中国全科医学 ›› 2025, Vol. 28 ›› Issue (16): 2017-2024.DOI: 10.12114/j.issn.1007-9572.2024.0279
所属专题: 心血管最新文章合辑; 生活方式干预相关研究最新文章合集
安芹彧1, 王艺颖2, 张小丹1, 张畑霖3, 詹清清3, 张福艳3, 刘涛1,2,*( ), 吴延莉2,*(
), 吴延莉2,*( )
)
收稿日期:2024-06-13
修回日期:2025-01-23
出版日期:2025-06-05
发布日期:2025-04-22
通讯作者:
刘涛, 吴延莉
作者贡献:
安芹彧提出主要研究目标,负责研究的构思与设计,研究的实施,撰写论文;王艺颖、张小丹、张畑霖进行数据的收集与整理,统计学处理,图、表的绘制与展示;詹清清、张福艳进行论文的修订;刘涛、吴延莉负责文章的质量控制与审查,对文章整体负责,监督管理。
基金资助:
AN Qinyu1, WANG Yiying2, ZHANG Xiaodan1, ZHANG Tianlin3, ZHAN Qingqing3, ZHANG Fuyan3, LIU Tao1,2,*( ), WU Yanli2,*(
), WU Yanli2,*( )
)
Received:2024-06-13
Revised:2025-01-23
Published:2025-06-05
Online:2025-04-22
Contact:
LIU Tao, WU Yanli
摘要: 背景 心血管疾病(CVD)是一个全球性的健康问题,目前尚不清楚社会经济地位(SES)和健康生活方式(HL)对CVD发病是否有影响。 目的 了解SES、HL与CVD的关系,为人群CVD防控提供依据。 方法 本研究采用多阶段整群随机抽样方法,于2010年抽取9 280名贵州省12个县/区18岁及以上常住居民进行基线调查,于2016—2020年对该队列所有人群进行随访,由经过统一培训且考核合格的人员进行面对面访谈,包括基本情况、生活方式(吸烟、饮酒、蔬菜水果摄入等)、既往史等,根据调查对象是否发病分为CVD组(123名)和非CVD组(4 025名);运用COX比例风险回归模型分析SES、HL对CVD发病的影响,采用加速失效时间模型分析不同SES、HL对CVD发病时间的影响。 结果 排除基线CVD患者、失访者及信息缺失者后,最终纳入分析的有效样本量为4 148名,CVD发病123名,发病密度为4.13/1 000人年。COX比例风险回归模型分析结果显示,与SES低分组人群相比,SES高分组人群CVD发病风险下降40.60%(HR=0.594,95%CI=0.402~0.878)。与≤6种HL人群相比,拥有8种、≥9种HL人群CVD发病风险分别下降44.40%(HR=0.556,95%CI=0.320~0.968)、49.20%(HR=0.508,95%CI=0.284~0.912)。与SES低分组且HL≤6种的人群相比,SES低分组且HL为7、8、≥9种的人群CVD发病风险无统计学意义(P>0.05);SES高分组且HL为8种和≥9种人群CVD发病风险将分别下降61.80%(HR=0.382,95%CI=0.163~0.894)、70.20%(HR=0.298,95%CI=0.119~0.748),CVD发病风险呈下降趋势(P趋势<0.001)。加速失效时间模型结果显示,与SES低分组且HL≤6种的人群相比,SES高分组且拥有8种和≥9种HL人群CVD发病时间分别推迟1.148年(95%CI=0.049~2.247)、1.407年(95%CI=0.227~2.588)。 结论 不同SES、HL与CVD发病呈负相关;在高SES人群中,随着HL种类的增加CVD发病时间随之延长。低SES人群是贵州省CVD防控的重点人群,应采取措施提高其健康素养,同时针对性地开展CVD的健康教育与健康促进工作。
中图分类号:
| SES衡量指标 | 赋分情况 |
|---|---|
| 家庭人均年收入 | <2 700元=1分,2 700元~=2分,5 122元~=3分,≥10 000元=4分 |
| 职业 | 无业=1分,其他劳动者=2分,体力劳动者=3分,脑力劳动者=4分 |
| 个人受教育程度 | 文盲、半文盲=1分,小学=2分,初中=3分,高中/中专及以上=4分 |
表1 SES衡量指标的赋分标准
Table 1 Criteria for assigning measurement indicators of SES
| SES衡量指标 | 赋分情况 |
|---|---|
| 家庭人均年收入 | <2 700元=1分,2 700元~=2分,5 122元~=3分,≥10 000元=4分 |
| 职业 | 无业=1分,其他劳动者=2分,体力劳动者=3分,脑力劳动者=4分 |
| 个人受教育程度 | 文盲、半文盲=1分,小学=2分,初中=3分,高中/中专及以上=4分 |
| 特征 | CVD组(n=123) | 非CVD组(n=4 025) | χ2(t)值 | P值 |
|---|---|---|---|---|
| 性别[名(%)] | 0.169 | 0.681 | ||
| 男 | 57(46.30) | 1 941(48.20) | ||
| 女 | 66(53.70) | 2 084(51.80) | ||
| 年龄[名(%)] | 45.915 | <0.001 | ||
| ≤44岁 | 29(23.60) | 2 194(54.50) | ||
| >44岁 | 94(76.40) | 1 831(45.50) | ||
| 民族[名(%)] | 4.313 | 0.038 | ||
| 汉族 | 89(72.40) | 2 544(63.20) | ||
| 少数民族 | 34(27.60) | 1 481(36.80) | ||
| 城乡居住地[名(%)] | 2.116 | 0.146 | ||
| 城市 | 34(27.60) | 1 366(33.90) | ||
| 农村 | 89(72.40) | 2 659(66.10) | ||
| 婚姻状况[名(%)] | 10.368 | 0.006 | ||
| 未婚 | 3(2.40) | 359(8.90) | ||
| 已婚/同居 | 101(82.10) | 3 289(81.70) | ||
| 离异/丧偶/分居 | 19(15.40) | 377(9.40) | ||
| 个人受教育程度[名(%)] | 19.175 | <0.001 | ||
| 文盲/半文盲 | 57(46.30) | 1 180(29.30) | ||
| 小学 | 23(18.70) | 848(21.10) | ||
| 初中 | 23(18.70) | 1 315(32.70) | ||
| 高中/中专及以上 | 20(16.30) | 682(16.90) | ||
| 职业类型[名(%)] | 1.749 | 0.626 | ||
| 不在业人员 | 27(22.00) | 710(17.60) | ||
| 其他劳动者 | 11(8.90) | 362(9.00) | ||
| 体力劳动者 | 70(56.90) | 2 372(58.90) | ||
| 脑力劳动者 | 15(12.20) | 581(14.40) | ||
| 家庭人均年收入[名(%)] | 0.095 | 0.992 | ||
| <2 700元 | 27(22.00) | 888(22.10) | ||
| 2 700~元 | 30(24.40) | 987(24.50) | ||
| 5 122~元 | 30(24.40) | 937(23.30) | ||
| ≥10 000元 | 36(29.30) | 1 213(30.10) | ||
| SES分组[名(%)] | 10.137 | 0.001 | ||
| SES低分组 | 78(63.40) | 1 966(48.80) | ||
| SES高分组 | 45(36.60) | 2 059(51.20) | ||
| 每日静态时间<4 h[名(%)] | 0.415 | 0.520 | ||
| 否 | 70(56.90) | 2 407(59.80) | ||
| 是 | 53(43.10) | 1 618(40.20) | ||
| 从不吸烟[名(%)] | 0.058 | 0.809 | ||
| 否 | 41(33.30) | 1 300(32.30) | ||
| 是 | 82(66.70) | 2 725(67.70) | ||
| 从不饮酒[名(%)] | 1.004 | 0.316 | ||
| 否 | 40(32.50) | 1 487(36.90) | ||
| 是 | 83(67.50) | 2 538(63.10) | ||
| 水果蔬菜摄入量≥400 g/d[名(%)] | 1.306 | 0.253 | ||
| 否 | 56(45.50) | 2 043(50.80) | ||
| 是 | 67(54.50) | 1 982(49.20) | ||
| 烹饪油摄入≤25 g/d[名(%)] | 2.019 | 0.155 | ||
| 否 | 99(80.50) | 3 013(74.90) | ||
| 是 | 24(19.50) | 1 012(25.10) | ||
| 腰高比<0.5[名(%)] | 5.464 | 0.019 | ||
| 否 | 60(48.80) | 1 544(38.40) | ||
| 是 | 63(51.20) | 2 481(61.60) | ||
| 每周中等强度运动≥150 min[名(%)] | 0.105 | 0.745 | ||
| 否 | 44(35.80) | 1 383(34.40) | ||
| 是 | 79(64.20) | 2 642(65.60) | ||
| 心理健康情况[名(%)] | 7.655 | 0.006 | ||
| 心理不健康 | 14(11.40) | 222(5.50) | ||
| 心理健康 | 109(88.60) | 3 803(94.50) | ||
| 食盐摄入<6 g/d[名(%)] | 5.820 | 0.016 | ||
| 否 | 98(79.70) | 2 799(69.50) | ||
| 是 | 25(20.30) | 1 226(30.50) | ||
| 谷薯类摄入≥200 g/d[名(%)] | 0.722 | 0.395 | ||
| 否 | 11(8.90) | 280(7.00) | ||
| 是 | 112(91.10) | 3 745(93.00) | ||
| 7 h/d≤睡眠时间≤9 h/d[名(%)] | 12.560 | <0.001 | ||
| 否 | 55(44.70) | 1 200(29.80) | ||
| 是 | 68(55.30) | 2 825(70.20) | ||
| 不食用油炸食品[名(%)] | 0.464 | 0.496 | ||
| 否 | 40(32.50) | 1 429(35.50) | ||
| 是 | 83(67.50) | 2 596(64.50) | ||
| BMI分级[名(%)] | 3.869 | 0.276 | ||
| 轻体质量 | 2(1.60) | 207(5.10) | ||
| 正常 | 74(60.20) | 2 444(60.70) | ||
| 超重 | 35(28.50) | 1 071(26.60) | ||
| 肥胖 | 12(9.80) | 303(7.50) | ||
| MET( | 103.89±113.58 | 112.10±118.70 | 0.757b | 0.449 |
| 糖尿病疾病史a | 4.462 | 0.107 | ||
| 否 | 106(86.20) | 3 670(91.20) | ||
| 是 | 16(13.00) | 345(8.60) | ||
| 血脂异常[名(%)] | 0.566 | 0.452 | ||
| 否 | 50(40.70) | 1 502(37.30) | ||
| 是 | 73(59.30) | 2 523(62.70) | ||
| 高血压疾病史[名(%)] | 15.744 | <0.001 | ||
| 否 | 71(57.70) | 2 970(73.80) | ||
| 是 | 52(42.30) | 1 055(26.20) | ||
| HL分组[名(%)] | 11.430 | 0.010 | ||
| ≤6种 | 47(38.20) | 1 308(32.50) | ||
| 7种 | 38(30.90) | 880(21.90) | ||
| 8种 | 19(15.40) | 862(21.40) | ||
| ≥9种 | 19(15.40) | 975(24.20) | ||
表2 基线人群基本特征
Table 2 Baseline characteristics of participants
| 特征 | CVD组(n=123) | 非CVD组(n=4 025) | χ2(t)值 | P值 |
|---|---|---|---|---|
| 性别[名(%)] | 0.169 | 0.681 | ||
| 男 | 57(46.30) | 1 941(48.20) | ||
| 女 | 66(53.70) | 2 084(51.80) | ||
| 年龄[名(%)] | 45.915 | <0.001 | ||
| ≤44岁 | 29(23.60) | 2 194(54.50) | ||
| >44岁 | 94(76.40) | 1 831(45.50) | ||
| 民族[名(%)] | 4.313 | 0.038 | ||
| 汉族 | 89(72.40) | 2 544(63.20) | ||
| 少数民族 | 34(27.60) | 1 481(36.80) | ||
| 城乡居住地[名(%)] | 2.116 | 0.146 | ||
| 城市 | 34(27.60) | 1 366(33.90) | ||
| 农村 | 89(72.40) | 2 659(66.10) | ||
| 婚姻状况[名(%)] | 10.368 | 0.006 | ||
| 未婚 | 3(2.40) | 359(8.90) | ||
| 已婚/同居 | 101(82.10) | 3 289(81.70) | ||
| 离异/丧偶/分居 | 19(15.40) | 377(9.40) | ||
| 个人受教育程度[名(%)] | 19.175 | <0.001 | ||
| 文盲/半文盲 | 57(46.30) | 1 180(29.30) | ||
| 小学 | 23(18.70) | 848(21.10) | ||
| 初中 | 23(18.70) | 1 315(32.70) | ||
| 高中/中专及以上 | 20(16.30) | 682(16.90) | ||
| 职业类型[名(%)] | 1.749 | 0.626 | ||
| 不在业人员 | 27(22.00) | 710(17.60) | ||
| 其他劳动者 | 11(8.90) | 362(9.00) | ||
| 体力劳动者 | 70(56.90) | 2 372(58.90) | ||
| 脑力劳动者 | 15(12.20) | 581(14.40) | ||
| 家庭人均年收入[名(%)] | 0.095 | 0.992 | ||
| <2 700元 | 27(22.00) | 888(22.10) | ||
| 2 700~元 | 30(24.40) | 987(24.50) | ||
| 5 122~元 | 30(24.40) | 937(23.30) | ||
| ≥10 000元 | 36(29.30) | 1 213(30.10) | ||
| SES分组[名(%)] | 10.137 | 0.001 | ||
| SES低分组 | 78(63.40) | 1 966(48.80) | ||
| SES高分组 | 45(36.60) | 2 059(51.20) | ||
| 每日静态时间<4 h[名(%)] | 0.415 | 0.520 | ||
| 否 | 70(56.90) | 2 407(59.80) | ||
| 是 | 53(43.10) | 1 618(40.20) | ||
| 从不吸烟[名(%)] | 0.058 | 0.809 | ||
| 否 | 41(33.30) | 1 300(32.30) | ||
| 是 | 82(66.70) | 2 725(67.70) | ||
| 从不饮酒[名(%)] | 1.004 | 0.316 | ||
| 否 | 40(32.50) | 1 487(36.90) | ||
| 是 | 83(67.50) | 2 538(63.10) | ||
| 水果蔬菜摄入量≥400 g/d[名(%)] | 1.306 | 0.253 | ||
| 否 | 56(45.50) | 2 043(50.80) | ||
| 是 | 67(54.50) | 1 982(49.20) | ||
| 烹饪油摄入≤25 g/d[名(%)] | 2.019 | 0.155 | ||
| 否 | 99(80.50) | 3 013(74.90) | ||
| 是 | 24(19.50) | 1 012(25.10) | ||
| 腰高比<0.5[名(%)] | 5.464 | 0.019 | ||
| 否 | 60(48.80) | 1 544(38.40) | ||
| 是 | 63(51.20) | 2 481(61.60) | ||
| 每周中等强度运动≥150 min[名(%)] | 0.105 | 0.745 | ||
| 否 | 44(35.80) | 1 383(34.40) | ||
| 是 | 79(64.20) | 2 642(65.60) | ||
| 心理健康情况[名(%)] | 7.655 | 0.006 | ||
| 心理不健康 | 14(11.40) | 222(5.50) | ||
| 心理健康 | 109(88.60) | 3 803(94.50) | ||
| 食盐摄入<6 g/d[名(%)] | 5.820 | 0.016 | ||
| 否 | 98(79.70) | 2 799(69.50) | ||
| 是 | 25(20.30) | 1 226(30.50) | ||
| 谷薯类摄入≥200 g/d[名(%)] | 0.722 | 0.395 | ||
| 否 | 11(8.90) | 280(7.00) | ||
| 是 | 112(91.10) | 3 745(93.00) | ||
| 7 h/d≤睡眠时间≤9 h/d[名(%)] | 12.560 | <0.001 | ||
| 否 | 55(44.70) | 1 200(29.80) | ||
| 是 | 68(55.30) | 2 825(70.20) | ||
| 不食用油炸食品[名(%)] | 0.464 | 0.496 | ||
| 否 | 40(32.50) | 1 429(35.50) | ||
| 是 | 83(67.50) | 2 596(64.50) | ||
| BMI分级[名(%)] | 3.869 | 0.276 | ||
| 轻体质量 | 2(1.60) | 207(5.10) | ||
| 正常 | 74(60.20) | 2 444(60.70) | ||
| 超重 | 35(28.50) | 1 071(26.60) | ||
| 肥胖 | 12(9.80) | 303(7.50) | ||
| MET( | 103.89±113.58 | 112.10±118.70 | 0.757b | 0.449 |
| 糖尿病疾病史a | 4.462 | 0.107 | ||
| 否 | 106(86.20) | 3 670(91.20) | ||
| 是 | 16(13.00) | 345(8.60) | ||
| 血脂异常[名(%)] | 0.566 | 0.452 | ||
| 否 | 50(40.70) | 1 502(37.30) | ||
| 是 | 73(59.30) | 2 523(62.70) | ||
| 高血压疾病史[名(%)] | 15.744 | <0.001 | ||
| 否 | 71(57.70) | 2 970(73.80) | ||
| 是 | 52(42.30) | 1 055(26.20) | ||
| HL分组[名(%)] | 11.430 | 0.010 | ||
| ≤6种 | 47(38.20) | 1 308(32.50) | ||
| 7种 | 38(30.90) | 880(21.90) | ||
| 8种 | 19(15.40) | 862(21.40) | ||
| ≥9种 | 19(15.40) | 975(24.20) | ||
| 特征 | 新发病数(人) | 发病密度(/1 000人年) | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P值 | HR(95%CI) | P值 | HR(95%CI) | P值 | |||
| SES低分组 | 78 | 5.39 | 1.000 | — | 1.000 | — | 1.000 | — |
| SES高分组 | 45 | 2.94 | 0.476(0.329~0.689) | <0.001 | 0.565(0.385~0.829) | 0.003 | 0.594(0.402~0.878) | 0.009 |
表3 SES对CVD发病的COX比例风险回归模型分析
Table 3 COX regression analysis of CVD onset by SES
| 特征 | 新发病数(人) | 发病密度(/1 000人年) | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P值 | HR(95%CI) | P值 | HR(95%CI) | P值 | |||
| SES低分组 | 78 | 5.39 | 1.000 | — | 1.000 | — | 1.000 | — |
| SES高分组 | 45 | 2.94 | 0.476(0.329~0.689) | <0.001 | 0.565(0.385~0.829) | 0.003 | 0.594(0.402~0.878) | 0.009 |
| 特征 | 新发病数(人) | 发病密度(/1 000人年) | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P值 | HR(95%CI) | P值 | HR(95%CI) | P值 | |||
| ≤6种 | 47 | 4.92 | 1.000 | — | 1.000 | — | 1.000 | — |
| 7种 | 38 | 5.80 | 1.070(0.698~1.642) | 0.756 | 1.118(0.721~1.733) | 0.619 | 1.140(0.732~1.776) | 0.561 |
| 8种 | 19 | 2.99 | 0.514(0.301~0.876) | 0.014 | 0.547(0.316~0.946) | 0.031 | 0.556(0.320~0.968) | 0.038 |
| ≥9种 | 19 | 2.61 | 0.412(0.242~0.703) | 0.001 | 0.481(0.272~0.848) | 0.012 | 0.508(0.284~0.912) | 0.023 |
表4 HL对CVD发病的COX比例风险回归模型分析
Table 4 COX regression analysis of healthy lifestyle on CVD onset
| 特征 | 新发病数(人) | 发病密度(/1 000人年) | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P值 | HR(95%CI) | P值 | HR(95%CI) | P值 | |||
| ≤6种 | 47 | 4.92 | 1.000 | — | 1.000 | — | 1.000 | — |
| 7种 | 38 | 5.80 | 1.070(0.698~1.642) | 0.756 | 1.118(0.721~1.733) | 0.619 | 1.140(0.732~1.776) | 0.561 |
| 8种 | 19 | 2.99 | 0.514(0.301~0.876) | 0.014 | 0.547(0.316~0.946) | 0.031 | 0.556(0.320~0.968) | 0.038 |
| ≥9种 | 19 | 2.61 | 0.412(0.242~0.703) | 0.001 | 0.481(0.272~0.848) | 0.012 | 0.508(0.284~0.912) | 0.023 |
| SES分组 | HL分组 | 新发病数(人) | 发病密度(/1 000人年) | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P值 | HR(95%CI) | P值 | HR(95%CI) | P值 | ||||
| SES低分组 | ≤6种 | 26 | 6.69 | 1.000 | — | 1.000 | — | 1.000 | — |
| SES低分组 | 7种 | 27 | 8.09 | 1.138(0.664~1.950) | 0.638 | 1.244(0.721~2.146) | 0.432 | 1.295(0.746~2.250) | 0.359 |
| SES低分组 | 8种 | 12 | 3.56 | 0.468(0.236~0.927) | 0.030 | 0.543(0.271~1.086) | 0.084 | 0.564(0.281~1.134) | 0.108 |
| SES低分组 | ≥9种 | 13 | 3.37 | 0.408(0.210~0.795) | 0.008 | 0.512(0.257~1.018) | 0.056 | 0.560(0.278~1.129) | 0.105 |
| SES高分组 | ≤6种 | 21 | 3.70 | 0.509(0.287~0.906) | 0.022 | 0.643(0.358~1.156) | 0.140 | 0.683(0.378~1.235) | 0.208 |
| SES高分组 | 7种 | 11 | 3.42 | 0.404(0.199~0.819) | 0.012 | 0.554(0.272~1.131) | 0.105 | 0.622(0.304~1.273) | 0.194 |
| SES高分组 | 8种 | 7 | 2.34 | 0.255(0.110~0.588) | 0.001 | 0.348(0.150~0.810) | 0.014 | 0.382(0.163~0.894) | 0.027 |
| SES高分组 | ≥9种 | 6 | 1.75 | 0.174(0.071~0.424) | <0.001 | 0.272(0.109~0.674) | 0.005 | 0.298(0.119~0.748) | 0.010 |
表5 SES、HL对CVD发病的COX比例风险回归模型分析
Table 5 COX regression analysis of SES and healthy lifestyle on CVD onset
| SES分组 | HL分组 | 新发病数(人) | 发病密度(/1 000人年) | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P值 | HR(95%CI) | P值 | HR(95%CI) | P值 | ||||
| SES低分组 | ≤6种 | 26 | 6.69 | 1.000 | — | 1.000 | — | 1.000 | — |
| SES低分组 | 7种 | 27 | 8.09 | 1.138(0.664~1.950) | 0.638 | 1.244(0.721~2.146) | 0.432 | 1.295(0.746~2.250) | 0.359 |
| SES低分组 | 8种 | 12 | 3.56 | 0.468(0.236~0.927) | 0.030 | 0.543(0.271~1.086) | 0.084 | 0.564(0.281~1.134) | 0.108 |
| SES低分组 | ≥9种 | 13 | 3.37 | 0.408(0.210~0.795) | 0.008 | 0.512(0.257~1.018) | 0.056 | 0.560(0.278~1.129) | 0.105 |
| SES高分组 | ≤6种 | 21 | 3.70 | 0.509(0.287~0.906) | 0.022 | 0.643(0.358~1.156) | 0.140 | 0.683(0.378~1.235) | 0.208 |
| SES高分组 | 7种 | 11 | 3.42 | 0.404(0.199~0.819) | 0.012 | 0.554(0.272~1.131) | 0.105 | 0.622(0.304~1.273) | 0.194 |
| SES高分组 | 8种 | 7 | 2.34 | 0.255(0.110~0.588) | 0.001 | 0.348(0.150~0.810) | 0.014 | 0.382(0.163~0.894) | 0.027 |
| SES高分组 | ≥9种 | 6 | 1.75 | 0.174(0.071~0.424) | <0.001 | 0.272(0.109~0.674) | 0.005 | 0.298(0.119~0.748) | 0.010 |
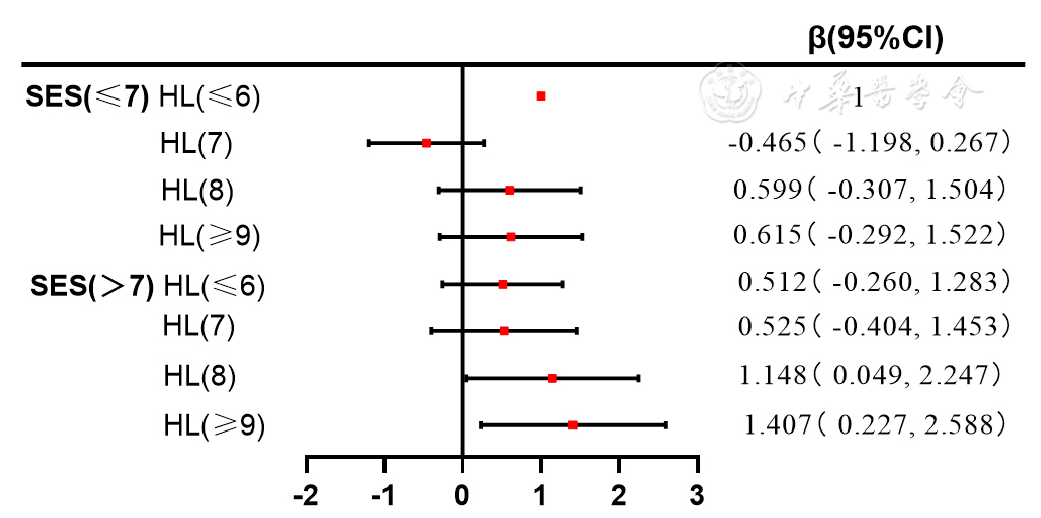
图2 SES、HL对CVD发病延迟时间分析注:SES=社会经济地位,HL=健康生活方式,MET=代谢当量;调整年龄、性别、城乡、民族、糖尿病疾病史、血脂异常、高血压疾病史、MET、BMI。
Figure 2 Analysis of the delay time of CVD onset by SES and healthy lifestyle
| [1] |
|
| [2] |
|
| [3] |
GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories,1990-2019:a systematic analysis for the Global Burden of Disease Study 2019[J]. Lancet,2020,396(10258):1223-1249. DOI:10.1016/S0140-6736(20)30752-2.
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
Non communicable diseases[EB/OL]. [2024-06-12].
|
| [21] |
|
| [22] |
|
| [23] |
|
| [24] |
|
| [25] |
|
| [26] |
|
| [27] |
|
| [28] |
|
| [29] |
|
| [30] |
|
| [31] |
|
| [32] |
|
| [33] |
|
| [34] |
|
| [35] |
|
| [36] |
|
| [37] |
|
| [1] | 曾明慧, 蒯文涛, 陈林, 韩家鑫, 徐连欣, 葛立颖, 代容容, 宓余强, 徐亮. 2型糖尿病对核苷(酸)类似物治疗慢性乙型肝炎效果的影响研究[J]. 中国全科医学, 2025, 28(35): 4414-4420. |
| [2] | 赵倬, 王贺. 缺氧诱导因子2α在心血管系统疾病中的作用机制研究进展[J]. 中国全科医学, 2025, 28(33): 4241-4248. |
| [3] | 王碧优, 高鹰, 尤俊方, 刘莉, 张卿, 苏海燕. 心血管疾病风险人群脂质比值与炎症指标的典型相关性研究[J]. 中国全科医学, 2025, 28(33): 4132-4139. |
| [4] | 陈慧龙, 廖芸楚, 刘育伟, 孔政辉, 黄兴辉, 徐嘉辉, 漆娜, 王远平, 梁文坚. 相对脂肪量与中老年人群心血管疾病之间的关联:一项基于CHARLS的横断面与纵向研究[J]. 中国全科医学, 2025, 28(32): 4047-4054. |
| [5] | 刘明波, 何新叶, 杨晓红, 王增武. 《中国心血管健康与疾病报告2024》要点解读[J]. 中国全科医学, 2025, 28(32): 3989-4008. |
| [6] | 廖姣姣, 王照宇, 李兆基, 赵威, 詹思延, 王鹏, 陶立元. 非高密度脂蛋白胆固醇动态变化对颈动脉内中膜增厚的预测价值:一项双向性队列研究[J]. 中国全科医学, 2025, 28(31): 3932-3941. |
| [7] | 张骥, 周婕, 李凌, 吴延莉, 吉维, 刘涛. 空腹血糖水平与全因死亡和特定原因死亡风险的前瞻性队列研究[J]. 中国全科医学, 2025, 28(31): 3924-3931. |
| [8] | 苏晴, 徐曜, 李一航, 汪丽燕, 蔡业峰, 倪小佳. 脑卒中及其风险人群中医证候演变规律研究的方法学质量评价[J]. 中国全科医学, 2025, 28(29): 3694-3702. |
| [9] | 邓洁, 齐祺, 吴欣雨, 韩全乐, 李雷, 蒋越, 郁静, 吴若洁, 吴寿岭, 李康博. 血浆致动脉硬化指数与体检人群新发心力衰竭风险的队列研究[J]. 中国全科医学, 2025, 28(29): 3645-3652. |
| [10] | 周晟, 邓长生, 邹冠炀, 宋健平. 疟疾心血管疾病并发症发病机制的研究进展[J]. 中国全科医学, 2025, 28(27): 3466-3472. |
| [11] | 向心月, 张冰青, 欧阳煜钦, 汤文娟, 冯文焕. 短期内科门诊减重对肥胖患者动脉粥样硬化性心血管疾病风险的影响研究[J]. 中国全科医学, 2025, 28(26): 3229-3239. |
| [12] | 丁香, 刘健, 陈晓露, 张先恒. 中草药降低类风湿关节炎合并链球菌感染患者再入院的风险:一项匹配队列研究[J]. 中国全科医学, 2025, 28(24): 3005-3012. |
| [13] | 刘银银, 隋鸿平, 李婷婷, 姜桐桐, 史铁英, 夏云龙. 乳腺癌治疗相关心脏毒性风险预测模型的研究进展[J]. 中国全科医学, 2025, 28(24): 3072-3078. |
| [14] | 杨继, 张垚, 赵英强, 张秋月. 中医三级防控模式对冠心病与脑卒中患者的管理效能评价:一项单中心前瞻性队列研究[J]. 中国全科医学, 2025, 28(22): 2750-2761. |
| [15] | 潘姚佳, 傅方琳, 韩正, 孙梦, 顾怀聪, 王为强. 肥胖类型与心血管代谢性共病的关系:基于不同性别的中年居民[J]. 中国全科医学, 2025, 28(18): 2285-2293. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





