中国全科医学 ›› 2025, Vol. 28 ›› Issue (22): 2740-2749.DOI: 10.12114/j.issn.1007-9572.2023.0748
陈飞1, 王金英2, 于海搏1, 李新1, 张佳佳1, 申曼1, 詹晓凯1, 汤然1, 范斯斌1, 赵凤仪1, 张天宇1, 黄仲夏1,*( )
)
收稿日期:2024-12-10
修回日期:2025-07-01
出版日期:2025-08-05
发布日期:2025-06-30
通讯作者:
黄仲夏
陈飞和王金英为共同第一作者
作者贡献:
陈飞、王金英负责患者选取与样本采集,并进行试验分析、总结与撰写论文;于海搏、李新、张佳佳、申曼、詹晓凯、汤然、范斯斌、赵凤仪、张天宇协助数据收集与整理、图表绘制与展示;黄仲夏指导选题和设计、负责文章质量控制,对文章整体负责。
基金资助:
CHEN Fei1, WANG Jinying2, YU Haibo1, LI Xin1, ZHANG Jiajia1, SHEN Man1, ZHAN Xiaokai1, TANG Ran1, FAN Sibin1, ZHAO Fengyi1, ZHANG Tianyu1, HUANG Zhongxia1,*( )
)
Received:2024-12-10
Revised:2025-07-01
Published:2025-08-05
Online:2025-06-30
Contact:
HUANG Zhongxia
About author:CHEN Fei and WANG Jinying are co-first authors
摘要: 背景 多发性骨髓瘤(MM)是一种恶性浆细胞病,近半数患者在就诊时存在MM相关肾损害(KI),与患者死亡率增加有关。早期识别和治疗KI,有可能逆转肾功能,改善患者生存状况。中性粒细胞明胶酶相关运载蛋白(NGAL)、T细胞免疫球蛋白粘蛋白受体1(TIM-1)、血管细胞黏附分子-1(VCAM-1)和激活素A与细胞增殖、侵袭和KI等病理过程相关。上述指标有希望成为MM相关KI早期诊断的指标。 目的 探讨新型生物标志物NGAL、TIM-1、VCAM-1和激活素A在新诊断MM(NDMM)合并KI的病情演变、分期和预后中的意义。 方法 选取2017年1月—2022年2月首都医科大学附属北京朝阳医院石景山院区血液科住院的70例NDMM患者,包括62例症状性MM和8例冒烟型MM(SMM);同时纳入12例意义未明单克隆丙种球蛋白血症(MGUS)患者、7例肾脏意义的单克隆免疫球蛋白血症(MGRS)患者及20例健康对照(HC)。收集纳入者的临床资料及MGUS、MGRS、NDMM患者骨髓穿刺活检、M蛋白检查、影像学检查结果;应用酶联免疫吸附法检测尿NGAL(uNGAL)、尿TIM-1(uTIM-1)、血清TIM-1(sTIM-1)、尿VCAM-1(uVCAM-1)、尿激活素A水平。根据疾病状态将研究对象分为MGUS组、MGRS组、NDMM组和HC组,根据KI情况将患者分为MGUS组、MGRS组、KI组和非肾损伤(NKI)组,KI组依据动态疾病治疗状态分为治疗前MM亚组、治疗后达到部分治疗反应(PR)以上(>PR)亚组、复发MM亚组。各指标的相关性采用Spearman秩相关分析,绘制受试者工作特征(ROC)曲线以分析各指标对NDMM合并KI的诊断价值,计算最佳截断值;依据各指标的最佳截断值分为高于最佳截断值组及低于最佳截断值组,采用Kaplan-Meier方法分析各指标在高于最佳截断值组和低于最佳截断值组的总生存期(OS);并采用COX比例风险回归分析NDMM合并KI患者全因死亡的影响因素。 结果 NDMM组的uNGAL、uTIM-1、uVCAM-1、sTIM-1和尿激活素A水平高于MGUS组和HC组(P<0.05),MGRS组的uNGAL、uTIM-1、uVCAM-1、sTIM-1和尿激活素A水平高于MGUS组(P<0.05),KI组的uNGAL、uTIM-1、uVCAM-1、sTIM-1和尿激活素A水平高于NKI组(P<0.05),治疗前MM亚组、复发MM亚组的uNGAL、uTIM-1、uVCAM-1、sTIM-1和尿激活素A水平高于>PR亚组(P<0.05)。uNGAL、uTIM-1、uVCAM-1、sTIM-1及尿激活素A与肌酐、β2-微球蛋白、R-ISS分期呈正相关(P<0.05),与估算肾小球滤过率呈负相关(P<0.05)。uNGAL、uTIM-1、sTIM-1、尿激活素A与24 h尿轻链水平呈正相关(P<0.05),uNGAL、uTIM-1与克隆性浆细胞比例呈正相关(P<0.05)。根据ROC曲线得出诊断MM相关KI的uNGAL、uTIM-1、uVCAM-1、尿激活素A最佳截断值分别为14.774 ng/mL、1.978 ng/mL、144.400 ng/mL、33.730 pg/mL。Kaplan-Meier结果显示,高于uNGAL、uTIM-1、sTIM-1、uVCAM-1、尿激活素A各自最佳截断值的患者OS更差(P<0.05);多因素COX比例风险回归分析结果显示,uNGAL、R-ISS分期是NDMM合并KI患者全因死亡的影响因素(P<0.05)。 结论 uNGAL、uTIM-1、uVCAM-1、尿激活素A可能与MM病情进展和KI有关,是肾小管损伤的早期标志物,有利于MM合并KI患者的早期诊治,且与R-ISS分期、24 h尿轻链、克隆性浆细胞比例等肿瘤负荷指标和MM患者总体生存相关。
中图分类号:
| 组别 | 例数 | 年龄[M(QR),年] | 性别[例(%)] | 异常免疫球蛋白重链类型[例(%)] | 异常免疫球蛋白轻链类型[例(%)] | 克隆性浆细胞比例[M(QR),%] | 血钙( | |||
|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | IgG | IgA | k | λ | |||||
| HC组 | 20 | 61.0(14.0) | 11(55.0) | 9(45.0) | — | — | — | — | 0(0) | 2.1±0.1 |
| MGUS组 | 12 | 69.5(13.0) | 9(75.0) | 3(25.0) | 5(41.7) | 3(25.0) | 5(41.7) | 7(58.3) | 2.6(2.0) | 2.2±0.2 |
| MGRS组 | 7 | 62.0(12.0) | 3(42.9) | 4(57.1) | 3(42.9) | 4(57.1) | 5(71.4) | 2(28.6) | 2.4(1.7) | 2.1±0.1 |
| NDMM组 | 70 | 65.0(12.0) | 41(58.5) | 29(41.4) | 23(32.9) | 22(31.4) | 43(61.4) | 27(38.6) | 28.3(33.4)abc | 2.3±0.4a |
| 检验统计量值 | 4.654 | 1.336d | 0.371d | 2.106d | 28.428 | 11.823e | ||||
| P值 | 0.199 | 0.721 | 0.831 | 0.349 | <0.001 | <0.001 | ||||
| 组别 | 血红蛋白( | β2-微球蛋白[M(QR),mg/L] | 白蛋白( | eGFR[M(QR),mL·min-1·(1.73 m2)-1] | 肌酐[M(QR),μmol/L] | sFLC[M(QR),mg/L] | sFLC k/λ [M(QR)] | 24 h尿蛋白( | 24 h尿轻链( | |
| HC组 | 131.7±5.1 | 2.6(1.2) | 38.3±4.8 | 93.7(34.4) | 74.2(19.5) | — | — | — | — | |
| MGUS组 | 138.5±9.5 | 2.9(1.2) | 40.6±3.6 | 88.60(41.2) | 77.2(26.4) | 61.3(93.0) | 4.5(14.3) | 0.1±0.1 | 0.3±0.3 | |
| MGRS组 | 115.6±26.4 b | 4.8(4.9) | 37.0±5.5 | 38.4(20.6)b | 175.0(104.6)ab | 109.8(403.0) | 3.2(13.1) | 2.6±1.7ab | 1.7±1.1 | |
| NDMM组 | 91.3±22.6 | 7.7(11.1)ab | 33.9±6.0b | 49.2(65.5)abc | 152.8(169.0)ab | 1 340.0(3 345.0)bc | 72.6(268.8)ab | 2.8±1.3bc | 7.8±6.3bc | |
| 检验统计量值 | 32.441e | 41.906 | 4.124e | 25.721 | 23.654 | 44.276 | 32.221 | 23.782e | 26.655 | |
| P值 | 0.014 | <0.001 | 0.042 | 0.014 | 0.019 | <0.001 | <0.001 | <0.001 | <0.001 | |
表1 MGUS组、MGRS组、NDMM组、HC组临床特征比较
Table 1 Comparison of clinical characteristics among HC,MGUS,MGRS and NDMM group
| 组别 | 例数 | 年龄[M(QR),年] | 性别[例(%)] | 异常免疫球蛋白重链类型[例(%)] | 异常免疫球蛋白轻链类型[例(%)] | 克隆性浆细胞比例[M(QR),%] | 血钙( | |||
|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | IgG | IgA | k | λ | |||||
| HC组 | 20 | 61.0(14.0) | 11(55.0) | 9(45.0) | — | — | — | — | 0(0) | 2.1±0.1 |
| MGUS组 | 12 | 69.5(13.0) | 9(75.0) | 3(25.0) | 5(41.7) | 3(25.0) | 5(41.7) | 7(58.3) | 2.6(2.0) | 2.2±0.2 |
| MGRS组 | 7 | 62.0(12.0) | 3(42.9) | 4(57.1) | 3(42.9) | 4(57.1) | 5(71.4) | 2(28.6) | 2.4(1.7) | 2.1±0.1 |
| NDMM组 | 70 | 65.0(12.0) | 41(58.5) | 29(41.4) | 23(32.9) | 22(31.4) | 43(61.4) | 27(38.6) | 28.3(33.4)abc | 2.3±0.4a |
| 检验统计量值 | 4.654 | 1.336d | 0.371d | 2.106d | 28.428 | 11.823e | ||||
| P值 | 0.199 | 0.721 | 0.831 | 0.349 | <0.001 | <0.001 | ||||
| 组别 | 血红蛋白( | β2-微球蛋白[M(QR),mg/L] | 白蛋白( | eGFR[M(QR),mL·min-1·(1.73 m2)-1] | 肌酐[M(QR),μmol/L] | sFLC[M(QR),mg/L] | sFLC k/λ [M(QR)] | 24 h尿蛋白( | 24 h尿轻链( | |
| HC组 | 131.7±5.1 | 2.6(1.2) | 38.3±4.8 | 93.7(34.4) | 74.2(19.5) | — | — | — | — | |
| MGUS组 | 138.5±9.5 | 2.9(1.2) | 40.6±3.6 | 88.60(41.2) | 77.2(26.4) | 61.3(93.0) | 4.5(14.3) | 0.1±0.1 | 0.3±0.3 | |
| MGRS组 | 115.6±26.4 b | 4.8(4.9) | 37.0±5.5 | 38.4(20.6)b | 175.0(104.6)ab | 109.8(403.0) | 3.2(13.1) | 2.6±1.7ab | 1.7±1.1 | |
| NDMM组 | 91.3±22.6 | 7.7(11.1)ab | 33.9±6.0b | 49.2(65.5)abc | 152.8(169.0)ab | 1 340.0(3 345.0)bc | 72.6(268.8)ab | 2.8±1.3bc | 7.8±6.3bc | |
| 检验统计量值 | 32.441e | 41.906 | 4.124e | 25.721 | 23.654 | 44.276 | 32.221 | 23.782e | 26.655 | |
| P值 | 0.014 | <0.001 | 0.042 | 0.014 | 0.019 | <0.001 | <0.001 | <0.001 | <0.001 | |
| 组别 | 例数 | 年龄[M(QR),年] | 性别[例(%)] | 异常免疫球蛋白重链类型[例(%)] | 异常免疫球蛋白轻链类型[例(%)] | 克隆性浆细胞比例[M(QR),%] | 血钙( | |||
|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | IgG | IgA | k | λ | |||||
| MGUS组 | 12 | 69.5(13.0) | 9(75.0) | 3(25.0) | 5(41.7) | 3(25.0) | 5(41.7) | 7(58.3) | 2.6(2.0) | 2.2±0.2 |
| MGRS组 | 7 | 62.0(12.0) | 3(42.9) | 4(57.1) | 3(42.9) | 4(57.1) | 5(71.4) | 2(28.6) | 2.4(1.7) | 2.1±0.1a |
| NKI组 | 30 | 64.5(8.0) | 18(60.0) | 12(40.0) | 12(40.0) | 7(23.3) | 16(53.3) | 14(46.7) | 26.4(14.1)ab | 2.4±0.3 |
| KI组 | 40 | 67.0(7.0) | 23(57.5) | 17(42.5) | 11(27.5) | 15(37.5) | 27(67.5) | 13(32.5) | 28.3(19.8)ab | 2.5±0.5b |
| 检验统计量值 | 3.745 | 1.535d | 2.285d | 3.534 | 44.515 | 7.863e | ||||
| P值 | 0.290 | 0.674 | 0.515 | 0.316 | <0.001 | 0.036 | ||||
| 组别 | 血红蛋白( | β2-微球蛋白[M(QR),mg/L] | 白蛋白( | eGFR[M(QR),mL·min-1·(1.73 m2)-1] | 肌酐[M(QR),μmol/L] | sFLC[M(QR),mg/L] | sFLC k/λ [M(QR)] | 24 h尿蛋白( | 24 h尿轻链( | |
| MGUS组 | 139±10 | 2.9(1.2) | 40.6±3.6 | 88.60(41.2) | 77.2(26.4) | 61.3(93.0) | 4.5(14.3) | 0.1±0.1 | 0.3±0.3 | |
| MGRS组 | 116±26a | 4.8(4.9) | 37.0±5.5 | 38.4(20.6)a | 175.0(104.6)a | 109.8(403.0) | 3.2(13.1) | 2.6±1.7a | 1.7±1.1 | |
| NKI组 | 104±13a | 3.8(2.3) | 34.9±5.5 | 100.4(31.6)b | 79.7(35.6)b | 312.0(775.0) | 31.6(88.4) | 1.3±0.8a | 3.4±2.0a | |
| KI组 | 82±17a | 14.5(10.3)ac | 33.1±7.0ac | 37.8(29.2)ac | 201.2(84.3)ac | 1980.0(4327.0)abc | 103.5(373.9)abc | 3.9±2.6ac | 10.9±10.1abc | |
| 检验统计量值 | 5.251e | 48.627 | 5.688e | 65.959 | 66.263 | 22.442 | 24.429 | 17.442e | 9.074e | |
| P值 | 0.039 | <0.001 | 0.038 | <0.001 | <0.001 | <0.001 | <0.001 | 0.022 | 0.028 | |
表2 MGUS组、MGRS组、NKI组、KI组基线临床特征比较
Table 2 Comparison of baseline clinical characteristics among MGUS,MGRS,NKI and KI group
| 组别 | 例数 | 年龄[M(QR),年] | 性别[例(%)] | 异常免疫球蛋白重链类型[例(%)] | 异常免疫球蛋白轻链类型[例(%)] | 克隆性浆细胞比例[M(QR),%] | 血钙( | |||
|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | IgG | IgA | k | λ | |||||
| MGUS组 | 12 | 69.5(13.0) | 9(75.0) | 3(25.0) | 5(41.7) | 3(25.0) | 5(41.7) | 7(58.3) | 2.6(2.0) | 2.2±0.2 |
| MGRS组 | 7 | 62.0(12.0) | 3(42.9) | 4(57.1) | 3(42.9) | 4(57.1) | 5(71.4) | 2(28.6) | 2.4(1.7) | 2.1±0.1a |
| NKI组 | 30 | 64.5(8.0) | 18(60.0) | 12(40.0) | 12(40.0) | 7(23.3) | 16(53.3) | 14(46.7) | 26.4(14.1)ab | 2.4±0.3 |
| KI组 | 40 | 67.0(7.0) | 23(57.5) | 17(42.5) | 11(27.5) | 15(37.5) | 27(67.5) | 13(32.5) | 28.3(19.8)ab | 2.5±0.5b |
| 检验统计量值 | 3.745 | 1.535d | 2.285d | 3.534 | 44.515 | 7.863e | ||||
| P值 | 0.290 | 0.674 | 0.515 | 0.316 | <0.001 | 0.036 | ||||
| 组别 | 血红蛋白( | β2-微球蛋白[M(QR),mg/L] | 白蛋白( | eGFR[M(QR),mL·min-1·(1.73 m2)-1] | 肌酐[M(QR),μmol/L] | sFLC[M(QR),mg/L] | sFLC k/λ [M(QR)] | 24 h尿蛋白( | 24 h尿轻链( | |
| MGUS组 | 139±10 | 2.9(1.2) | 40.6±3.6 | 88.60(41.2) | 77.2(26.4) | 61.3(93.0) | 4.5(14.3) | 0.1±0.1 | 0.3±0.3 | |
| MGRS组 | 116±26a | 4.8(4.9) | 37.0±5.5 | 38.4(20.6)a | 175.0(104.6)a | 109.8(403.0) | 3.2(13.1) | 2.6±1.7a | 1.7±1.1 | |
| NKI组 | 104±13a | 3.8(2.3) | 34.9±5.5 | 100.4(31.6)b | 79.7(35.6)b | 312.0(775.0) | 31.6(88.4) | 1.3±0.8a | 3.4±2.0a | |
| KI组 | 82±17a | 14.5(10.3)ac | 33.1±7.0ac | 37.8(29.2)ac | 201.2(84.3)ac | 1980.0(4327.0)abc | 103.5(373.9)abc | 3.9±2.6ac | 10.9±10.1abc | |
| 检验统计量值 | 5.251e | 48.627 | 5.688e | 65.959 | 66.263 | 22.442 | 24.429 | 17.442e | 9.074e | |
| P值 | 0.039 | <0.001 | 0.038 | <0.001 | <0.001 | <0.001 | <0.001 | 0.022 | 0.028 | |
| 组别 | 例数 | 年龄( | 性别[例(%)] | 免疫球蛋白重链类型[例(%)] | 免疫球蛋白轻链类型[例(%)] | 克隆性浆细胞比例[M(QR),%] | 血钙( | |||
|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | IgG | IgA | k | λ | |||||
| 治疗前MM亚组 | 20 | 58.4±10.6 | 9(45.0) | 11(55.0) | 4(20.0) | 10(50.0) | 13(65.0) | 7(35.0) | 31.4(22.3) | 2.6±0.6 |
| >PR亚组 | 20 | 58.4±10.6 | 9(45.0) | 11(55.0) | 4(20.0) | 10(50.0) | 13(65.0) | 7(35.0) | 3.6(5.2)a | 2.2±0.1a |
| 复发MM亚组 | 11 | 55.8±10.2 | 8(72.7) | 3(27.3) | 3(27.3) | 5(45.5) | 7(63.6) | 4(36.4) | 25.2(24.8)b | 2.5±0.4 b |
| 检验统计量值 | 18.683 | 4.000c | 3.196c | 3.024c | 12.484 | 3.537d | ||||
| P值 | 0.271 | 0.135 | 0.143 | 0.158 | <0.001 | 0.043 | ||||
| 组别 | 血红蛋白( | β2-微球蛋白[M(QR),mg/L] | 白蛋白( | eGFR[M(QR),mL·min-1·(1.73 m2)-1] | 肌酐[M(QR),μmol/L] | sFLC[M(QR),mg/L] | sFLC k/λ [M(QR)] | 24 h尿蛋白[M(QR),g/24 h] | 24 h尿轻链[M(QR),g/24 h] | |
| 治疗前MM亚组 | 81±14 | 13.9(13.5) | 33.4±6.9 | 38.1(22.5) | 184.2(120.3) | 1 903.5(4 420.0) | 125.6(402.2) | 2.8(4.8) | 7.5(7.4) | |
| >PR亚组 | 106±21a | 5.1(1.9)a | 37.6±3.5a | 61.8(42.1)a | 100.7(58.0)a | 66.0(635.0)a | 3.4(56.8)a | 0.2(0.4)a | 0(0.8)a | |
| 复发MM亚组 | 99±29 | 8.4(12.8)b | 34.5±5.1 | 32.8(20.6) | 180.4(123.7) | 1 111.0(6 572.0)b | 309.8(2042.7)b | 2.9(3.8)b | 4.0(12.3)b | |
| 检验统计量值 | 5.344d | 3.833 | 6.242d | 3.920 | 11.636 | 2.395 | 2.395 | 3.823 | 2.934 | |
| P值 | 0.032 | 0.043 | 0.044 | <0.001 | 0.025 | 0.038 | 0.038 | 0.028 | 0.032 | |
表3 治疗前MM亚组、>PR亚组、复发MM亚组临床特征比较
Table 3 Comparison of baseline clinical characteristics among pre-treatmnet MM、>PR and relapsed MM group
| 组别 | 例数 | 年龄( | 性别[例(%)] | 免疫球蛋白重链类型[例(%)] | 免疫球蛋白轻链类型[例(%)] | 克隆性浆细胞比例[M(QR),%] | 血钙( | |||
|---|---|---|---|---|---|---|---|---|---|---|
| 男 | 女 | IgG | IgA | k | λ | |||||
| 治疗前MM亚组 | 20 | 58.4±10.6 | 9(45.0) | 11(55.0) | 4(20.0) | 10(50.0) | 13(65.0) | 7(35.0) | 31.4(22.3) | 2.6±0.6 |
| >PR亚组 | 20 | 58.4±10.6 | 9(45.0) | 11(55.0) | 4(20.0) | 10(50.0) | 13(65.0) | 7(35.0) | 3.6(5.2)a | 2.2±0.1a |
| 复发MM亚组 | 11 | 55.8±10.2 | 8(72.7) | 3(27.3) | 3(27.3) | 5(45.5) | 7(63.6) | 4(36.4) | 25.2(24.8)b | 2.5±0.4 b |
| 检验统计量值 | 18.683 | 4.000c | 3.196c | 3.024c | 12.484 | 3.537d | ||||
| P值 | 0.271 | 0.135 | 0.143 | 0.158 | <0.001 | 0.043 | ||||
| 组别 | 血红蛋白( | β2-微球蛋白[M(QR),mg/L] | 白蛋白( | eGFR[M(QR),mL·min-1·(1.73 m2)-1] | 肌酐[M(QR),μmol/L] | sFLC[M(QR),mg/L] | sFLC k/λ [M(QR)] | 24 h尿蛋白[M(QR),g/24 h] | 24 h尿轻链[M(QR),g/24 h] | |
| 治疗前MM亚组 | 81±14 | 13.9(13.5) | 33.4±6.9 | 38.1(22.5) | 184.2(120.3) | 1 903.5(4 420.0) | 125.6(402.2) | 2.8(4.8) | 7.5(7.4) | |
| >PR亚组 | 106±21a | 5.1(1.9)a | 37.6±3.5a | 61.8(42.1)a | 100.7(58.0)a | 66.0(635.0)a | 3.4(56.8)a | 0.2(0.4)a | 0(0.8)a | |
| 复发MM亚组 | 99±29 | 8.4(12.8)b | 34.5±5.1 | 32.8(20.6) | 180.4(123.7) | 1 111.0(6 572.0)b | 309.8(2042.7)b | 2.9(3.8)b | 4.0(12.3)b | |
| 检验统计量值 | 5.344d | 3.833 | 6.242d | 3.920 | 11.636 | 2.395 | 2.395 | 3.823 | 2.934 | |
| P值 | 0.032 | 0.043 | 0.044 | <0.001 | 0.025 | 0.038 | 0.038 | 0.028 | 0.032 | |
| 组别 | 例数 | uNGAL[M(QR),ng/mL] | uTIM-1[M(QR),ng/mL] | sTIM-1[M(QR),pg/mL] | Ratio of TIM-1 [M(QR)] | uVCAM-1[M(QR),ng/mL] | 尿激活素A [M(QR),pg/mL] |
|---|---|---|---|---|---|---|---|
| HC组 | 20 | 1.5(1.2) | 0.7(0.5) | 34.8(16.4) | 0.06(0.03) | 103.7(44.7) | 18.6(12.9) |
| MGUS组 | 12 | 2.8(3.2) | 0.6(0.7) | — | — | — | — |
| MGRS组 | 7 | 35.0(19.8)ab | 1.4(0.6)a | — | — | — | — |
| NDMM组 | 70 | 14.0(39.7)a | 1.7(1.3)ab | 173.0(204.8)a | 0.10(0.06)a | 171.6(95.5)a | 33.3(23.1)a |
| 检验统计量值 | 58.494 | 64.848 | 20.948c | 23.635c | 25.541c | 30.716c | |
| P值 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
表4 HC组、MGUS组、MGRS组、NDMM组患者各检测因子水平比较
Table 4 Comparison of detective factors among HC,MGUS,MGRS and NDMM group
| 组别 | 例数 | uNGAL[M(QR),ng/mL] | uTIM-1[M(QR),ng/mL] | sTIM-1[M(QR),pg/mL] | Ratio of TIM-1 [M(QR)] | uVCAM-1[M(QR),ng/mL] | 尿激活素A [M(QR),pg/mL] |
|---|---|---|---|---|---|---|---|
| HC组 | 20 | 1.5(1.2) | 0.7(0.5) | 34.8(16.4) | 0.06(0.03) | 103.7(44.7) | 18.6(12.9) |
| MGUS组 | 12 | 2.8(3.2) | 0.6(0.7) | — | — | — | — |
| MGRS组 | 7 | 35.0(19.8)ab | 1.4(0.6)a | — | — | — | — |
| NDMM组 | 70 | 14.0(39.7)a | 1.7(1.3)ab | 173.0(204.8)a | 0.10(0.06)a | 171.6(95.5)a | 33.3(23.1)a |
| 检验统计量值 | 58.494 | 64.848 | 20.948c | 23.635c | 25.541c | 30.716c | |
| P值 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| 组别 | 例数 | uNGAL[M(QR),ng/mL] | uTIM-1[M(QR),ng/mL] | sTIM-1[M(QR),pg/mL] | Ratio of TIM-1 [M(QR)] | uVCAM-1[M(QR),ng/mL] | 尿激活素A [M(QR),pg/mL] |
|---|---|---|---|---|---|---|---|
| MGUS组 | 12 | 2.8(3.2) | 0.6(0.7) | — | — | — | — |
| MGRS组 | 7 | 35.0(19.8)a | 1.4(0.6) | — | — | — | — |
| NKI组 | 30 | 4.4(4.2)b | 1.4(0.9)a | 92.2(86.4) | 0.07(0.02) | 162.6(53.7) | 26.5(18.0) |
| KI组 | 40 | 35.4(111.4)ac | 1.9(1.3)ac | 220.9(216.0)c | 0.11(0.06)c | 232.9(129.6)c | 44.2(27.5)c |
| 检验统计量值 | 39.872 | 32.500 | 10.982 d | 6.817 d | 11.438 d | 10.221 d | |
| P值 | <0.001 | <0.001 | 0.004 | 0.005 | 0.003 | 0.004 |
表5 MGUS组、MGRS组、NKI组和KI组患者各检测因子水平比较
Table 5 Comparison of detective factors among MGUS,MGRS,NKI,KI group
| 组别 | 例数 | uNGAL[M(QR),ng/mL] | uTIM-1[M(QR),ng/mL] | sTIM-1[M(QR),pg/mL] | Ratio of TIM-1 [M(QR)] | uVCAM-1[M(QR),ng/mL] | 尿激活素A [M(QR),pg/mL] |
|---|---|---|---|---|---|---|---|
| MGUS组 | 12 | 2.8(3.2) | 0.6(0.7) | — | — | — | — |
| MGRS组 | 7 | 35.0(19.8)a | 1.4(0.6) | — | — | — | — |
| NKI组 | 30 | 4.4(4.2)b | 1.4(0.9)a | 92.2(86.4) | 0.07(0.02) | 162.6(53.7) | 26.5(18.0) |
| KI组 | 40 | 35.4(111.4)ac | 1.9(1.3)ac | 220.9(216.0)c | 0.11(0.06)c | 232.9(129.6)c | 44.2(27.5)c |
| 检验统计量值 | 39.872 | 32.500 | 10.982 d | 6.817 d | 11.438 d | 10.221 d | |
| P值 | <0.001 | <0.001 | 0.004 | 0.005 | 0.003 | 0.004 |
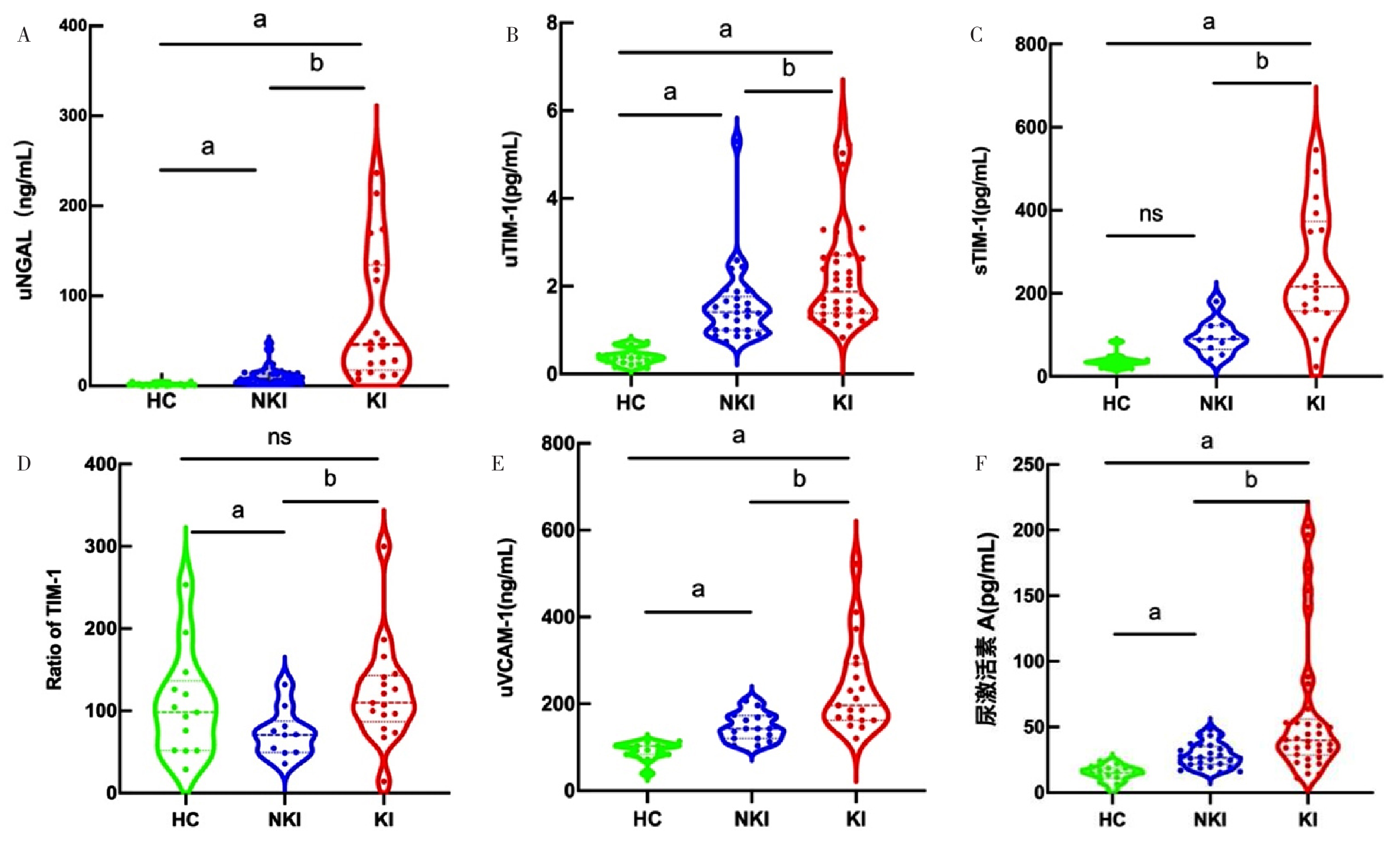
图1 HC组、NKI组、KI组各检测因子水平比较小提琴图注:HC=健康对照,KI=肾损害,NKI=非肾损伤;A为尿中性粒细胞明胶酶相关运载蛋白(uNGAL),B为尿T细胞免疫球蛋白粘蛋白受体1(uTIM-1),C为血清T细胞免疫球蛋白粘蛋白受体1(sTIM-1),D为血清与尿液中TIM-1浓度比值(Ratio of TIM-1),E为尿血管细胞黏附分子1(uVCAM-1),F为尿液激活素A;ns表示P>0.05,a表示与HC组比较P<0.05,b表示与NKI组比较P<0.05。
Figure 1 Violin plot comparing the levels of each detected factors in HC,NKI and KI group
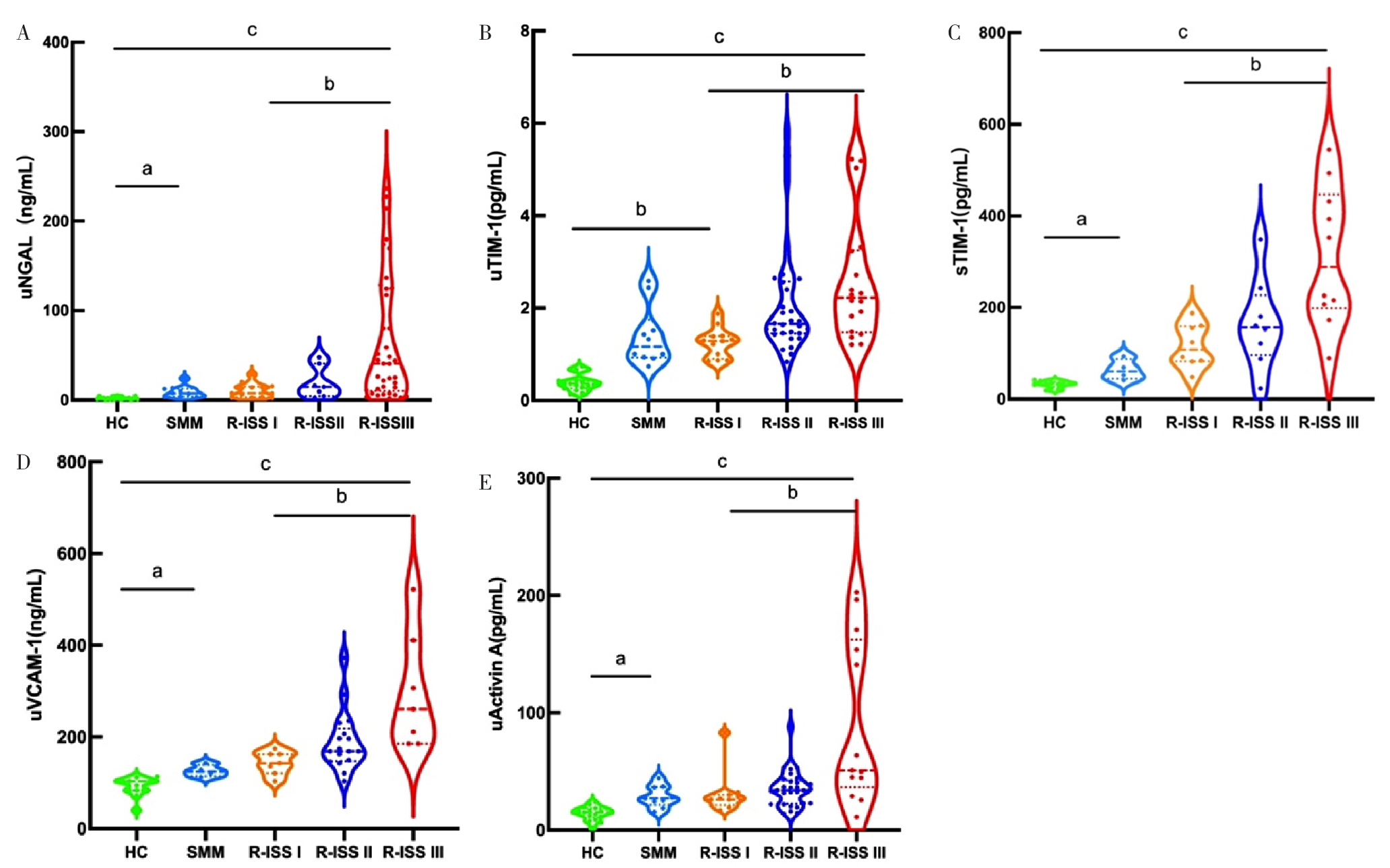
图2 随着MM病情演变各检测因子水平变化小提琴图注:MM=多发性骨髓瘤,SMM=冒烟型MM,R-ISS=修订的国际预后分期;A为uNGAL,B为uTIM-1,C为sTIM-1,D为uVCAM-1,E为尿液激活素A;a表示与SMM组比较P<0.05,b表示与R-ISS I期组比较P<0.05,c表示与HC组比较P<0.05。
Figure 2 Violin plot of changes in levels of each detected factors in MM disease evolution
| 组别 | 例数 | uNGAL | uTIM-1 |
|---|---|---|---|
| 治疗前MM亚组 | 20 | 46.2(117.0) | 2.0(1.1) |
| >PR亚组 | 20 | 7.5(29.9)a | 0.8(1.0)a |
| 复发MM亚组 | 11 | 26.8(72.6)b | 1.6(1.1)b |
| H值 | 3.920 | 3.771 | |
| P值 | <0.001 | 0.043 |
表6 治疗前MM亚组、>PR亚组、复发MM亚组uNGAL、uTIM-1水平比较[M(QR),ng/mL]
Table 6 Comparison of uNGAL and uTIM-1 detection levels in pre-treatment MM,>PR,and relapsed MM groups
| 组别 | 例数 | uNGAL | uTIM-1 |
|---|---|---|---|
| 治疗前MM亚组 | 20 | 46.2(117.0) | 2.0(1.1) |
| >PR亚组 | 20 | 7.5(29.9)a | 0.8(1.0)a |
| 复发MM亚组 | 11 | 26.8(72.6)b | 1.6(1.1)b |
| H值 | 3.920 | 3.771 | |
| P值 | <0.001 | 0.043 |
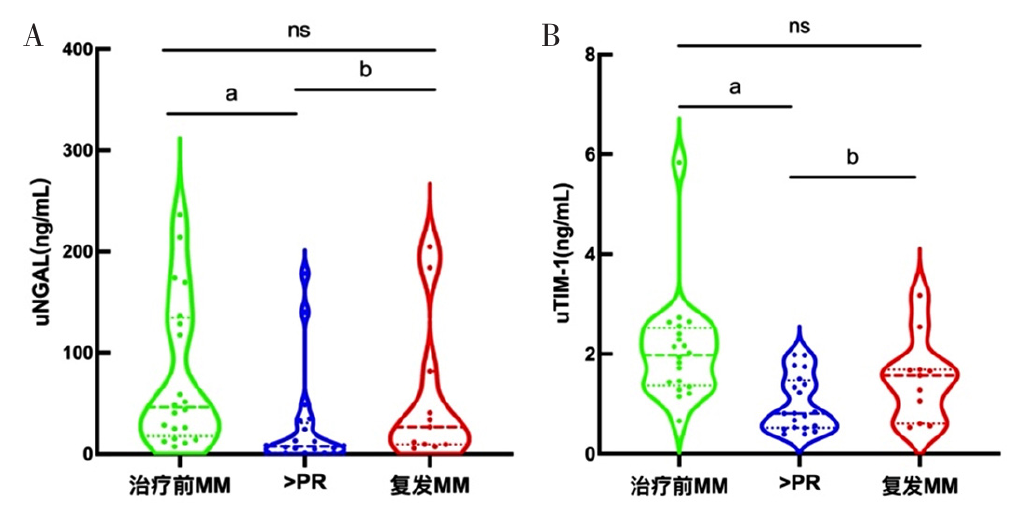
图3 治疗前MM亚组、>PR亚组、复发MM亚组uNGAL和uTIM-1水平变化小提琴图注:A为uNGAL,B为uTIM-1;ns表示P>0.05,a表示与治疗前MM亚组比较P<0.05,b表示与复发MM亚组比较P<0.05。
Figure 3 Violin plot of dynamic changes of uNGAL and uTIM-1 levels in pre-treatment MM group,> PR group and relapsed MM group
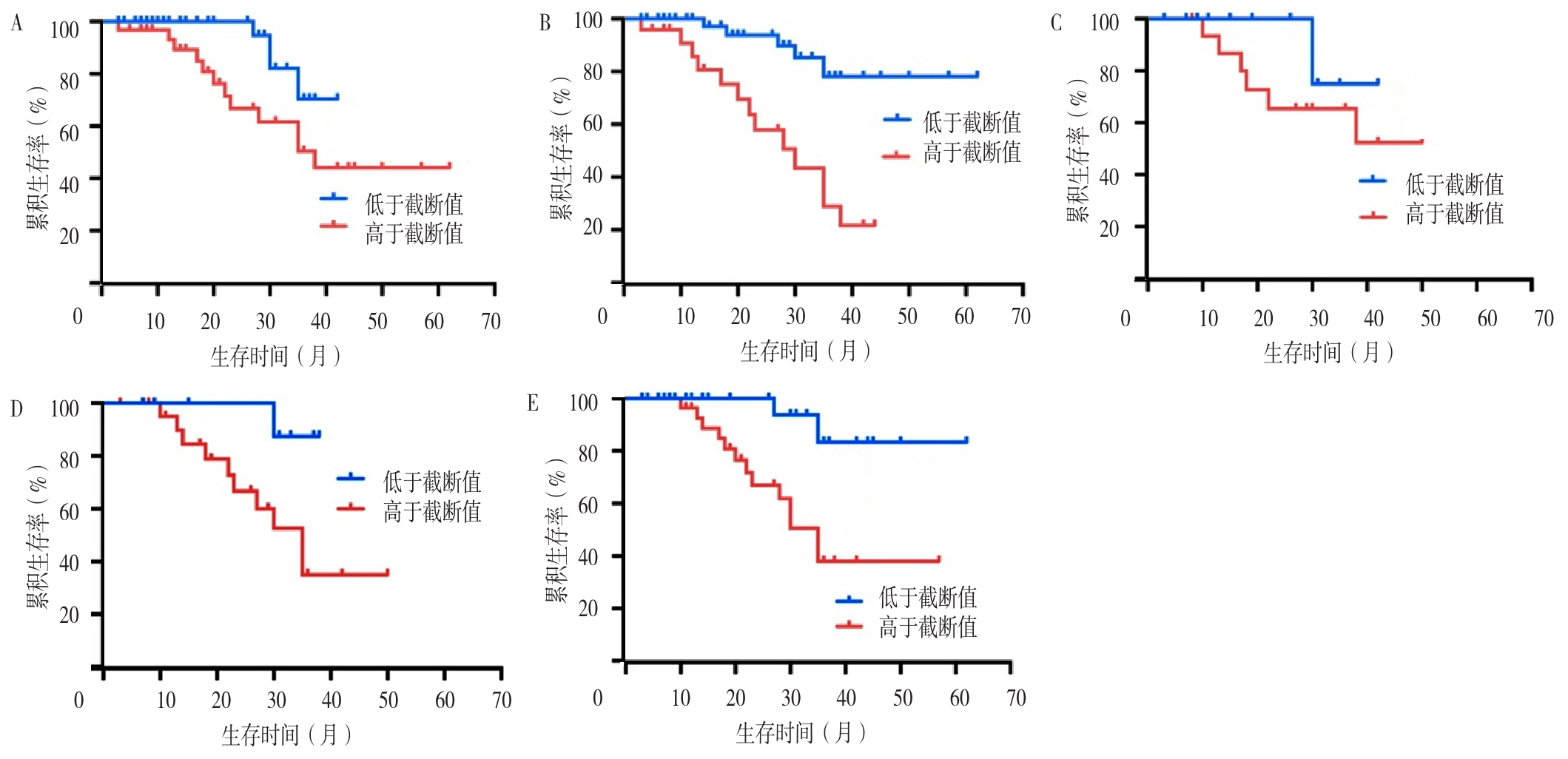
图5 不同检测因子水平患者的生存曲线注:A为uNGAL,B为uTIM-1,C为sTIM-1,D为uVCAM-1,E为尿激活素A。
Figure 5 Function graph of survival analysis of patients with different levels of tested factors
| 变量 | 单因素COX比例风险回归分析 | 多因素COX比例风险回归分析 | ||
|---|---|---|---|---|
| HR(95%CI) | P值 | HR(95%CI) | P值 | |
| 年龄 | 0.467(0.048~0.998) | 0.046 | 0.905(0.923~1.100) | 0.871 |
| R-ISS分期 | 0.865(0.984~7.290) | 0.003 | 0.820(1.378~8.290) | 0.008 |
| 血红蛋白 | 0.488(0.051~1.053) | 0.041 | 0.784(0.026~2.072) | 0.191 |
| 肌酐 | 0.481(0.038~1.027) | 0.043 | 1.412(0.011~1.957) | 0.962 |
| uNGAL | 0.589(0.766~2.021) | 0.032 | 0.261(0.046~1.013) | 0.049 |
| uTIM-1 | 0.452(0.046~0.975) | 0.048 | 1.022(0.199~1.705) | 0.325 |
| sTIM-1 | 0.524(0.736~1.575) | 0.039 | 0.761(0.212~1.825) | 0.342 |
| uVCAM-1 | 0.471(0.046~1.002) | 0.045 | 0.57(0.041~13.743) | 0.848 |
| 尿激活素A | 0.477(0.046~1.015) | 0.044 | 1.245(0.011~1.957) | 0.145 |
表7 NDMM合并KI患者全因死亡影响因素的COX比例风险回归分析
Table 7 Cox regression analysis of influencing factors of all-cause mortality in NDMM patients with KI
| 变量 | 单因素COX比例风险回归分析 | 多因素COX比例风险回归分析 | ||
|---|---|---|---|---|
| HR(95%CI) | P值 | HR(95%CI) | P值 | |
| 年龄 | 0.467(0.048~0.998) | 0.046 | 0.905(0.923~1.100) | 0.871 |
| R-ISS分期 | 0.865(0.984~7.290) | 0.003 | 0.820(1.378~8.290) | 0.008 |
| 血红蛋白 | 0.488(0.051~1.053) | 0.041 | 0.784(0.026~2.072) | 0.191 |
| 肌酐 | 0.481(0.038~1.027) | 0.043 | 1.412(0.011~1.957) | 0.962 |
| uNGAL | 0.589(0.766~2.021) | 0.032 | 0.261(0.046~1.013) | 0.049 |
| uTIM-1 | 0.452(0.046~0.975) | 0.048 | 1.022(0.199~1.705) | 0.325 |
| sTIM-1 | 0.524(0.736~1.575) | 0.039 | 0.761(0.212~1.825) | 0.342 |
| uVCAM-1 | 0.471(0.046~1.002) | 0.045 | 0.57(0.041~13.743) | 0.848 |
| 尿激活素A | 0.477(0.046~1.015) | 0.044 | 1.245(0.011~1.957) | 0.145 |
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
王岩,黄仲夏,胡婉莉,等. 血管细胞黏附分子-1和激活素A对多发性骨髓瘤的影响研究[J]. 中国全科医学,2021,24(17):2185-2191.
|
| [21] |
|
| [22] |
|
| [23] |
|
| [24] |
|
| [25] |
|
| [26] |
|
| [1] | 杨晨, 陈瞳, 张利方, 张洪旭, 李鹏飞, 张雪娟. 达格列净对老年乳腺癌幸存者射血分数保留的心力衰竭合并2型糖尿病患者的预后影响研究[J]. 中国全科医学, 2025, 28(24): 3053-3058. |
| [2] | 曹干, 邓毅凡, 何胜虎, 张晶. 乳酸脱氢酶与白蛋白比值与急性ST段抬高型心肌梗死急诊经皮冠状动脉介入治疗术后患者预后的相关性研究[J]. 中国全科医学, 2025, 28(15): 1878-1883. |
| [3] | 陈伊静, 许琪, 刘忠典, 覃玲巧, 陈淑萍, 唐薇婷, 钟秋安. 己糖胺生物合成通路在血管内皮炎症中的调控作用研究[J]. 中国全科医学, 2025, 28(15): 1871-1877. |
| [4] | 张树静, 孙立新, 曹雨晴. 人乳头瘤病毒相关宫颈腺癌与非人乳头瘤相关宫颈腺癌的临床病理特征比较及预后研究[J]. 中国全科医学, 2025, 28(14): 1758-1764. |
| [5] | 王德祥, 原佳雯, 陆沁云, 杭宇豪, 鲁俊, 程璐. 清肺化瘀通腑方治疗时机对脓毒症相关急性呼吸窘迫综合征治疗效果及预后的影响研究[J]. 中国全科医学, 2025, 28(12): 1500-1505. |
| [6] | 王晓雨, 冯贞贞, 王军, 郭小川, 李建生. 急性呼吸窘迫综合征患者并发急性肾损伤危险因素的系统评价[J]. 中国全科医学, 2025, 28(12): 1527-1537. |
| [7] | 李秋敬, 商娜, 高倩, 杨黎, 郭树彬. 基于腹部CT的骨骼肌量联合危重症评分对老年腹腔脓毒症患者预后的预测价值研究[J]. 中国全科医学, 2025, 28(12): 1459-1464. |
| [8] | 张沛, 杨萌, 高春林, 夏正坤. 加味升降散治疗儿童急性肾损伤和急性肾脏病效果和预后的影响研究[J]. 中国全科医学, 2025, 28(11): 1376-1382. |
| [9] | 王一荃, 陈万佳, 刘旺意, 张璐芸, 邓跃毅. 发酵虫草菌粉治疗慢性肾脏病4期患者的预后效果:基于回顾性队列研究[J]. 中国全科医学, 2025, 28(09): 1084-1091. |
| [10] | 杜慧杰, 刘星雨, 徐明欢, 杨学智, 张慧琴, 莫佳丽, 卢依, 况杰. 急性缺血性脑卒中预后预测研究的应用进展:以机器学习预测模型为例[J]. 中国全科医学, 2025, 28(05): 554-560. |
| [11] | 张萍淑, 薛晶, 邢爱君, 王连辉, 马倩, 符永山, 元小冬. 急性后循环缺血性脑卒中患者睡眠状态变化与预后影响因素的研究[J]. 中国全科医学, 2025, 28(05): 548-553. |
| [12] | 朱露, 艾军, 廖生武, 黄淑婷, 龚妮容, 孔耀中, 刘德慧, 窦献蕊, 张广清. 预后营养指数对腹膜透析患者心血管疾病死亡的影响:一项多中心回顾性队列研究[J]. 中国全科医学, 2025, 28(05): 568-574. |
| [13] | 张少通, 王博, 张明瑞, 马桂燕, 柳少光. 使用降钙素原轨迹识别脓毒症亚表型及风险分层研究[J]. 中国全科医学, 2025, 28(05): 594-600. |
| [14] | 王林娜, 张靖辉. 血清淀粉样蛋白A、白介素6、肿瘤坏死因子α及微小RNA在脓毒症并发急性肾损伤患儿中的表达及预后评估价值研究[J]. 中国全科医学, 2025, 28(03): 293-298. |
| [15] | 张连芳, 郑雅斌, 林雪烽, 谢榕城, 马杰飞. 未成熟血小板比率联合其他指标对脓毒症严重程度及其预后的预测价值研究[J]. 中国全科医学, 2024, 27(35): 4417-4425. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





