

Chinese General Practice ›› 2024, Vol. 27 ›› Issue (06): 685-691.DOI: 10.12114/j.issn.1007-9572.2022.0765
Special Issue: 高血压最新文章合辑
• Original Research • Previous Articles Next Articles
Received:2022-09-30
Revised:2022-12-26
Published:2024-02-20
Online:2023-11-21
Contact:
LIU Xiaohui
通讯作者:
刘小慧
作者简介:
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.chinagp.net/EN/10.12114/j.issn.1007-9572.2022.0765
| 公式名称 | 点尿钠测定样本类型 | 24 h尿钠排泄量估测公式 |
|---|---|---|
| Kawasaki | 清晨空腹第2次尿 | 24 h尿钠排泄量(mmol/d)=16.3×[点尿钠(mmol/L)/点尿肌酐(mg/L)×24 h尿肌酐(mg/d)]0.5 24 h尿肌酐(mg/d)(男)=15.12×体质量(kg)+7.39×身高(cm)-12.63×年龄-79.9 24 h尿肌酐(mg/d)(女)=8.58×体质量(kg)+5.09×身高(cm)-4.72×年龄-74.5 |
| INTERSALT | 随机尿 | 24 h尿钠排泄量(mmol/d)(男)=25.46+0.46×点尿钠(mmol/L)-2.75×点尿肌酐(mmol/L)-0.13×点尿钾(mmol/L)+4.1×BMI+0.26×年龄 24 h尿钠排泄量(mmol/d)(女)=5.07+0.34×点尿钠(mmol/L)-2.16×点尿肌酐(mmol/L)-0.09×点尿钾(mmol/L)+2.39×BMI+2.35×年龄-0.03×年龄2 |
| Tanaka | 随机尿 | 24 h尿钠排泄量(mmol/d)=21.98×[点尿钠(mmol/L)/点尿肌酐(mg/L)×24 h尿肌酐(mg/d)]0.392 24 h尿肌酐(mg/d)=14.89×体质量(kg)+16.14×身高(cm)-2.04×年龄-2 244.45 |
Table 1 Three equations using spot urine samples to estimate 24-hour urinary sodium excretion
| 公式名称 | 点尿钠测定样本类型 | 24 h尿钠排泄量估测公式 |
|---|---|---|
| Kawasaki | 清晨空腹第2次尿 | 24 h尿钠排泄量(mmol/d)=16.3×[点尿钠(mmol/L)/点尿肌酐(mg/L)×24 h尿肌酐(mg/d)]0.5 24 h尿肌酐(mg/d)(男)=15.12×体质量(kg)+7.39×身高(cm)-12.63×年龄-79.9 24 h尿肌酐(mg/d)(女)=8.58×体质量(kg)+5.09×身高(cm)-4.72×年龄-74.5 |
| INTERSALT | 随机尿 | 24 h尿钠排泄量(mmol/d)(男)=25.46+0.46×点尿钠(mmol/L)-2.75×点尿肌酐(mmol/L)-0.13×点尿钾(mmol/L)+4.1×BMI+0.26×年龄 24 h尿钠排泄量(mmol/d)(女)=5.07+0.34×点尿钠(mmol/L)-2.16×点尿肌酐(mmol/L)-0.09×点尿钾(mmol/L)+2.39×BMI+2.35×年龄-0.03×年龄2 |
| Tanaka | 随机尿 | 24 h尿钠排泄量(mmol/d)=21.98×[点尿钠(mmol/L)/点尿肌酐(mg/L)×24 h尿肌酐(mg/d)]0.392 24 h尿肌酐(mg/d)=14.89×体质量(kg)+16.14×身高(cm)-2.04×年龄-2 244.45 |
| 指标 | 女性患者(n=91) | 男性患者(n=105) | χ2(t)值 | P值 |
|---|---|---|---|---|
| 年龄(岁) | 63.0±12.1 | 52.3±14.7 | -5.875a | <0.001 |
| 体质指数(kg/m2) | 26.14±4.15 | 27.49±3.67 | 2.224a | 0.027 |
| 入院收缩压(mmHg) | 151±20 | 148±19 | -0.950a | 0.343 |
| 入院舒张压(mmHg) | 79±15 | 85±16 | 2.776a | 0.006 |
| 24 h平均收缩压(mmHg) | 130±18 | 130±17 | 0.044a | 0.965 |
| 24 h平均舒张压(mmHg) | 71±11 | 78±13 | 4.151a | <0.001 |
| 24 h平均心率(bpm) | 69±10 | 71±9 | 1.181a | 0.239 |
| 夜间血压下降异常[例(%)] | 65(72.2) | 65(63.1) | 1.815 | 0.178 |
| 糖尿病[例(%)] | 26(28.6) | 27(25.7) | 0.202 | 0.653 |
| 高脂血症[例(%)] | 65(71.4) | 69(65.7) | 0.736 | 0.391 |
| 左心室肥厚[例(%)] | 12(13.2) | 12(11.5) | 0.122 | 0.727 |
| 颈动脉内中膜增厚或斑块[例(%)] | 67(75.3) | 75(75.0) | 0.002 | 0.964 |
| 吸烟史[例(%)] | 1(1.1) | 59(56.2) | 69.657 | <0.001 |
| 微量蛋白尿[例(%)] | 28(31.1) | 19(18.1) | 4.488 | 0.034 |
| 临床蛋白尿[例(%)] | 8(8.8) | 2(1.9) | 4.775 | 0.047 |
| 点尿钠(mmol/L) | 101.35±49.49 | 134.44±56.54 | 4.350a | <0.001 |
| 实测24 h尿钠排泄量(mmol/d) | 134.86±62.90 | 193.11±82.00 | 5.458a | <0.001 |
Table 2 Baseline characteristics of enrolled patients with primary hypertension
| 指标 | 女性患者(n=91) | 男性患者(n=105) | χ2(t)值 | P值 |
|---|---|---|---|---|
| 年龄(岁) | 63.0±12.1 | 52.3±14.7 | -5.875a | <0.001 |
| 体质指数(kg/m2) | 26.14±4.15 | 27.49±3.67 | 2.224a | 0.027 |
| 入院收缩压(mmHg) | 151±20 | 148±19 | -0.950a | 0.343 |
| 入院舒张压(mmHg) | 79±15 | 85±16 | 2.776a | 0.006 |
| 24 h平均收缩压(mmHg) | 130±18 | 130±17 | 0.044a | 0.965 |
| 24 h平均舒张压(mmHg) | 71±11 | 78±13 | 4.151a | <0.001 |
| 24 h平均心率(bpm) | 69±10 | 71±9 | 1.181a | 0.239 |
| 夜间血压下降异常[例(%)] | 65(72.2) | 65(63.1) | 1.815 | 0.178 |
| 糖尿病[例(%)] | 26(28.6) | 27(25.7) | 0.202 | 0.653 |
| 高脂血症[例(%)] | 65(71.4) | 69(65.7) | 0.736 | 0.391 |
| 左心室肥厚[例(%)] | 12(13.2) | 12(11.5) | 0.122 | 0.727 |
| 颈动脉内中膜增厚或斑块[例(%)] | 67(75.3) | 75(75.0) | 0.002 | 0.964 |
| 吸烟史[例(%)] | 1(1.1) | 59(56.2) | 69.657 | <0.001 |
| 微量蛋白尿[例(%)] | 28(31.1) | 19(18.1) | 4.488 | 0.034 |
| 临床蛋白尿[例(%)] | 8(8.8) | 2(1.9) | 4.775 | 0.047 |
| 点尿钠(mmol/L) | 101.35±49.49 | 134.44±56.54 | 4.350a | <0.001 |
| 实测24 h尿钠排泄量(mmol/d) | 134.86±62.90 | 193.11±82.00 | 5.458a | <0.001 |
| 患者人群 | 例数 | 24 h尿钠排泄量实测值 | 24 h尿钠排泄量估测值 | t配对值 | P值 |
|---|---|---|---|---|---|
| 女性患者 | 91 | 134.86±62.90 | 194.97±64.55 | -8.786 | <0.001 |
| 男性患者 | 105 | 193.11±82.00 | 237.44±83.30 | -4.274 | <0.001 |
| 糖尿病患者 | 53 | 155.70±75.79 | 219.20±87.73 | -4.850 | <0.001 |
| 非糖尿病患者 | 143 | 168.62±79.77 | 217.03±74.33 | -6.401 | <0.001 |
| 白蛋白尿患者 | 57 | 152.12±73.94 | 235.92±100.39 | -5.926 | <0.001 |
| 无蛋白尿患者 | 139 | 169.15±80.23 | 211.96±69.18 | -5.879 | <0.001 |
| 钠盐摄入量 | |||||
| <6.0 g组 | 40 | 67.18±24.42 | 164.38±67.29 | -9.593 | <0.001 |
| 6.0~8.9 g组 | 51 | 127.33±14.17 | 207.76±75.02 | -7.526 | <0.001 |
| 9.0~11.9 g组 | 58 | 175.86±14.20 | 243.11±76.48 | -6.442 | <0.001 |
| ≥12 g组 | 47 | 276.39±49.53 | 242.73±67.03 | 2.659 | 0.011 |
Table 3 The difference and correlation between the estimated 24-hour urinary sodium excretion by Kawasaki equation and the measured value
| 患者人群 | 例数 | 24 h尿钠排泄量实测值 | 24 h尿钠排泄量估测值 | t配对值 | P值 |
|---|---|---|---|---|---|
| 女性患者 | 91 | 134.86±62.90 | 194.97±64.55 | -8.786 | <0.001 |
| 男性患者 | 105 | 193.11±82.00 | 237.44±83.30 | -4.274 | <0.001 |
| 糖尿病患者 | 53 | 155.70±75.79 | 219.20±87.73 | -4.850 | <0.001 |
| 非糖尿病患者 | 143 | 168.62±79.77 | 217.03±74.33 | -6.401 | <0.001 |
| 白蛋白尿患者 | 57 | 152.12±73.94 | 235.92±100.39 | -5.926 | <0.001 |
| 无蛋白尿患者 | 139 | 169.15±80.23 | 211.96±69.18 | -5.879 | <0.001 |
| 钠盐摄入量 | |||||
| <6.0 g组 | 40 | 67.18±24.42 | 164.38±67.29 | -9.593 | <0.001 |
| 6.0~8.9 g组 | 51 | 127.33±14.17 | 207.76±75.02 | -7.526 | <0.001 |
| 9.0~11.9 g组 | 58 | 175.86±14.20 | 243.11±76.48 | -6.442 | <0.001 |
| ≥12 g组 | 47 | 276.39±49.53 | 242.73±67.03 | 2.659 | 0.011 |
| 患者人群 | rs值 | P值 |
|---|---|---|
| 女性患者 | 0.472 | <0.001 |
| 男性患者 | 0.195 | 0.047 |
| 糖尿病患者 | 0.425 | 0.002 |
| 非糖尿病患者 | 0.386 | <0.001 |
| 白蛋白尿患者 | 0.409 | 0.005 |
| 无蛋白尿患者 | 0.401 | <0.001 |
| 钠盐摄入量 | ||
| <6.0 g组 | 0.319 | 0.045 |
| 6.0~8.9 g组 | -0.016 | 0.913 |
| 9.0~11.9 g组 | 0.014 | 0.915 |
| ≥12 g组 | <0.001 | 0.999 |
Table 4 Correlation analysis between estimated 24-hour sodium excretion by Kawasaki equation and measured 24-hour sodium excretion
| 患者人群 | rs值 | P值 |
|---|---|---|
| 女性患者 | 0.472 | <0.001 |
| 男性患者 | 0.195 | 0.047 |
| 糖尿病患者 | 0.425 | 0.002 |
| 非糖尿病患者 | 0.386 | <0.001 |
| 白蛋白尿患者 | 0.409 | 0.005 |
| 无蛋白尿患者 | 0.401 | <0.001 |
| 钠盐摄入量 | ||
| <6.0 g组 | 0.319 | 0.045 |
| 6.0~8.9 g组 | -0.016 | 0.913 |
| 9.0~11.9 g组 | 0.014 | 0.915 |
| ≥12 g组 | <0.001 | 0.999 |
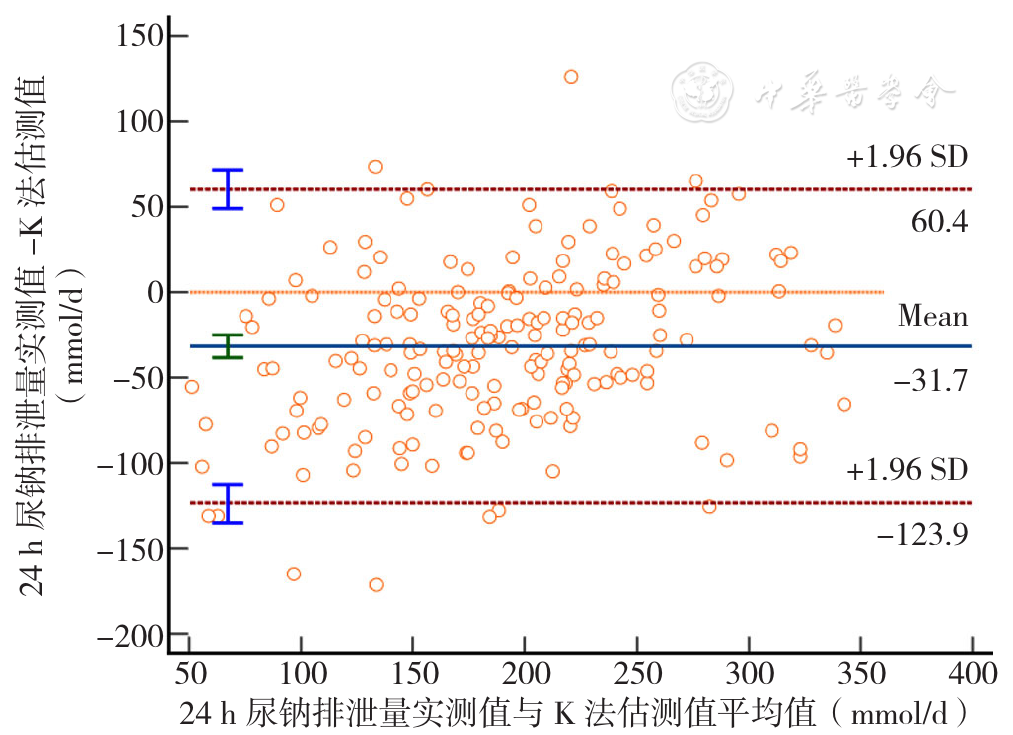
Figure 1 The consistency of measured 24-hour urine sodium excretion and estimated 24-hour urine sodium excretion by Kawasaki equation evaluated by the Bland-Altman plot
| 患者人群 | 例数 | 24 h尿钠排泄量实测值 | 24 h尿钠排泄量估测值 | t配对值 | P值 |
|---|---|---|---|---|---|
| 女性患者 | 91 | 134.86±62.90 | 107.69±26.42 | 4.678 | <0.001 |
| 男性患者 | 105 | 193.11±82.00 | 174.89±33.58 | 2.008 | 0.047 |
| 糖尿病患者 | 53 | 155.70±75.79 | 139.43±48.83 | 1.651 | 0.105 |
| 非糖尿病患者 | 143 | 168.62±79.77 | 145.26±44.00 | 3.864 | <0.001 |
| 白蛋白尿患者 | 57 | 152.12±73.94 | 140.23±46.24 | 1.179 | 0.244 |
| 无蛋白尿患者 | 139 | 169.15±80.23 | 145.15±45.02 | 4.018 | <0.001 |
| 钠盐摄入量 | |||||
| <6.0 g组 | 40 | 67.18±24.42 | 113.23±40.86 | -6.751 | <0.001 |
| 6.0~8.9 g组 | 51 | 127.33±14.17 | 129.36±43.35 | -0.322 | 0.749 |
| 9.0~11.9 g组 | 58 | 175.86±14.20 | 155.47±43.61 | 3.311 | 0.002 |
| ≥12 g组 | 47 | 276.39±49.53 | 170.61±30.58 | 12.260 | <0.001 |
Table 5 The difference and correlation between the estimated 24-hour urinary sodium excretion by INTERSALT equation and the measured value
| 患者人群 | 例数 | 24 h尿钠排泄量实测值 | 24 h尿钠排泄量估测值 | t配对值 | P值 |
|---|---|---|---|---|---|
| 女性患者 | 91 | 134.86±62.90 | 107.69±26.42 | 4.678 | <0.001 |
| 男性患者 | 105 | 193.11±82.00 | 174.89±33.58 | 2.008 | 0.047 |
| 糖尿病患者 | 53 | 155.70±75.79 | 139.43±48.83 | 1.651 | 0.105 |
| 非糖尿病患者 | 143 | 168.62±79.77 | 145.26±44.00 | 3.864 | <0.001 |
| 白蛋白尿患者 | 57 | 152.12±73.94 | 140.23±46.24 | 1.179 | 0.244 |
| 无蛋白尿患者 | 139 | 169.15±80.23 | 145.15±45.02 | 4.018 | <0.001 |
| 钠盐摄入量 | |||||
| <6.0 g组 | 40 | 67.18±24.42 | 113.23±40.86 | -6.751 | <0.001 |
| 6.0~8.9 g组 | 51 | 127.33±14.17 | 129.36±43.35 | -0.322 | 0.749 |
| 9.0~11.9 g组 | 58 | 175.86±14.20 | 155.47±43.61 | 3.311 | 0.002 |
| ≥12 g组 | 47 | 276.39±49.53 | 170.61±30.58 | 12.260 | <0.001 |
| 患者人群 | rs值 | P值 |
|---|---|---|
| 女性患者 | 0.449 | <0.001 |
| 男性患者 | 0.124 | 0.209 |
| 糖尿病患者 | 0.415 | <0.001 |
| 非糖尿病患者 | 0.472 | <0.001 |
| 白蛋白尿患者 | 0.392 | 0.006 |
| 无蛋白尿患者 | 0.466 | <0.001 |
| 钠盐摄入量 | ||
| <6.0 g组 | 0.085 | 0.600 |
| 6.0~8.9 g组 | 0.006 | 0.965 |
| 9.0~11.9 g组 | -0.012 | 0.931 |
| ≥12 g组 | -0.088 | 0.555 |
Table 6 Correlation analysis between estimated 24-hour sodium excretion by INTERSALT equation and measured 24-hour sodium excretion
| 患者人群 | rs值 | P值 |
|---|---|---|
| 女性患者 | 0.449 | <0.001 |
| 男性患者 | 0.124 | 0.209 |
| 糖尿病患者 | 0.415 | <0.001 |
| 非糖尿病患者 | 0.472 | <0.001 |
| 白蛋白尿患者 | 0.392 | 0.006 |
| 无蛋白尿患者 | 0.466 | <0.001 |
| 钠盐摄入量 | ||
| <6.0 g组 | 0.085 | 0.600 |
| 6.0~8.9 g组 | 0.006 | 0.965 |
| 9.0~11.9 g组 | -0.012 | 0.931 |
| ≥12 g组 | -0.088 | 0.555 |
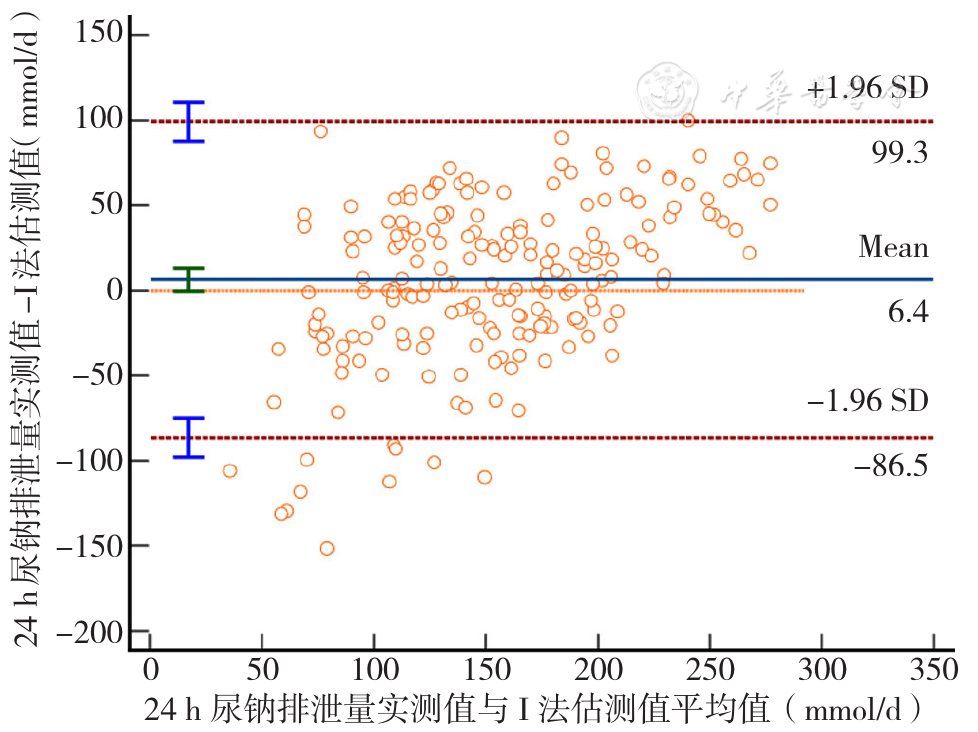
Figure 2 The consistency of measured 24-hour urine sodium excretion and estimated 24-hour urine sodium excretion by INTERSALT equation evaluated by the Bland-Altman plot
| 患者人群 | 例数 | 24 h尿钠排泄量实测值 | 24 h尿钠排泄量估测值 | t配对值 | P值 |
|---|---|---|---|---|---|
| 女性患者 | 91 | 134.86±62.90 | 161.87±44.05 | -4.524 | <0.001 |
| 男性患者 | 105 | 193.11±82.00 | 173.81±49.54 | 1.992 | 0.049 |
| 糖尿病患者 | 53 | 155.70±75.79 | 170.19±54.05 | -1.336 | 0.187 |
| 非糖尿病患者 | 143 | 168.62±79.77 | 167.51±44.74 | 0.164 | 0.870 |
| 白蛋白尿患者 | 57 | 152.12±73.94 | 181.17±60.37 | -2.696 | 0.010 |
| 无蛋白尿患者 | 139 | 169.15±80.23 | 164.15±42.06 | 0.752 | 0.453 |
| 钠盐摄入量 | |||||
| <6.0 g组 | 40 | 67.18±24.42 | 137.89±44.70 | -10.347 | <0.001 |
| 6.0~8.9 g组 | 51 | 127.33±14.17 | 163.10±46.11 | -5.281 | <0.001 |
| 9.0~11.9 g组 | 58 | 175.86±14.20 | 185.03±44.83 | -1.438 | 0.156 |
| ≥12 g组 | 47 | 276.39±49.53 | 179.30±41.07 | 9.808 | <0.001 |
Table 7 The difference and correlation between the estimated 24-hour urinary sodium excretion by Tanaka equation and the measured value
| 患者人群 | 例数 | 24 h尿钠排泄量实测值 | 24 h尿钠排泄量估测值 | t配对值 | P值 |
|---|---|---|---|---|---|
| 女性患者 | 91 | 134.86±62.90 | 161.87±44.05 | -4.524 | <0.001 |
| 男性患者 | 105 | 193.11±82.00 | 173.81±49.54 | 1.992 | 0.049 |
| 糖尿病患者 | 53 | 155.70±75.79 | 170.19±54.05 | -1.336 | 0.187 |
| 非糖尿病患者 | 143 | 168.62±79.77 | 167.51±44.74 | 0.164 | 0.870 |
| 白蛋白尿患者 | 57 | 152.12±73.94 | 181.17±60.37 | -2.696 | 0.010 |
| 无蛋白尿患者 | 139 | 169.15±80.23 | 164.15±42.06 | 0.752 | 0.453 |
| 钠盐摄入量 | |||||
| <6.0 g组 | 40 | 67.18±24.42 | 137.89±44.70 | -10.347 | <0.001 |
| 6.0~8.9 g组 | 51 | 127.33±14.17 | 163.10±46.11 | -5.281 | <0.001 |
| 9.0~11.9 g组 | 58 | 175.86±14.20 | 185.03±44.83 | -1.438 | 0.156 |
| ≥12 g组 | 47 | 276.39±49.53 | 179.30±41.07 | 9.808 | <0.001 |
| 患者人群 | rs值 | P值 |
|---|---|---|
| 女性患者 | 0.459 | <0.001 |
| 男性患者 | 0.165 | 0.093 |
| 糖尿病患者 | 0.377 | 0.005 |
| 非糖尿病患者 | 0.318 | <0.001 |
| 白蛋白尿患者 | 0.410 | 0.005 |
| 无蛋白尿患者 | 0.331 | <0.001 |
| 钠盐摄入量 | ||
| <6.0 g组 | 0.297 | 0.063 |
| 6.0~8.9 g组 | -0.038 | 0.791 |
| 9.0~11.9 g组 | -0.022 | 0.874 |
| ≥12.0 g组 | -0.060 | 0.691 |
Table 8 Correlation analysis between estimated 24-hour sodium excretion by Tanaka equation and measured 24-hour sodium excretion
| 患者人群 | rs值 | P值 |
|---|---|---|
| 女性患者 | 0.459 | <0.001 |
| 男性患者 | 0.165 | 0.093 |
| 糖尿病患者 | 0.377 | 0.005 |
| 非糖尿病患者 | 0.318 | <0.001 |
| 白蛋白尿患者 | 0.410 | 0.005 |
| 无蛋白尿患者 | 0.331 | <0.001 |
| 钠盐摄入量 | ||
| <6.0 g组 | 0.297 | 0.063 |
| 6.0~8.9 g组 | -0.038 | 0.791 |
| 9.0~11.9 g组 | -0.022 | 0.874 |
| ≥12.0 g组 | -0.060 | 0.691 |
| 钠盐摄入量 | 例数 | K法24 h尿钠排泄量估测值的相对偏差 | I法24 h尿钠排泄量估测值的相对偏差 | T法24 h尿钠排泄量估测值的相对偏差 |
|---|---|---|---|---|
| <6.0 g组 | 40 | -144.69 | -68.54 | -105.25 |
| 6.0~8.9 g组 | 51 | -63.17 | -1.59 | -28.09 |
| 9.0~11.9 g组 | 58 | -38.23 | 11.37 | -5.21 |
| ≥12 g组 | 47 | 12.18 | 38.27 | 35.13 |
Table 9 The relative difference between the estimated 24-hour sodium excretion by three estimation methods and the measured 24-hour sodium excretion
| 钠盐摄入量 | 例数 | K法24 h尿钠排泄量估测值的相对偏差 | I法24 h尿钠排泄量估测值的相对偏差 | T法24 h尿钠排泄量估测值的相对偏差 |
|---|---|---|---|---|
| <6.0 g组 | 40 | -144.69 | -68.54 | -105.25 |
| 6.0~8.9 g组 | 51 | -63.17 | -1.59 | -28.09 |
| 9.0~11.9 g组 | 58 | -38.23 | 11.37 | -5.21 |
| ≥12 g组 | 47 | 12.18 | 38.27 | 35.13 |
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
杜晓甫,陈向宇,张洁,等. 三种点尿法估算中国人群24 h尿钠排泄量的可行性评价[J]. 中华预防医学杂志,2020,54(4):420-424. DOI:10.3760/cma.j.cn112150-20190610-00458.
|
| [14] |
|
| [15] |
|
| [16] |
国家卫生健康委员会. 中国居民营养与慢性病状况报告-2020年[M]. 北京:人民卫生出版社,2021.
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [21] |
|
| [22] |
姜薇,张俊仕,帕提古丽,等. 点尿法及24h尿收集法估算高血压病患者24 h尿钠钾排泄量的应用比较[J]. 中华诊断学电子杂志,2019,7(1):21-25. DOI:10.3877/cma.j.issn.2095-655X.2019.01.005.
|
| [23] |
|
| [24] |
|
| [1] | LI Hao, LI Peijin, LIU Tingting, CUI Yiyuan, LI Sicong, LIU Lixing, FENG Li, Working Group on Integrated Traditional Chinese and Western Medicine Diagnosis and Treatment Guidelines for Cancer Pain. Guidelines on the Diagnosis and Treatment of Cancer Pain by Integrated Traditional Chinese and Western Medicine [J]. Chinese General Practice, 2025, 28(30): 3729-3740. |
| [2] | ZHI Congcong, LI Xue, CHENG Yicheng, WANG Xiaolong, ZHENG Lihua. Guidelines for Integrated Traditional Chinese and Western Medicine Diagnosis and Treatment of Hemorrhoids (2025 Edition) [J]. Chinese General Practice, 2025, 28(26): 3217-3228. |
| [3] | PAN Qi, REN Jingjing, MA Fanghui, HU Mengjie. Survey of General Practitioners' Cognition and Needs for AI Assisted Diagnosis and Treatment Systems [J]. Chinese General Practice, 2025, 28(25): 3127-3136. |
| [4] | Chinese Geriatrics Society, General Practice Branch of Zhejiang Medical Association, the Expert Collaboration Group on Medically Unspecified Disease in General Practice. Expert Consensus on the Diagnosis, Treatment, and Management of Emaciation (2025) [J]. Chinese General Practice, 2025, 28(21): 2577-2594. |
| [5] | LIU Hongya, YU Dehua. Construction and Practice of Clinical Diagnosis and Treatment Technology Combining General Practice and Specialist in Shanghai Community [J]. Chinese General Practice, 2025, 28(19): 2390-2397. |
| [6] | BIAN Ying, YIN Gang, ZHANG Zixun, TAO Hongbing. The Mechanism of Information Construction Enabling High-quality Development of Compact County-level Medical Consortium [J]. Chinese General Practice, 2025, 28(19): 2426-2432. |
| [7] | LYU Lulu, ZHU Wanjie, XIAO Mingyang, LI Yike, ZHANG Juan. Correlation Analysis of the Circadian Rhythmicity of Blood Pressure with Ox-LDL/β2GPI Complex and Carotid Atherosclerosis in Patients with Essential Hypertension [J]. Chinese General Practice, 2025, 28(18): 2228-2233. |
| [8] | DENG Yaqian, CAO Chunli, MA Jinmei, LI Wenxiao, XU Zelin, CHENG Jing, LI Jun. Predictive Value of S-Detect Combined with Virtual Touch Tissue Imaging Quantification in Axillary Lymph Node Metastasis of Breast Cancer [J]. Chinese General Practice, 2025, 28(17): 2149-2155. |
| [9] | LI Jie, DU Yue, SHAO Shen, PAN Dong, ZHANG Yaxin. The Operational Efficiency of Traditional Chinese Medicine Diagnosis and Treatment Services in Primary Medical Institutions in Tianjin Based on DEA and SFA [J]. Chinese General Practice, 2025, 28(16): 1980-1986. |
| [10] | GU Jie, HUANG Yanyan. Diagnosis and Comprehensive Management of Rare Diseases: the Indispensable Role of General Practitioners [J]. Chinese General Practice, 2025, 28(16): 1955-1960. |
| [11] | Chinese Academy Society of Sleep Medicine, Chinese Medical Doctor Association, Sleep Medicine Group, China Neurologist Association. Chinese Guideline for Diagnosis and Treatment of Co-morbid Insomnia and Obstructive Sleep Apnea (2024) [J]. Chinese General Practice, 2025, 28(11): 1289-1303. |
| [12] | HUANG Lujie, ZHANG Xiaoying, YU Shasha. Risk Factors, Prognosis and Rapid Screening in Patients with Acute Aortic Dissection Complicated with Type 2 Diabetes [J]. Chinese General Practice, 2025, 28(09): 1100-1105. |
| [13] | MA Xiaoxuan, WANG Rongqi. Research Progress in Metabolomics for HCC Diagnosis and Treatment [J]. Chinese General Practice, 2025, 28(08): 1017-1022. |
| [14] | MA Hongyang, YUE Anna, SUN Kangyun. Familial Hypercholesterolemia: Diagnostic Differences between Domestic and Foreign Guidelines [J]. Chinese General Practice, 2025, 28(06): 655-665. |
| [15] | DAI Yao, XUE Liping, ZHANG Shiqi, XU Min, ZHANG Qiu, HU Honglin. Congential Adrenal Hyperplasia Associated with CYP17A1 Gene Mutation: a Case Report and Literature Review [J]. Chinese General Practice, 2025, 28(06): 771-776. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||