 | OR(95%CI) | P值 | OR(95%CI) | P值 | |
| TMT(男性) | 0.06(<0.01~0.35) | 0.010 | 0.05(<0.01~0.70) | 0.027 | 0.05(<0.01~0.98) | 0.049 |
| TMA(男性) | 0.89(0.86~0.92) | <0.001 | 0.88(0.85~0.92) | <0.001 | 0.86(0.82~0.91) | <0.001 |
| TMT(女性) | <0.01(<0.01~0.02) | <0.001 | <0.01(<0.01~0.01) | <0.001 | 0.01(<0.01~0.01) | 0.002 |
| TMA(女性) | 0.89(0.84~0.94) | <0.001 | 0.89(0.84~0.94) | <0.001 | 0.86(0.79~0.95) | <0.001 |
表2 TMT/TMA与不同性别患者肌肉衰减症发生关系的多因素Logistic回归分析
Table 2 Multivariate Logistic regression analysis of the relationship between TMT/TMA and the occurrence of muscle atrophy syndrome in different sexes
| 变量 | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| OR(95%CI) | P值 | OR(95%CI) | P值 | OR(95%CI) | P值 | |
| TMT(男性) | 0.06(<0.01~0.35) | 0.010 | 0.05(<0.01~0.70) | 0.027 | 0.05(<0.01~0.98) | 0.049 |
| TMA(男性) | 0.89(0.86~0.92) | <0.001 | 0.88(0.85~0.92) | <0.001 | 0.86(0.82~0.91) | <0.001 |
| TMT(女性) | <0.01(<0.01~0.02) | <0.001 | <0.01(<0.01~0.01) | <0.001 | 0.01(<0.01~0.01) | 0.002 |
| TMA(女性) | 0.89(0.84~0.94) | <0.001 | 0.89(0.84~0.94) | <0.001 | 0.86(0.79~0.95) | <0.001 |
| 变量 | B | SE | Wald χ2值 | P值 | OR(95%CI) |
|---|---|---|---|---|---|
| 年龄 | 0.094 | 0.014 | 47.235 | <0.001 | 1.099(1.070~1.128) |
| NIHSS评分(以>5分为参照) | 1.413 | 0.236 | 35.979 | <0.001 | 4.110(2.590~6.523) |
| 卒中类型(以大动脉粥样硬化型为参照) | |||||
| 小动脉闭塞型 | -1.273 | 0.326 | 15.229 | 0.001 | 0.280(0.148~0.531) |
| 心源性梗死型 | -0.930 | 0.387 | 5.780 | 0.016 | 0.394(0.185~0.842) |
| 不明原因型 | -1.168 | 0.488 | 5.716 | 0.017 | 0.311(0.119~0.810) |
| 性别(以男性为参照) | -0.008 | 0.234 | 0.001 | 0.974 | 0.992(0.627~1.571) |
| 高血压(以无为参照) | 0.376 | 0.224 | 2.826 | 0.093 | 1.457(0.940~2.258) |
| 糖尿病(以无为参照) | 0.050 | 0.026 | 3.823 | 0.051 | 1.251(0.998~1.329) |
| 高脂血症(以无为参照) | 1.059 | 0.412 | 6.614 | 0.010 | 2.101(1.287~6.467) |
| 饮酒(以无为参照) | 0.031 | 0.238 | 0.016 | 0.898 | 1.031(0.646~1.645) |
| 吸烟(以无为参照) | -0.145 | 0.224 | 0.422 | 0.516 | 0.865(0.558~1.341) |
| 婚姻状况(以未婚为参照) | |||||
| 已婚 | -0.470 | 1.142 | 0.169 | 0.681 | 0.625(0.067~5.859) |
| 离婚或丧偶 | -0.589 | 0.263 | 5.008 | 0.025 | 0.555(0.331~0.929) |
| NRS 2002评分 | 1.645 | 0.264 | 38.731 | <0.001 | 5.182(1.287~20.864) |
| mRS评分 | -2.488 | 0.291 | 73.511 | <0.001 | 0.083(0.047~0.146) |
| MMSE评分 | -0.347 | 0.038 | 85.536 | <0.001 | 0.707(0.657~0.761) |
| HAMA评分 | 0.418 | 0.048 | 74.446 | <0.001 | 1.520(1.382~1.671) |
| 体脂质量 | -0.217 | 0.024 | 83.249 | <0.001 | 0.805(0.769~0.844) |
| 骨骼肌质量 | -0.846 | 0.134 | 39.746 | <0.001 | 0.429(0.330~0.558) |
| 肌肉质量 | -2.617 | 0.619 | 17.860 | <0.001 | 0.073(0.022~0.246) |
| 全身相位角 | -5.809 | 0.935 | 38.137 | <0.001 | 0.003(<0.001~0.019) |
| TMA | -0.115 | 0.015 | 60.834 | <0.001 | 0.891(0.865~0.917) |
| TMT | -1.339 | 0.220 | 37.183 | <0.001 | 0.262(0.160~0.430) |
| 血清白蛋白 | -0.288 | 0.040 | 51.720 | <0.001 | 0.750(0.694~0.811) |
表3 急性缺血性脑卒中患者肌肉衰减症影响因素的单因素Logistic回归分析
Table 3 Single logistic regression analysis of factors affecting muscle atrophy in patients with AIS
| 变量 | B | SE | Wald χ2值 | P值 | OR(95%CI) |
|---|---|---|---|---|---|
| 年龄 | 0.094 | 0.014 | 47.235 | <0.001 | 1.099(1.070~1.128) |
| NIHSS评分(以>5分为参照) | 1.413 | 0.236 | 35.979 | <0.001 | 4.110(2.590~6.523) |
| 卒中类型(以大动脉粥样硬化型为参照) | |||||
| 小动脉闭塞型 | -1.273 | 0.326 | 15.229 | 0.001 | 0.280(0.148~0.531) |
| 心源性梗死型 | -0.930 | 0.387 | 5.780 | 0.016 | 0.394(0.185~0.842) |
| 不明原因型 | -1.168 | 0.488 | 5.716 | 0.017 | 0.311(0.119~0.810) |
| 性别(以男性为参照) | -0.008 | 0.234 | 0.001 | 0.974 | 0.992(0.627~1.571) |
| 高血压(以无为参照) | 0.376 | 0.224 | 2.826 | 0.093 | 1.457(0.940~2.258) |
| 糖尿病(以无为参照) | 0.050 | 0.026 | 3.823 | 0.051 | 1.251(0.998~1.329) |
| 高脂血症(以无为参照) | 1.059 | 0.412 | 6.614 | 0.010 | 2.101(1.287~6.467) |
| 饮酒(以无为参照) | 0.031 | 0.238 | 0.016 | 0.898 | 1.031(0.646~1.645) |
| 吸烟(以无为参照) | -0.145 | 0.224 | 0.422 | 0.516 | 0.865(0.558~1.341) |
| 婚姻状况(以未婚为参照) | |||||
| 已婚 | -0.470 | 1.142 | 0.169 | 0.681 | 0.625(0.067~5.859) |
| 离婚或丧偶 | -0.589 | 0.263 | 5.008 | 0.025 | 0.555(0.331~0.929) |
| NRS 2002评分 | 1.645 | 0.264 | 38.731 | <0.001 | 5.182(1.287~20.864) |
| mRS评分 | -2.488 | 0.291 | 73.511 | <0.001 | 0.083(0.047~0.146) |
| MMSE评分 | -0.347 | 0.038 | 85.536 | <0.001 | 0.707(0.657~0.761) |
| HAMA评分 | 0.418 | 0.048 | 74.446 | <0.001 | 1.520(1.382~1.671) |
| 体脂质量 | -0.217 | 0.024 | 83.249 | <0.001 | 0.805(0.769~0.844) |
| 骨骼肌质量 | -0.846 | 0.134 | 39.746 | <0.001 | 0.429(0.330~0.558) |
| 肌肉质量 | -2.617 | 0.619 | 17.860 | <0.001 | 0.073(0.022~0.246) |
| 全身相位角 | -5.809 | 0.935 | 38.137 | <0.001 | 0.003(<0.001~0.019) |
| TMA | -0.115 | 0.015 | 60.834 | <0.001 | 0.891(0.865~0.917) |
| TMT | -1.339 | 0.220 | 37.183 | <0.001 | 0.262(0.160~0.430) |
| 血清白蛋白 | -0.288 | 0.040 | 51.720 | <0.001 | 0.750(0.694~0.811) |
| 变量 | B | SE | Wald χ2值 | P值 | OR(95%CI) |
|---|---|---|---|---|---|
| 年龄 | 0.541 | 0.229 | 5.576 | 0.018 | 1.717(1.223~2.410) |
| NIHSS评分(以>5分为参照) | 1.167 | 0.288 | 16.426 | <0.001 | 3.213(1.829~5.643) |
| 卒中类型(以大动脉粥样硬化型为参照) | |||||
| 小动脉闭塞型 | -0.517 | 1.278 | 0.164 | 0.688 | 0.596(0.048~7.431) |
| 心源性梗死型 | -0.552 | 0.986 | 0.313 | 0.576 | 0.576(0.185~1.792) |
| 不明原因型 | -0.774 | 0.667 | 1.347 | 0.247 | 0.461(0.125~1.708) |
| 高脂血症(以无为参照) | -4.200 | 5.221 | 0.634 | 0.426 | 0.015(0.001~0.226) |
| NRS 2002评分 | 0.290 | 0.125 | 5.412 | 0.020 | 1.337(1.045~1.711) |
| mRS评分 | -2.064 | 1.918 | 1.157 | 0.282 | 0.127(0.003~5.437) |
| MMSE评分 | -0.491 | 0.291 | 2.848 | 0.092 | 0.612(0.346~1.083) |
| HAMA评分 | -0.478 | 0.300 | 2.543 | 0.112 | 0.620(0.310~1.240) |
| TMA | -0.247 | 0.103 | 5.765 | 0.016 | 0.781(0.639~0.955) |
| TMT | -1.019 | 0.773 | 1.737 | 0.189 | 0.361(0.079~1.642) |
| 血清白蛋白 | -0.467 | 0.334 | 1.958 | 0.161 | 0.627(0.327~1.204) |
表4 AIS患者肌肉衰减症影响因素的多因素Logistic回归分析
Table 4 Multi Logistic regression analysis of factors affecting muscle atrophy in patients with AIS
| 变量 | B | SE | Wald χ2值 | P值 | OR(95%CI) |
|---|---|---|---|---|---|
| 年龄 | 0.541 | 0.229 | 5.576 | 0.018 | 1.717(1.223~2.410) |
| NIHSS评分(以>5分为参照) | 1.167 | 0.288 | 16.426 | <0.001 | 3.213(1.829~5.643) |
| 卒中类型(以大动脉粥样硬化型为参照) | |||||
| 小动脉闭塞型 | -0.517 | 1.278 | 0.164 | 0.688 | 0.596(0.048~7.431) |
| 心源性梗死型 | -0.552 | 0.986 | 0.313 | 0.576 | 0.576(0.185~1.792) |
| 不明原因型 | -0.774 | 0.667 | 1.347 | 0.247 | 0.461(0.125~1.708) |
| 高脂血症(以无为参照) | -4.200 | 5.221 | 0.634 | 0.426 | 0.015(0.001~0.226) |
| NRS 2002评分 | 0.290 | 0.125 | 5.412 | 0.020 | 1.337(1.045~1.711) |
| mRS评分 | -2.064 | 1.918 | 1.157 | 0.282 | 0.127(0.003~5.437) |
| MMSE评分 | -0.491 | 0.291 | 2.848 | 0.092 | 0.612(0.346~1.083) |
| HAMA评分 | -0.478 | 0.300 | 2.543 | 0.112 | 0.620(0.310~1.240) |
| TMA | -0.247 | 0.103 | 5.765 | 0.016 | 0.781(0.639~0.955) |
| TMT | -1.019 | 0.773 | 1.737 | 0.189 | 0.361(0.079~1.642) |
| 血清白蛋白 | -0.467 | 0.334 | 1.958 | 0.161 | 0.627(0.327~1.204) |
| 组别 | 例数 | 性别[例(%)] | 糖尿病[例(%)] | NRS 2002评分[例(%)] | mRS评分[例(%)] | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | 否 | 是 | <3分 | ≥3分 | ≤2分 | >2分 | ||||
| 训练集 | 398 | 274(68.84) | 124(31.16) | 360(90.45) | 38(9.55) | 125(31.41) | 273(68.59) | 226(56.78) | 172(43.22) | ||
| 验证集 | 133 | 91(68.42) | 42(31.58) | 118(88.72) | 15(11.28) | 51(38.35) | 82(61.65) | 80(60.15) | 53(39.85) | ||
| χ2(t)值 | 0.008 | 0.332 | 0.659 | 98.11 | |||||||
| P值 | 0.191 | 0.343 | 0.469 | 0.146 | |||||||
| 组别 | 婚姻状况[例(%)] | 吸烟状况[例(%)] | 饮酒状况[例(%)] | 高脂血症[例(%)] | 高血压[例(%)] | ||||||
| 未婚 | 已婚 | 离婚或丧偶 | 从不吸烟 | 现在吸烟 | 现在饮酒 | 现在不饮 | 否 | 是 | 否 | 是 | |
| 训练集 | 3(0.75) | 330(82.91) | 65(16.33) | 254(63.82) | 144(36.18) | 277(69.60) | 121(30.40) | 341(85.68) | 57(14.32) | 230(57.79) | 168(42.21) |
| 验证集 | 2(1.50) | 105(78.95) | 26(19.55) | 86(64.66) | 47(35.34) | 96(72.18) | 37(27.82) | 111(83.46) | 22(16.54) | 67(50.38) | 66(49.62) |
| χ2(t)值 | 1.389 | 0.031 | 0.318 | 0.388 | 2.223 | ||||||
| P值 | 0.090 | 0.463 | 0.361 | 0.469 | 0.258 | ||||||
| 组别 | 卒中类型[例(%)] | 年龄( | 血清白蛋白( | TMA( | TMT( | MMSE评分( | MoCA评分( | ||||
| 大动脉粥样硬化型 | 小动脉闭塞型 | 心源性梗死型 | 其他类型 | ||||||||
| 训练集 | 254(63.82) | 72(18.09) | 35(8.79) | 37(9.30) | 61.08±10.88 | 40.03±3.40 | 512.22±36.96 | 4.35±0.77 | 25.18±3.86 | 23.70±4.49 | |
| 验证集 | 94(70.68) | 19(14.29) | 9(6.77) | 11(8.27) | 61.64±12.04 | 40.15±3.20 | 514.81±42.57 | 4.28±0.85 | 25.40±4.00 | 23.94±4.63 | |
| χ2(t)值 | 2.168 | 0.501a | -0.362a | -0.671a | 0.780a | -0.558a | -0.538a | ||||
| P值 | 0.115 | 0.387 | 0.810 | 0.788 | 0.901 | 0.649 | 0.090 | ||||
| 组别 | HAMA评分( | HAMD评分( | BMI( | 肌肉质量( | 骨骼肌质量( | 体脂质量( | NIHSS评分[例(%)] | 肌肉衰减症[例(%)] | |||
| ≤5分 | >5分 | 否 | 是 | ||||||||
| 训练集 | 10.47±2.56 | 4.34±3.20 | 25.47±3.35 | 42.15±11.08 | 40.91±11.53 | 14.57±7.03 | 319(80.15) | 79(19.85) | 323(81.16) | 75(18.84) | |
| 验证集 | 11.32±3.25 | 4.64±3.13 | 25.37±3.28 | 42.16±11.50 | 39.23±12.19 | 14.34±7.24 | 96(72.18) | 37(27.82) | 102(76.69) | 31(23.31) | |
| χ2(t)值 | -3.075a | -0.978a | 0.238a | -0.006a | 1.435a | 0.312a | 3.709 | 1.243 | |||
| P值 | 0.788 | 0.076 | 0.116 | 0.544 | 0.715 | 0.567 | 0.559 | 0.873 | |||
表5 训练集与验证集患者一般资料比较
Table 5 Comparison of general demographics between training cohort and test cohort
| 组别 | 例数 | 性别[例(%)] | 糖尿病[例(%)] | NRS 2002评分[例(%)] | mRS评分[例(%)] | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | 否 | 是 | <3分 | ≥3分 | ≤2分 | >2分 | ||||
| 训练集 | 398 | 274(68.84) | 124(31.16) | 360(90.45) | 38(9.55) | 125(31.41) | 273(68.59) | 226(56.78) | 172(43.22) | ||
| 验证集 | 133 | 91(68.42) | 42(31.58) | 118(88.72) | 15(11.28) | 51(38.35) | 82(61.65) | 80(60.15) | 53(39.85) | ||
| χ2(t)值 | 0.008 | 0.332 | 0.659 | 98.11 | |||||||
| P值 | 0.191 | 0.343 | 0.469 | 0.146 | |||||||
| 组别 | 婚姻状况[例(%)] | 吸烟状况[例(%)] | 饮酒状况[例(%)] | 高脂血症[例(%)] | 高血压[例(%)] | ||||||
| 未婚 | 已婚 | 离婚或丧偶 | 从不吸烟 | 现在吸烟 | 现在饮酒 | 现在不饮 | 否 | 是 | 否 | 是 | |
| 训练集 | 3(0.75) | 330(82.91) | 65(16.33) | 254(63.82) | 144(36.18) | 277(69.60) | 121(30.40) | 341(85.68) | 57(14.32) | 230(57.79) | 168(42.21) |
| 验证集 | 2(1.50) | 105(78.95) | 26(19.55) | 86(64.66) | 47(35.34) | 96(72.18) | 37(27.82) | 111(83.46) | 22(16.54) | 67(50.38) | 66(49.62) |
| χ2(t)值 | 1.389 | 0.031 | 0.318 | 0.388 | 2.223 | ||||||
| P值 | 0.090 | 0.463 | 0.361 | 0.469 | 0.258 | ||||||
| 组别 | 卒中类型[例(%)] | 年龄( | 血清白蛋白( | TMA( | TMT( | MMSE评分( | MoCA评分( | ||||
| 大动脉粥样硬化型 | 小动脉闭塞型 | 心源性梗死型 | 其他类型 | ||||||||
| 训练集 | 254(63.82) | 72(18.09) | 35(8.79) | 37(9.30) | 61.08±10.88 | 40.03±3.40 | 512.22±36.96 | 4.35±0.77 | 25.18±3.86 | 23.70±4.49 | |
| 验证集 | 94(70.68) | 19(14.29) | 9(6.77) | 11(8.27) | 61.64±12.04 | 40.15±3.20 | 514.81±42.57 | 4.28±0.85 | 25.40±4.00 | 23.94±4.63 | |
| χ2(t)值 | 2.168 | 0.501a | -0.362a | -0.671a | 0.780a | -0.558a | -0.538a | ||||
| P值 | 0.115 | 0.387 | 0.810 | 0.788 | 0.901 | 0.649 | 0.090 | ||||
| 组别 | HAMA评分( | HAMD评分( | BMI( | 肌肉质量( | 骨骼肌质量( | 体脂质量( | NIHSS评分[例(%)] | 肌肉衰减症[例(%)] | |||
| ≤5分 | >5分 | 否 | 是 | ||||||||
| 训练集 | 10.47±2.56 | 4.34±3.20 | 25.47±3.35 | 42.15±11.08 | 40.91±11.53 | 14.57±7.03 | 319(80.15) | 79(19.85) | 323(81.16) | 75(18.84) | |
| 验证集 | 11.32±3.25 | 4.64±3.13 | 25.37±3.28 | 42.16±11.50 | 39.23±12.19 | 14.34±7.24 | 96(72.18) | 37(27.82) | 102(76.69) | 31(23.31) | |
| χ2(t)值 | -3.075a | -0.978a | 0.238a | -0.006a | 1.435a | 0.312a | 3.709 | 1.243 | |||
| P值 | 0.788 | 0.076 | 0.116 | 0.544 | 0.715 | 0.567 | 0.559 | 0.873 | |||
| [1] |
GBD 2021 Stroke Risk Factor Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021[J]. Lancet Neurol, 2024, 23(10): 973-1003. DOI: 10.1016/S1474-4422(24)00369-7.
|
| [2] |
国家心血管病中心, 中国心血管健康与疾病报告撰写组. 中国心血管健康与疾病报告2024概要[J]. 中国循环杂志, 2025, 40(6): 521-559. DOI: 10.3969/j.issn.1000-3614.2025.06.001.
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组, 彭斌, 等. 中国急性缺血性卒中诊治指南2023[J]. 中华神经科杂志, 2024, 57(6): 523-559. DOI: 10.3969/j.issn.1673-5765.2024.08.013.
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [21] |
|
| [22] |
|
| [23] |
|
| [24] |
|
| [25] |
|
| [26] |
|
| [27] |
|
| [28] |
|
| [29] |
|
| [30] |
|
| [31] |
崔华, 王朝晖, 吴剑卿, 等. 老年人肌少症防控干预中国专家共识(2023)[J]. 中华老年医学杂志, 2023, 42(2): 144-153.
|
| [32] |
|
| [1] | 李纪新, 邱林杰, 任燕, 王文茹, 李美洁, 栗文婕, 邹姹姹, 吴梓敬, 张晋. 肌肉与脂肪比值对非超重/肥胖2型糖尿病的预测价值研究[J]. 中国全科医学, 2026, 29(06): 726-732. |
| [2] | 雷淳心, 张曦亚, 张燕, 陈嘉琪, 刘子菡, 罗静, 陶庆文. 原发性干燥综合征燥瘀互结证患者临床特点及影响因素研究[J]. 中国全科医学, 2026, 29(06): 718-725. |
| [3] | 刘璠, 李嘉丽, 柯立鑫, 张强, 陈嘉慧, 卢存存, 赵信科. 1990—2021年全球与中国60岁及以上人群高胆固醇血症的疾病负担:趋势分析与模型预测[J]. 中国全科医学, 2026, 29(05): 631-640. |
| [4] | 夏莹, 吴新日, 张彩琴, 洪忻. 基于"生命八要素"评分的社区居民心血管健康分布及影响因素研究[J]. 中国全科医学, 2026, 29(05): 597-605. |
| [5] | 奚谦, 申颖, 赵璨, 纪舒妤, 彭厚瑄, 覃金琼, 王璇, 郑艳萍, 左延莉. 乡镇卫生院住院患者多重慢病共患模式、住院服务利用及影响因素研究[J]. 中国全科医学, 2026, 29(04): 498-508. |
| [6] | 江晓蕊, 闫玉瑶, 卫靖靖, 乔利杰, 彭广操, 朱明军. 冠心病患者并发心力衰竭风险预测模型的系统评价[J]. 中国全科医学, 2026, 29(03): 393-402. |
| [7] | 赵雪姣, 李娟, 李雨洁, 卢婷, 先丽红, 颜欢. 中国脑卒中后认知障碍患病趋势及影响因素的Meta分析[J]. 中国全科医学, 2026, 29(03): 380-392. |
| [8] | 赵颖颖, 苏萍, 陈巧巧, 逄锦宏, 施婕, 王雅倩, 李秋春, 何蕊言, 王玥, 陈学禹, 于媛媛, 迟蔚蔚. 多种慢性病对年龄相关性黄斑变性风险的影响及其交互效应研究[J]. 中国全科医学, 2026, 29(02): 213-218. |
| [9] | 马玉萍, 乔梦媛, 何雁云, 徐曼如, 陈崇利, 伍文彬. "体病相关"视角下探析老年2型糖尿病伴轻度认知障碍现状及影响因素研究:以四川省为例[J]. 中国全科医学, 2026, 29(02): 188-194. |
| [10] | 闵叶平, 薛垚, 冯同保, 张合, 刘福菁. 血压反应指数对老年重症肺炎休克患者急性肾损伤的影响研究[J]. 中国全科医学, 2026, 29(02): 207-212. |
| [11] | 苏宁, 刘平平, 郭宇濛, 芦明月, 朱瑞, 于建平. 2019—2022年北京市基层传染病防控能力及影响因素研究[J]. 中国全科医学, 2025, 28(35): 4473-4478. |
| [12] | 王瓅珠, 李思涵, 王心怡, 冒孙汐, 邱杨, 王中华. 基于ITHBC模型的糖尿病知识、自我效能对农村2型糖尿病患者自我管理和生存质量的影响路径研究[J]. 中国全科医学, 2025, 28(34): 4351-4358. |
| [13] | 马念, 王子云, 滕小艳, 陈云, 孙正勇. 老年高血压患者共病现状及影响因素的城乡差异性研究[J]. 中国全科医学, 2025, 28(34): 4344-4350. |
| [14] | 尹佳佳, 姚丽, 周梓涵, 李钦钦, 王庭瑞, 刘焱. 我国不同地区老年人共病患病影响因素的Meta分析:南北方对比研究[J]. 中国全科医学, 2025, 28(34): 4326-4336. |
| [15] | 刘春燕, 邓朝晖, 宋颖博, 杨芳, 史茜, 李永鑫, 张新. 新疆地区居民高血压、糖尿病、血脂异常患病及共病情况研究[J]. 中国全科医学, 2025, 28(32): 4031-4037. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





