中国全科医学 ›› 2024, Vol. 27 ›› Issue (35): 4426-4434.DOI: 10.12114/j.issn.1007-9572.2024.0256
檀紫瑞1, 申青2, 刘俊英1, 陈砚凝1, 姚继方1,*( )
)
收稿日期:2024-05-10
修回日期:2024-08-06
出版日期:2024-12-15
发布日期:2024-09-13
通讯作者:
姚继方
檀紫瑞和申青为共同第一作者
作者贡献:
檀紫瑞和申青负责论文的构思与设计、资料收集与整理、统计分析、初稿撰写、论文修改;刘俊英负责论文设计与修订;陈砚凝负责论文设计与指导;姚继方负责论文设计与修订,质量控制及审校,对文章整体负责。
基金资助:
TAN Zirui1, SHEN Qing2, LIU Junying1, CHEN Yanning1, YAO Jifang1,*( )
)
Received:2024-05-10
Revised:2024-08-06
Published:2024-12-15
Online:2024-09-13
Contact:
YAO Jifang
About author:TAN Zirui and SHEN Qing are co-first authors
摘要: 背景 表皮生长因子受体酪氨酸激酶抑制剂(EGFR-TKIs)是晚期表皮生长因子受体(EGFR)突变型非小细胞肺癌(NSCLC)患者个体化靶向治疗方案之一,可显著改善患者的预后。然而不同类型EGFR的突变对EGFR-TKIs治疗的反应不同。 目的 比较EGFR非热点突变型NSCLC一线应用EGFR-TKIs及化疗的疗效。 方法 选取2012年4月—2019年6月在河北医科大学第四医院接受治疗的术后复发或晚期NSCLC患者,并确认为EGFR非热点突变型患者共90例。以患者一线治疗方案将患者分为一线EGFR-TKIs治疗组和一线化疗组。收集患者的一般资料及EGFR基因突变情况。所有患者通过电话进行随访或复查住院及门诊病例获得患者预后情况,随访截止时间为2024-03-31。观察并比较患者疗效及无进展生存期(PFS)和总生存期(OS)。 结果 90例患者中一线EGFR-TKIs治疗组52例,一线化疗组38例。术后复发转移患者16例,初诊分期为ⅢB~Ⅳ期患者74例。EGFR非热点突变患者中,单基因突变51例,复合突变39例。一线EGFR-TKIs治疗进展后二线EGFR-TKIs治疗患者8例,二线化疗患者9例。一线化疗进展后二线EGFR-TKIs治疗患者8例,二线化疗患者16例,免疫治疗患者1例。EGFR非热点突变不同亚型接受一线EGFR-TKIs治疗的患者PFS比较,差异有统计学意义(χ2=24.26,P<0.001)。一线EGFR-TKIs治疗组与一线化疗组的PFS、OS比较,差异有统计学意义(P<0.05)。在单突变亚型患者中,一线EGFR-TKIs治疗组与一线化疗组的PFS、OS比较,差异有统计学意义(P<0.05)。在复合位点突变患者中,一线EGFR-TKIs治疗组与一线化疗组的PFS比较,差异有统计学意义(P<0.05);一线EGFR-TKIs治疗组与一线化疗组的OS比较,差异无统计学意义(P>0.05)。在一线化疗进展后的患者中,二线EGFR-TKIs治疗(8例)与化疗(16例)的中位PFS分别为11.3个月和5.6个月,二线EGFR-TKIs治疗与化疗患者PFS比较,差异有统计学意义(χ2=7.487,P=0.006)。 结论 在EGFR非热点突变型术后复发或晚期NSCLC中,EGFR ex20ins和E20 S768I突变患者与其他突变类型患者接受一线EGFR-TKIs治疗后的生存期存在差异。而在各突变亚型中,与一线化疗相比,一线EGFR-TKIs治疗均明显延长了患者的生存时间。
| 项目 | 例数(n=90) | 一线EGFR-TKIs治疗组(n=52) | 一线化疗组(n=38) |
|---|---|---|---|
| 年龄(岁) | |||
| ≥60 | 54 | 31 | 23 |
| <60 | 36 | 21 | 15 |
| 性别 | |||
| 女 | 49 | 32 | 17 |
| 男 | 41 | 20 | 21 |
| 吸烟史 | |||
| 无 | 62 | 38 | 24 |
| 有 | 28 | 14 | 14 |
| 诊断时临床分期(期) | |||
| Ⅰ | 2 | 1 | 1 |
| Ⅱ | 5 | 4 | 1 |
| ⅢA | 9 | 6 | 3 |
| ⅢB~ⅢC | 7 | 1 | 6 |
| Ⅳ | 67 | 40 | 27 |
| 疾病程度 | |||
| 复发或转移 | 16 | 11 | 5 |
| 晚期 | 74 | 41 | 33 |
| 远处转移 | |||
| 是 | 70 | 41 | 29 |
| 否 | 20 | 11 | 9 |
| 病理分型 | |||
| 腺癌 | 87 | 50 | 37 |
| 鳞状细胞癌 | 2 | 1 | 1 |
| 腺鳞癌 | 1 | 1 | 0 |
| 突变类型 | |||
| 单突变 | 51 | 20 | 31 |
| Exon 18 G719X | 18 | 9 | 9 |
| Exon 21 L861Q | 10 | 6 | 4 |
| Exon 20 S768I | 4 | 2 | 2 |
| Exon 20 insertion | 18 | 2 | 16 |
| Exon 20 T790M | 1 | 1 | 0 |
| 复合突变 | 39 | 32 | 7 |
| E18 G719X+E20 S768I | 15 | 11 | 4 |
| E18 G719X+E19 del | 1 | 1 | 0 |
| E21 L703V+E21 L858R+E20 G796A | 1 | 1 | 0 |
| E18 G719X+E21 L861Q | 2 | 1 | 1 |
| EGFR ex20ins+E19 del | 1 | 1 | 0 |
| E20 S768I+E21 L858R | 3 | 3 | 0 |
| E20 T790M+E19 del | 1 | 1 | 0 |
| E20 T790M+E21 L858R | 9 | 8 | 1 |
| E21 L861Q+E19 del | 1 | 1 | 0 |
| E21 L844V+E21 L858R | 1 | 1 | 0 |
| E21 L861Q+E21 L833F | 1 | 1 | 0 |
| E21 L861Q+E21 R832H | 1 | 1 | 0 |
| E21 L833V+E21 H835L | 1 | 0 | 1 |
| E21 L861Q+E21 L858Q | 1 | 1 | 0 |
| 治疗方式 | |||
| 一线治疗方式 | 90 | 52 | 38 |
| Gefitinib | 13 | 13 | |
| Erlotinib | 3 | 3 | |
| Icotinib | 15 | 15 | |
| Afatinib | 12 | 12 | |
| Osimertinib | 9 | 9 | |
| 化疗 | 38 | 38 | |
| 二线治疗方式 | 42 | 17 | 25 |
| Gefitinib | 3 | 1 | 2 |
| Erlotinib | 4 | 4 | |
| Icotinib | 2 | 2 | |
| Afatinib | 2 | 2 | |
| Osimertinib | 5 | 5 | |
| 化疗 | 25 | 9 | 16 |
| 免疫治疗 | 1 | 1 |
表1 90例接受一线治疗患者的分组情况(例)
Table 1 Grouping of 90 patients receiving first-line treatment
| 项目 | 例数(n=90) | 一线EGFR-TKIs治疗组(n=52) | 一线化疗组(n=38) |
|---|---|---|---|
| 年龄(岁) | |||
| ≥60 | 54 | 31 | 23 |
| <60 | 36 | 21 | 15 |
| 性别 | |||
| 女 | 49 | 32 | 17 |
| 男 | 41 | 20 | 21 |
| 吸烟史 | |||
| 无 | 62 | 38 | 24 |
| 有 | 28 | 14 | 14 |
| 诊断时临床分期(期) | |||
| Ⅰ | 2 | 1 | 1 |
| Ⅱ | 5 | 4 | 1 |
| ⅢA | 9 | 6 | 3 |
| ⅢB~ⅢC | 7 | 1 | 6 |
| Ⅳ | 67 | 40 | 27 |
| 疾病程度 | |||
| 复发或转移 | 16 | 11 | 5 |
| 晚期 | 74 | 41 | 33 |
| 远处转移 | |||
| 是 | 70 | 41 | 29 |
| 否 | 20 | 11 | 9 |
| 病理分型 | |||
| 腺癌 | 87 | 50 | 37 |
| 鳞状细胞癌 | 2 | 1 | 1 |
| 腺鳞癌 | 1 | 1 | 0 |
| 突变类型 | |||
| 单突变 | 51 | 20 | 31 |
| Exon 18 G719X | 18 | 9 | 9 |
| Exon 21 L861Q | 10 | 6 | 4 |
| Exon 20 S768I | 4 | 2 | 2 |
| Exon 20 insertion | 18 | 2 | 16 |
| Exon 20 T790M | 1 | 1 | 0 |
| 复合突变 | 39 | 32 | 7 |
| E18 G719X+E20 S768I | 15 | 11 | 4 |
| E18 G719X+E19 del | 1 | 1 | 0 |
| E21 L703V+E21 L858R+E20 G796A | 1 | 1 | 0 |
| E18 G719X+E21 L861Q | 2 | 1 | 1 |
| EGFR ex20ins+E19 del | 1 | 1 | 0 |
| E20 S768I+E21 L858R | 3 | 3 | 0 |
| E20 T790M+E19 del | 1 | 1 | 0 |
| E20 T790M+E21 L858R | 9 | 8 | 1 |
| E21 L861Q+E19 del | 1 | 1 | 0 |
| E21 L844V+E21 L858R | 1 | 1 | 0 |
| E21 L861Q+E21 L833F | 1 | 1 | 0 |
| E21 L861Q+E21 R832H | 1 | 1 | 0 |
| E21 L833V+E21 H835L | 1 | 0 | 1 |
| E21 L861Q+E21 L858Q | 1 | 1 | 0 |
| 治疗方式 | |||
| 一线治疗方式 | 90 | 52 | 38 |
| Gefitinib | 13 | 13 | |
| Erlotinib | 3 | 3 | |
| Icotinib | 15 | 15 | |
| Afatinib | 12 | 12 | |
| Osimertinib | 9 | 9 | |
| 化疗 | 38 | 38 | |
| 二线治疗方式 | 42 | 17 | 25 |
| Gefitinib | 3 | 1 | 2 |
| Erlotinib | 4 | 4 | |
| Icotinib | 2 | 2 | |
| Afatinib | 2 | 2 | |
| Osimertinib | 5 | 5 | |
| 化疗 | 25 | 9 | 16 |
| 免疫治疗 | 1 | 1 |
| 单突变 | 年龄(岁) | 性别 | 吸烟史 | 治疗方案 | 疗效 | PFS(月) |
|---|---|---|---|---|---|---|
| E18 G719X | 52 | 女 | 无 | Gefitinib | SD | 6.0 |
| E18 G719X | 71 | 男 | 有 | Gefitinib | PR | 28.0 |
| E18 G719X | 69 | 女 | 无 | Icotinib | PR | 15.6 |
| E18 G719X | 70 | 男 | 有 | Afatinib | PR | 8.0 |
| E18 G719X | 63 | 女 | 无 | Gefitinib | SD | 11.5 |
| E18 G719X | 54 | 男 | 有 | Afatinib | PR | 25.4 |
| E18 G719X | 66 | 女 | 无 | Gefitinib | SD | 11.7 |
| E18 G719X | 56 | 女 | 无 | Icotinib | PR | 24.0 |
| E18 G719X | 68 | 男 | 无 | Icotinib | SD | 9.6 |
| E21 L861Q | 75 | 女 | 有 | Erlotinib | SD | 13.5 |
| E21 L861Q | 81 | 女 | 有 | Erlotinib | PD | 2.5 |
| E21 L861Q | 73 | 男 | 有 | Afatinib | SD | 18.6 |
| E21 L861Q | 57 | 女 | 无 | Icotinib | SD | 20.5 |
| E21 L861Q | 53 | 女 | 无 | Gefitinib | PR | 16.0 |
| E21 L861Q | 64 | 女 | 有 | Gefitinib | PR | 3.5 |
| E20 S768I | 61 | 男 | 无 | Gefitinib | PD | 3.0 |
| E20 S768I | 67 | 男 | 有 | Icotinib | SD | 4.0 |
| EGFR ex20ins | 59 | 女 | 无 | Afatinib | PD | 3.3 |
| EGFR ex20ins | 71 | 男 | 无 | Afatinib | SD | 8.0 |
表2 接受一线EGFR-TKIs治疗的单突变患者的临床结果
Table 2 Clinical outcomes of single mutation patients receiving first-line EGFR-TKIs treatment
| 单突变 | 年龄(岁) | 性别 | 吸烟史 | 治疗方案 | 疗效 | PFS(月) |
|---|---|---|---|---|---|---|
| E18 G719X | 52 | 女 | 无 | Gefitinib | SD | 6.0 |
| E18 G719X | 71 | 男 | 有 | Gefitinib | PR | 28.0 |
| E18 G719X | 69 | 女 | 无 | Icotinib | PR | 15.6 |
| E18 G719X | 70 | 男 | 有 | Afatinib | PR | 8.0 |
| E18 G719X | 63 | 女 | 无 | Gefitinib | SD | 11.5 |
| E18 G719X | 54 | 男 | 有 | Afatinib | PR | 25.4 |
| E18 G719X | 66 | 女 | 无 | Gefitinib | SD | 11.7 |
| E18 G719X | 56 | 女 | 无 | Icotinib | PR | 24.0 |
| E18 G719X | 68 | 男 | 无 | Icotinib | SD | 9.6 |
| E21 L861Q | 75 | 女 | 有 | Erlotinib | SD | 13.5 |
| E21 L861Q | 81 | 女 | 有 | Erlotinib | PD | 2.5 |
| E21 L861Q | 73 | 男 | 有 | Afatinib | SD | 18.6 |
| E21 L861Q | 57 | 女 | 无 | Icotinib | SD | 20.5 |
| E21 L861Q | 53 | 女 | 无 | Gefitinib | PR | 16.0 |
| E21 L861Q | 64 | 女 | 有 | Gefitinib | PR | 3.5 |
| E20 S768I | 61 | 男 | 无 | Gefitinib | PD | 3.0 |
| E20 S768I | 67 | 男 | 有 | Icotinib | SD | 4.0 |
| EGFR ex20ins | 59 | 女 | 无 | Afatinib | PD | 3.3 |
| EGFR ex20ins | 71 | 男 | 无 | Afatinib | SD | 8.0 |
| 复合突变 | 年龄(岁) | 性别 | 吸烟史 | 治疗方案 | 疗效 | PFS(月) |
|---|---|---|---|---|---|---|
| E18 G719X+E20 S768I | 60 | 女 | 无 | Icotinib | PR | 40.0 |
| E18 G719X+E20 S768I | 52 | 男 | 有 | Icotinib | SD | 17.0 |
| E18 G719X+E20 S768I | 49 | 女 | 无 | Gefitinib | PR | 10.0 |
| E18 G719X+E20 S768I | 64 | 女 | 无 | Afatinib | SD | 14.3 |
| E18 G719X+E20 S768I | 75 | 女 | 无 | Afatinib | PR | 17.6 |
| E18 G719X+E20 S768I | 53 | 女 | 无 | Afatinib | PR | 19.8 |
| E18 G719X+E20 S768I | 53 | 男 | 有 | Icotinib | PR | 16.2 |
| E18 G719X+E20 S768I | 64 | 女 | 无 | Icotinib | SD | 11.5 |
| E18 G719X+E20 S768I | 61 | 男 | 有 | Erlotinib | SD | 5.0 |
| E18 G719X+E20 S768I | 59 | 男 | 有 | Icotinib | PR | 30.5 |
| E18 G719X+E20 S768I | 68 | 男 | 有 | Afatinib | SD | 8.2 |
| E20 S768I+E21 L858R | 56 | 女 | 无 | Afatinib | PR | 20.5 |
| E20 S768I+E21 L858R | 63 | 女 | 无 | Icotinib | PR | 22.0 |
| E20 S768I+E21 L858R | 70 | 女 | 无 | Icotinib | PR | 14.0 |
| E18 G719X+E19 del | 51 | 女 | 无 | Gefitinib | PR | 6.5 |
| E18 G719X+E21 L861Q | 48 | 男 | 有 | Icotinib | PR | 12.0 |
| EGFR ex20ins+E19 del | 58 | 男 | 无 | Gefitinib | SD | 22.4 |
| E21 L844V+E21 L858R | 62 | 女 | 无 | Icotinib | SD | 19.3 |
| E21 L861Q+E21 L833F | 61 | 女 | 无 | Afatinib | SD | 12.2 |
| E21 L861Q+E19 del | 72 | 女 | 无 | Gefitinib | PD | 2.5 |
| E21 L861Q+E21 L858Q | 68 | 男 | 有 | Gefitinib | SD | 14.0 |
| E21 L861Q+E21 R832H | 55 | 女 | 无 | Gefitinib | SD | 9.5 |
| E21 L703V+E21 L858R+E20 G796A | 55 | 女 | 无 | Afatinib | SD | 20.2 |
表3 接受一线EGFR-TKIs治疗的复合突变患者的临床结果
Table 3 Clinical outcomes of compound mutation patients receiving first-line EGFR-TKIs treatment
| 复合突变 | 年龄(岁) | 性别 | 吸烟史 | 治疗方案 | 疗效 | PFS(月) |
|---|---|---|---|---|---|---|
| E18 G719X+E20 S768I | 60 | 女 | 无 | Icotinib | PR | 40.0 |
| E18 G719X+E20 S768I | 52 | 男 | 有 | Icotinib | SD | 17.0 |
| E18 G719X+E20 S768I | 49 | 女 | 无 | Gefitinib | PR | 10.0 |
| E18 G719X+E20 S768I | 64 | 女 | 无 | Afatinib | SD | 14.3 |
| E18 G719X+E20 S768I | 75 | 女 | 无 | Afatinib | PR | 17.6 |
| E18 G719X+E20 S768I | 53 | 女 | 无 | Afatinib | PR | 19.8 |
| E18 G719X+E20 S768I | 53 | 男 | 有 | Icotinib | PR | 16.2 |
| E18 G719X+E20 S768I | 64 | 女 | 无 | Icotinib | SD | 11.5 |
| E18 G719X+E20 S768I | 61 | 男 | 有 | Erlotinib | SD | 5.0 |
| E18 G719X+E20 S768I | 59 | 男 | 有 | Icotinib | PR | 30.5 |
| E18 G719X+E20 S768I | 68 | 男 | 有 | Afatinib | SD | 8.2 |
| E20 S768I+E21 L858R | 56 | 女 | 无 | Afatinib | PR | 20.5 |
| E20 S768I+E21 L858R | 63 | 女 | 无 | Icotinib | PR | 22.0 |
| E20 S768I+E21 L858R | 70 | 女 | 无 | Icotinib | PR | 14.0 |
| E18 G719X+E19 del | 51 | 女 | 无 | Gefitinib | PR | 6.5 |
| E18 G719X+E21 L861Q | 48 | 男 | 有 | Icotinib | PR | 12.0 |
| EGFR ex20ins+E19 del | 58 | 男 | 无 | Gefitinib | SD | 22.4 |
| E21 L844V+E21 L858R | 62 | 女 | 无 | Icotinib | SD | 19.3 |
| E21 L861Q+E21 L833F | 61 | 女 | 无 | Afatinib | SD | 12.2 |
| E21 L861Q+E19 del | 72 | 女 | 无 | Gefitinib | PD | 2.5 |
| E21 L861Q+E21 L858Q | 68 | 男 | 有 | Gefitinib | SD | 14.0 |
| E21 L861Q+E21 R832H | 55 | 女 | 无 | Gefitinib | SD | 9.5 |
| E21 L703V+E21 L858R+E20 G796A | 55 | 女 | 无 | Afatinib | SD | 20.2 |
| 原发T790M | 年龄(岁) | 性别 | 吸烟史 | 治疗方案 | 疗效 | PFS(月) |
|---|---|---|---|---|---|---|
| E20 T790M+E19 del | 46 | 女 | 无 | Osimertinib | PR | 23.3 |
| E20 T790M+E21 L858R | 67 | 男 | 有 | Icotinib | SD | 2.5 |
| E20 T790M+E21 L858R | 64 | 男 | 有 | Osimertinib | SD | 23.5 |
| E20 T790M+E21 L858R | 45 | 男 | 有 | Osimertinib | PR | 17.4 |
| E20 T790M+E21 L858R | 64 | 女 | 无 | Osimertinib | PR | 11.0 |
| E20 T790M+E21 L858R | 63 | 女 | 无 | Osimertinib | SD | 11.5 |
| E20 T790M+E21 L858R | 40 | 女 | 无 | Osimertinib | SD | 7.7 |
| E20 T790M+E21 L858R | 72 | 女 | 无 | Osimertinib | PR | 8.8 |
| E20 T790M+E21 L858R | 51 | 男 | 有 | Osimertinib | SD | 17.5 |
| E20 T790M | 53 | 女 | 无 | Osimertinib | SD | 15.0 |
表4 接受一线EGFR-TKIs治疗的原发性T790M突变患者的临床结果
Table 4 Clinical outcomes of primary T790M mutation patients receiving first-line EGFR-TKIs treatment
| 原发T790M | 年龄(岁) | 性别 | 吸烟史 | 治疗方案 | 疗效 | PFS(月) |
|---|---|---|---|---|---|---|
| E20 T790M+E19 del | 46 | 女 | 无 | Osimertinib | PR | 23.3 |
| E20 T790M+E21 L858R | 67 | 男 | 有 | Icotinib | SD | 2.5 |
| E20 T790M+E21 L858R | 64 | 男 | 有 | Osimertinib | SD | 23.5 |
| E20 T790M+E21 L858R | 45 | 男 | 有 | Osimertinib | PR | 17.4 |
| E20 T790M+E21 L858R | 64 | 女 | 无 | Osimertinib | PR | 11.0 |
| E20 T790M+E21 L858R | 63 | 女 | 无 | Osimertinib | SD | 11.5 |
| E20 T790M+E21 L858R | 40 | 女 | 无 | Osimertinib | SD | 7.7 |
| E20 T790M+E21 L858R | 72 | 女 | 无 | Osimertinib | PR | 8.8 |
| E20 T790M+E21 L858R | 51 | 男 | 有 | Osimertinib | SD | 17.5 |
| E20 T790M | 53 | 女 | 无 | Osimertinib | SD | 15.0 |

图2 一线EGFR-TKIs治疗组与一线化疗组PFS和OS曲线注:A表示无进展生存期(PFS),B表示总生存期(OS);EGFR-TKIs=表皮生长因子受体酪氨酸激酶抑制剂。
Figure 2 PFS and OS curves between first-line EGFR-TKIs treatment group and first-line chemotherapy group

图3 单突变患者中一线EGFR-TKIs治疗组与一线化疗组PFS和OS曲线注:A表示PFS,B表示OS。
Figure 3 PFS and OS curves between first-line EGFR-TKIs group and first-line chemotherapy group in patients with single mutation

图4 复合突变患者中一线EGFR-TKIs治疗组与一线化疗组PFS和OS曲线注:A表示PFS,B表示OS。
Figure 4 PFS and OS curves between first-line EGFR-TKIs treatment group and first-line chemotherapy group in patients with compound mutations
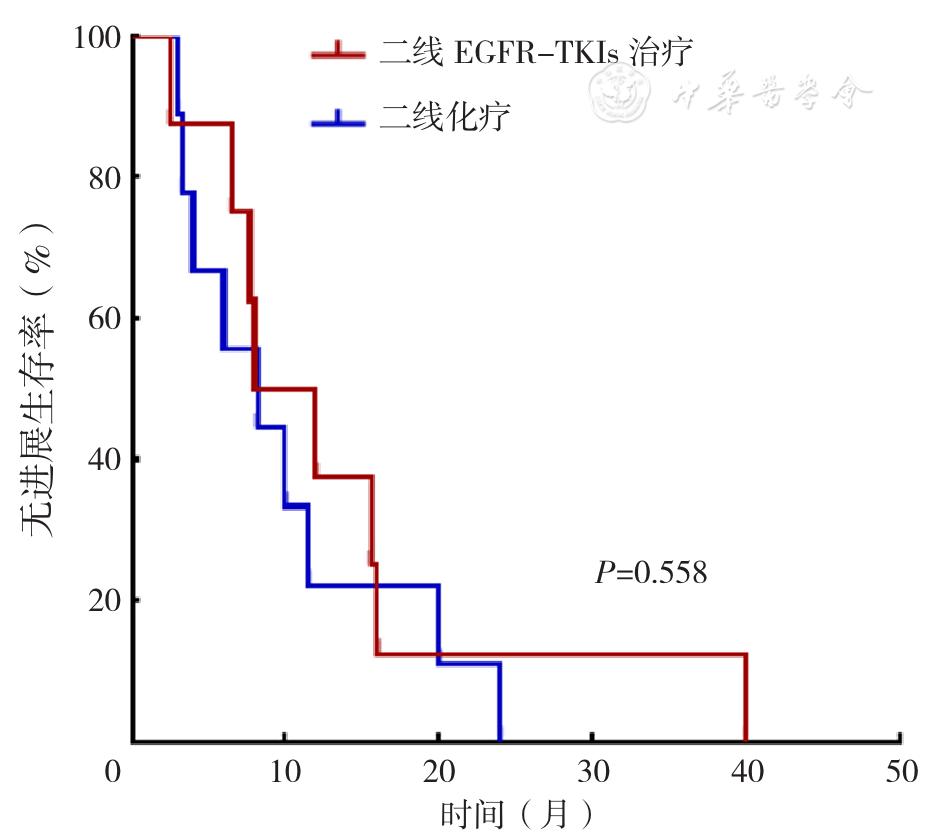
图5 一线EGFR-TKIs治疗进展后二线EGFR-TKIs治疗与化疗患者PFS曲线
Figure 5 PFS curves between second-line EGFR-TKIs treatment and chemotherapy patients after progression in first-line EGFR-TKIs treatment
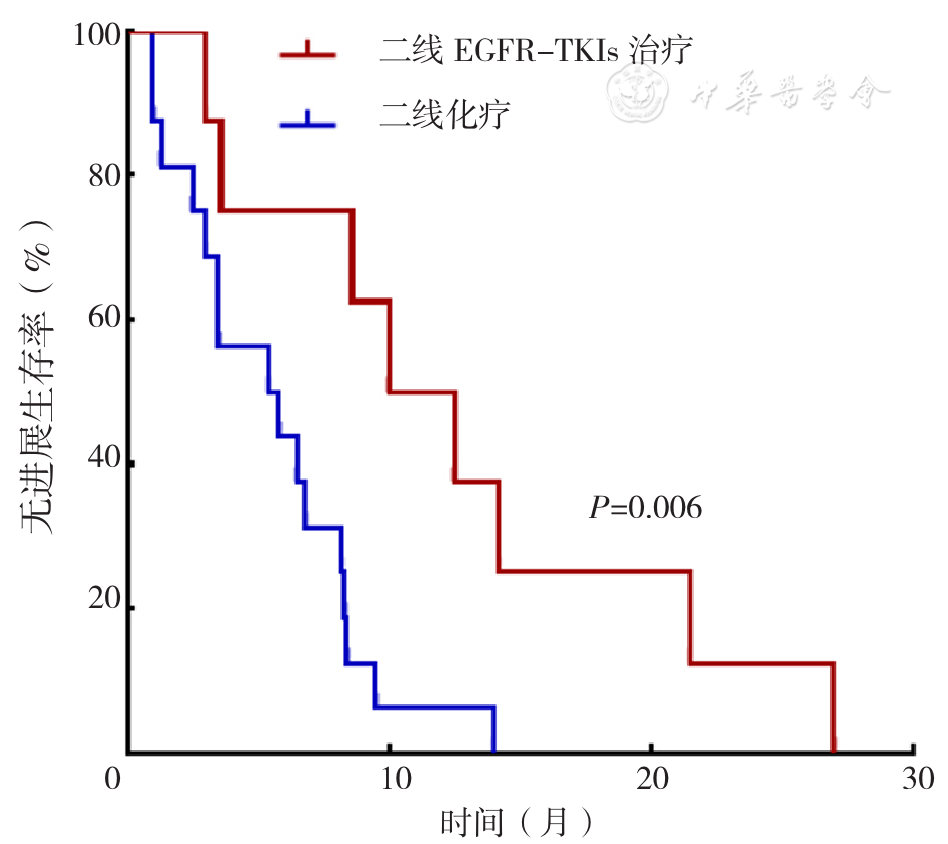
图6 一线化疗进展后二线EGFR-TKIs治疗与化疗患者PFS曲线
Figure 6 PFS curves between second-line EGFR-TKIs treatment and chemotherapy patients after first-line chemotherapy progression
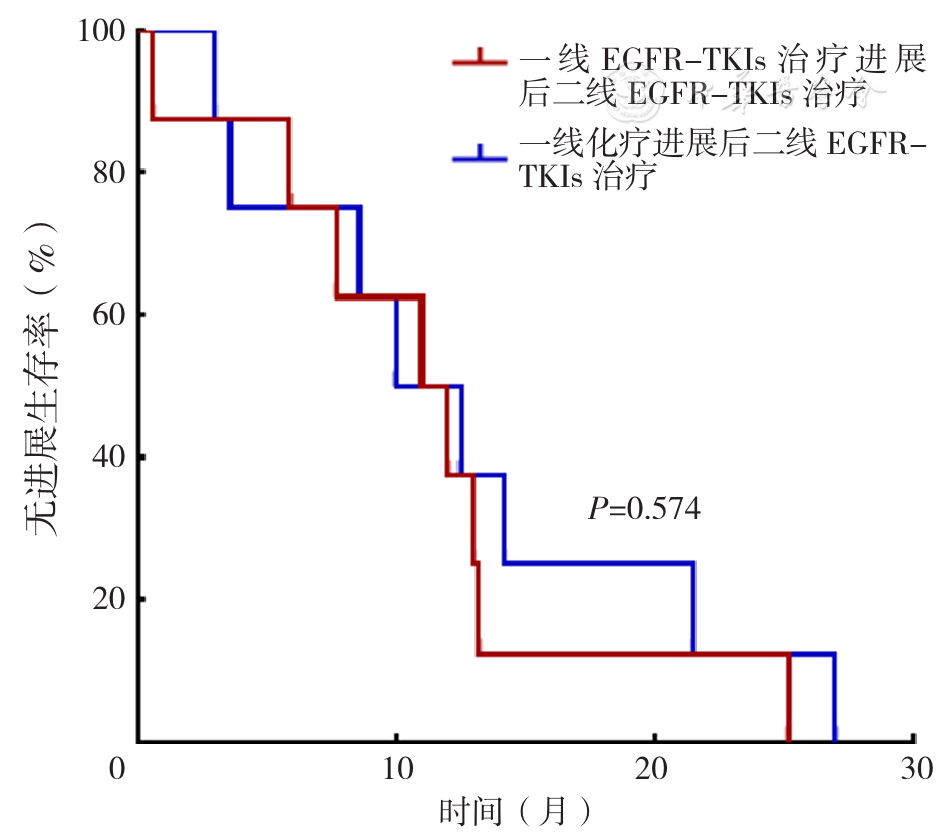
图7 一线EGFR-TKIs治疗与一线化疗进展后应用二线EGFR-TKIs治疗患者PFS曲线
Figure 7 PFS curves of patients treated with second-line EGFR-TKIs treatment between progression of first-line EGFR-TKIs treatment and chemotherapy
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [21] |
|
| [22] |
|
| [23] |
|
| [24] |
|
| [25] |
|
| [26] |
|
| [27] |
|
| [28] |
|
| [29] |
|
| [10] |
|
| [11] |
|
| [30] |
|
| [31] |
|
| [32] |
|
| [33] |
|
| [1] | 肖华, 王云芸, 王益, 董林, 常聪, 卢家春, 呼永河, 王文春. 青鹏软膏超声波导入对膝关节军事训练伤的疗效研究[J]. 中国全科医学, 2024, 27(32): 4014-4020. |
| [2] | 王秋琴, 章雨桐, 徐语晨, 柏亚妹, 陈华, 姜荣荣, 严姝霞, 王庆, 徐桂华, 谢颖, 乔春, 杨娟. 刮痧联合药物治疗原发性帕金森病的短期临床疗效研究[J]. 中国全科医学, 2023, 26(17): 2155-2161. |
| [3] | 田茂生, 高记华, 许建成, 戚文月, 王琳月, 高策. 贻贝粘蛋白联合痛痒消洗剂治疗Ⅰ度和Ⅱ度混合痔的临床疗效研究[J]. 中国全科医学, 2023, 26(08): 955-962. |
| [4] | 胡书威, 欧薇, 王智, 彭娟. 眼动脱敏与再加工和舍曲林治疗伴童年创伤的青少年抑郁症的效果比较[J]. 中国全科医学, 2023, 26(06): 692-698. |
| [5] | 曾媛, 王国华, 杨勇. 氢吗啡酮、舒芬太尼及吗啡在难治性癌痛合并口服困难患者静脉自控镇痛中的疗效比较研究[J]. 中国全科医学, 2022, 25(36): 4537-4545. |
| [6] | 杨涵雯, 王耀献, 吴巧茹, 张佳乐, 闫润泽, 王晓娜, 王珍, 孙卫卫. 泄浊消癥法治疗晚期糖尿病肾脏病的临床研究[J]. 中国全科医学, 2022, 25(26): 3252-3257. |
| [7] | 李勇, 龙勇, 赵冲, 张冠卿, 苏彦河. EGFR-TKIs联合抗血管生成药物治疗晚期EGFR突变型非小细胞肺癌患者疗效的Meta分析[J]. 中国全科医学, 2022, 25(08): 1007-1013. |
| [8] | 王欢英,许望梅,吴英,孙惠芬,李凡. 射流压力雾化泵临床雾化效果对比研究[J]. 中国全科医学, 2020, 23(12): 1508-1512. |
| [9] | 田阡陌,卢文,朱礼刚,白昕予,匡薇薇,任虹,吴园园. 基于面部不同埋线方法的综合针灸疗法治疗女性青春期后痤疮的疗效及其作用机制[J]. 中国全科医学, 2019, 22(9): 1068-1073. |
| [10] | 汪登亮,康权,王浩名,戴小科,张明满. 超声引导下新型水灌肠仪器灌肠与传统空气灌肠治疗小儿肠套叠的有效性及安全性研究[J]. 中国全科医学, 2019, 22(6): 712-714. |
| [11] | 洪秋阳,杨惠民,赵吉平,王世广,姚金,杨怡. 火针五脏俞加膈俞配合毫针治疗慢性失眠症临床疗效观察[J]. 中国全科医学, 2019, 22(3): 336-340. |
| [12] | 赵红波,吴晓晶,杨云,葛志明. “温中厚肠”法治疗腹泻型肠易激综合征临床疗效评价[J]. 中国全科医学, 2019, 22(25): 3137-3143. |
| [13] | 钟远鸣,李嘉琅,李智斐,张翼升,陈震,廖俊城. 不同浓度臭氧联合射频消融术治疗神经根型颈椎病的疗效对比研究[J]. 中国全科医学, 2019, 22(24): 2924-2928. |
| [14] | 李伟学,田宋君,詹争明,林先盛. Stretta射频治疗与toupet胃底折叠术对胃食管反流病的疗效比较研究[J]. 中国全科医学, 2019, 22(18): 2200-2205. |
| [15] | 姜笑明,陈润浩,黄文海,俞建平,张华云. 腹腔镜阑尾切除术两种阑尾残端处理方法的前瞻性对比研究[J]. 中国全科医学, 2018, 21(6): 712-714. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





